Bedsores are a serious complication of many diseases associated with tissue malnutrition or resulting from external compression with displacement. In medical practice, bedsores are often called ulcers.
This complication is by no means the fate of only bedridden patients; bedsores can form under any external pressure, especially often at the sites of bone protrusions.
Bedsores affect patients suffering from impaired tissue innervation due to pathology or damage to the spinal cord. In such patients, treatment of bedsores on the heels and buttocks becomes relevant, i.e. places receiving the greatest pressure from body weight.
In bedridden patients, compression of the skin and blood vessels occurs, resulting in stagnant processes and tissue death in places of maximum contact of the body with the hard parts of the bed, therefore bedsores are formed depending on the position of the body:
- When lying on your stomach, the pubis and cheekbones are affected
- When lying on the side - knees, hips, ankles
- Lying on your back – sacrum, heels, ischial tuberosity, elbows, shoulder blades, back of head
This process is facilitated by overdrying or, conversely, excessive moisturizing of the skin. Dryness leads to exfoliation of the stratum corneum (protective) layer of the skin, and humidity provokes infection of the affected areas, all this is aggravated by impaired blood supply to areas of compression.
Such a complication as bedsores, their prevention and treatment are relevant to this day - the search for the latest means of treating and preventing these formations is constantly underway. Bedsores form quite quickly, but their treatment is problematic and does not always bring the desired effect.
70% of patients who develop bedsores are elderly:
- 66% - older people with hip (femoral neck) fractures
- 60% - patients with tetraplegia
- 33% patients in intensive care units
- 9% of hospitalized patients
- 3-25% - people at home (bedridden patients)
Causes of bedsores formation
Bedsores develop as a result of the pressure of hard surfaces on which bedridden patients are located on their protruding areas of the body with a slight muscle and fat layer, most often on the shoulder blades, thoracic spine, sacrum, heels, back of the head, etc. In patients forced to sit for a long time, bedsores form on the back, sacrum, heels, fingers, feet and shoulder blades.
Tissue damage is caused by the following reasons:
- bending of blood vessels that deliver oxygen and nutritional components to muscle and skin cells. Due to oxygen starvation (hypoxia) and insufficient nutrition, the vital activity of cells is inhibited, which leads to their death;
- compression of nerve fibers responsible for regulating metabolism in tissues, as a result of which cell viability deteriorates;
- compression of the lymphatic vessels, which remove waste products of cells from the intercellular space, resulting in the accumulation of waste and toxins in it, a decrease in the viability of cells, their poisoning and death. In addition, one of the functions of the lymphatic system is the disposal of dead cells: compressed lymphatic vessels lead to the accumulation of dead cells in tissues, which favors the development of infection.
In addition, the development of bedsores is associated with friction, which causes mechanical damage and desquamation of skin cells, displacement of deep-lying tissues and rupture of blood vessels.
Increased humidity increases the likelihood of developing bedsores, causing the skin to swell and increase friction. There is a particularly high risk of developing bedsores in patients suffering from urinary and fecal incontinence, which contain substances that cause skin irritation.
What medications are used
The choice of treatment for pressure sores on the tailbone varies depending on the extent of the lesion and the severity of the disease. The doctor may recommend antiseptics, wound healing agents, and drugs that improve blood circulation. Chlorhexidine or another antiseptic solution is used to treat the skin, but not in every case it is possible to treat an open wound.
The classic approach to treatment includes several stages:
- Disinfection and cleaning of tissues in and around the damaged area.
- Applying a special cream or ointment dressing that promotes the rejection of dead cells.
- The use of agents that prevent bacterial infection (antiseptic dressings, etc.).
- If a bacterial infection is detected, the doctor will prescribe antibiotics. For inflammation - anti-inflammatory drugs. For pain - analgesics.
- Application of wound healing agents in the form of ointment dressings and creams.
It is not recommended to treat bedsores on the buttocks without consulting a doctor.
