Radiculitis is a complex of pain and neurological symptoms that occur when the nerve endings of the spinal nerves (paired nerve trunks corresponding to segments of the spinal cord) are pinched or compressed.
Radiculitis
Despite the fact that in 60% of cases radiculitis has an acute course, it is rarely possible to cure the disease completely: most patients are forced to adapt to the disease, and therapy for chronic radiculitis is aimed primarily at eliminating pain and reducing the degree of compression of spinal nerve endings. Some people confuse radiculitis with an attack of lumbago, but with radiculopathy (the pathology is also called radicular syndrome), lumbago in the lower back is provoked by compression of the nerve roots, and with lumbago, other pathological conditions can cause pain, for example, myofascial syndrome or swelling of the paravertebral muscles of the lower back (without compression of the nerve roots). endings).
Lumbosacral radiculitis
Etiology and pathogenesis
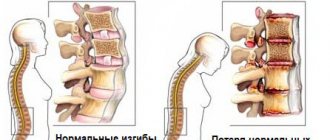
The pathogenetic mechanism of radiculopathy (radiculitis) is compression of the nerve roots, which are bundles of nerve fibers emerging from the spinal cord.
Structure of the spinal cord
The spinal cord has the appearance of a hollow tube with thick walls and is located in the central vertebral (spinal) canal formed by the vertebral arches.
Cross section of the spinal cord
In addition to the spinal cord, the spinal canal also contains blood vessels, the pia mater, the dura mater, and the arachnoid membrane. Nerve roots arise from the nerve trunks and extend beyond the spinal canal, forming the peripheral nervous system.
Pinching or compression of nerve bundles leads to severe lumbago in the lumbosacral region, forcing a person to take a certain body position and limiting his mobility. Such lumbago is called lumbago and is characterized by a sudden onset, acute course and high intensity.
Sharp pain in the lower back - lumbago
Unlike lumbodynia (pain in the lumbar region), which can have a long course with moderate or moderately high pain intensity, an attack of lumbago lasts from several minutes to several hours (less often, up to 1-3 days).
An attack of sharp pain (lumbago) rarely lasts more than three days
Note! Radiculitis can manifest itself not only as lumbago, but also as lumbar ischialgia. Sciatica is called sacrolumbar radiculitis, in which compression occurs on the sciatic nerve, which is the longest nerve trunk in the human body (from the lumbar region to the feet). The clinical picture of the pathology is represented not only by intense pain along the affected nerve, but also by pronounced neurological disorders, among which the leading place is occupied by paresthesia of the lower extremities.
Sciatica
What it is?
Radiculitis is an inflammation of the nerve roots entering the intervertebral foramina. Sciatica appears suddenly, and the pain is so severe that it is impossible to imagine it without experiencing it yourself. In 95% of cases, radiculitis is a consequence of osteochondrosis, in the remaining 5% it is the result of injuries, hernia, wear and deformation of the spinal column and intervertebral discs. People who play sports and lead a sedentary lifestyle are at risk for this disease.
Radiculitis can be acute - appear suddenly, as a consequence of injury or overexertion, and after timely treatment a person forgets about it for a long time, or chronic. The latter form occurs over time, due to ignoring the disease.
Clinical picture