Complications of bedsores
Bedsores left without proper attention can significantly worsen the patient's condition and lead to the development of severe consequences. In most cases, the disease can be complicated by the following pathologies:
- sepsis;
- phlegmon;
- osteomyelitis;
- purulent arthritis;
- wound myiasis (can develop in warm seasons, when insects actively reproduce and lay their larvae in wounds);
- arosive bleeding;
- skin cancer
Timely therapy and proper patient care by highly qualified medical personnel at the Yusupov Hospital, who know how to cure bedsores, ensure the prevention of the development of such complications.
Tests and diagnostics
The doctor makes a diagnosis based on the symptoms that the patient has. A purulent surgeon, traumatologist or other specialist conducts an external examination of the patient, interviewing him or relatives caring for the patient. A smear from the wound and a laboratory blood test are also taken and laboratory tested. No special diagnostic methods are required. In some cases, a differential diagnosis of a bedsore with skin cancer is carried out; a biopsy .
Bedsores: treatment at home with onion composition
If the patient has redness of the skin, you can prepare an onion mixture, which, in addition to onions, includes olive oil and candle wax.
Well-chopped onions (two medium-sized heads) are mixed with two tablespoons of olive oil, after which the resulting pulp must be heated in a water bath for about 20 minutes. Then strain the mixture through cheesecloth, add wax from a melted church candle, and let cool. Apply the resulting ointment to the reddened area of the skin twice a day (in the morning and before bed). Thanks to gentle warming, patients experience no discomfort, blood flow is activated, which has a positive effect on the regeneration process.
In addition, this product has a disinfectant effect, preventing infection of bedsores in the presence of microcracks on the surface of damaged skin.
Diet
Diet for skin diseases
- Efficacy: therapeutic effect after a month
- Time frame: three months or more
- Cost of products: 1400-1500 rubles per week
To prevent the occurrence of such lesions, it is important to introduce a sufficient amount of protein products into the patient’s diet. You should choose dietary, low-fat foods - milk, eggs, lean meat, fish. You should also introduce into the diet foods containing vitamins A , C , and group B. It is recommended that such patients prepare dishes from the liver, heart, rice, and buckwheat.
It is imperative to plan the patient’s diet - he should receive food in small portions 4-6 times a day. Drinking regimen is also important - the patient needs to drink enough liquid.
Dry bedsores: treatment with ammonia
One of the ways to treat bedsores at home is ammonia. To prevent the worsening of bedsores and the progression of the disease to a more severe stage, the reddened area of the skin should be thoroughly wiped with ammonia. Before treating bedsores in bedridden patients with ammonia, the skin must be thoroughly treated. Already on the third or fourth day of such treatment, the redness disappears, the skin is completely restored, since it is quite simple to quickly cure bedsores in the early stages, not accompanied by a necrotic process.
List of sources
- Vorobyov A.A., Tsurikov Yu.M., Poroisky S.V. Treatment of bedsores in spinal patients // Bulletin of the Volgograd Scientific Center of the Russian Academy of Medical Sciences. - 2007.- No. 2. - pp. 33-34.
- Klimiashvili A.D. Prevention and treatment of bedsores. // Russian medical journal. - 2004. - T. 12, No. 12. — P. 40-45.
- Paukov V.S., Musalatov H.A., Saltykov B.B., Shashlov S.V. Ermakova N.G., Elizarov M.N. Immunomorphological characteristics of bedsores // Pathology Archives. 1997. - No. 6. — p.40-44.
- Prevention and treatment of bedsores. Association of General Practitioners (Family Doctors). - M., 2004. - P. 44-64.
Can bedsores be cured by other means?
At the first signs of the development of bedsores, the following composition is used: add one tablespoon of vinegar (9%) to boiled water (250 ml). It is necessary to treat the affected area with the resulting solution every hour during the day, taking a break at night. Redness disappears, as a rule, on the 4-5th day of treatment.
Lilac leaves have excellent effectiveness in the early stages of the disease. A compress of mashed fresh leaves should be applied to the reddened area of skin, and then secure it with a band-aid. After three hours, remove the compress and apply a new one. Continue the course of treatment for at least five days.
Rules of care
What to do if bedsores begin is a common question for relatives faced with such a situation. In addition to medications, it is necessary to follow the following rules of care:
- Keep the skin clean, let the patient take air baths more often.
- Wipe oily skin with products containing alcohol, dry skin - moisturize with baby cream.
- If the area of the epidermis is red, massage around it, increasing blood circulation.
- For incontinence, use diapers and powder underneath.
- Eliminate the consequences of excessive sweating with a solution of table vinegar.
- Turn the patient over every 2 hours.
- Ventilate the room and monitor the air temperature.
Daily care, medications and vitamins will help strengthen the immune system, improve blood circulation, and restore tissue trophism at the initial stage of the disease.
Treating bedsores at home with baking soda solution
Purulent bedsores can be treated with regular baking soda. Add 1 teaspoon of soda to boiling water (250 ml), cool the solution. Soak a piece of linen cloth in the solution, squeeze it out a little and apply it to the affected area of the skin. This remedy promotes the active discharge of purulent contents of bedsores, which remains on the napkin. The napkin should remain on the wound for at least 10 minutes. During one procedure you need to change three napkins. Four procedures must be performed per day. Continue treatment for five to ten days until the wound is completely healed.
Classification
There are four stages of pressure ulcers according to their severity:
- The first stage - the skin remains intact. There is redness in the affected areas, and when you touch them, the skin does not become light. If you compare these areas with healthy ones, the skin on them is harder and more sensitive. Its temperature also differs - it is hotter or colder.
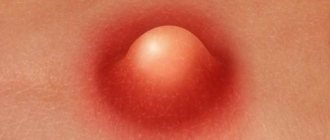
- The second stage – damage to the outer layer of the skin and dermis (the layer located under the outer layer) develops. At this stage, the wound is still shallow and pink or red. A fluid-filled blister may also appear, which then bursts.
- The third stage - a deep wound is formed on the affected area, in which subcutaneous fatty tissue is visible. The ulcer looks like a crater, with dead yellow tissue at the bottom. The pathological process spreads to adjacent areas of the skin.
- Stage four – massive tissue damage is noted. The wound becomes so large that it can reach muscles, tendons and even bone. The bottom of the wound is covered with a crust, it is yellow or dark in color.
Pressure ulcers of the third and fourth degree can only be treated surgically.
Bedsores are also classified based on the size of the resulting lesions:
- Small - up to 5 cm in diameter.
- Large – 10-15 cm.
- Giant - more than 15 cm.
Separately, there is a fistula form , when a large cavity is formed in the soft tissues, communicating with the external environment through an opening in the skin. The cavity may be located at a relatively large distance from the wound. osteomyelitis often develops .
Prevention of the development of bedsores at the Yusupov Hospital
Thanks to the professional approach, extensive experience and high qualifications of the specialists at the Yusupov Hospital, the development of bedsores in patients forced to be immobilized (during the rehabilitation period) is practically excluded.
For bedridden patients in the Yusupov Hospital, special orthopedic mattresses are provided that provide passive body massage and contribute to the correct distribution of the patient’s weight, hygiene procedures are regularly carried out, bed linen is changed, and nutritious meals are provided.
Thanks to all these services, as well as the professionalism and attentive attitude of the medical staff to each patient, the risk of developing bedsores in bedridden patients is minimized.
You can ask questions about the conditions of hospitalization and find out the cost of medical services by calling the Yusupov Hospital or on the clinic’s website, from the coordinating doctors.
Surgical method
If the disease is advanced before deep bedsores appear on the sacrum, then the surgeon removes the pus and dead cells. After the operation, the doctor prescribes:
- antibacterial drugs;
- means to improve blood circulation;
- wound healing dressings and ointments;
- anti-inflammatory drugs;
- minerals and vitamins for poor nutrition;
- immunomodulators.
When a patient has very deep bedsores on the sacrum, treatment may include transplanting one's own skin from healthy areas to damaged ones.
Proper care for a patient with bedsores can be provided with PAUL HARTMANN dressings. In case of severe exudation, it is recommended to use Sorbalgon and Molikar Skin care products. After cleaning the wound, a Hydrocoll dressing is added to provide a normal environment for wound granulation. Before using ointments, bandages and other products, you must consult a doctor.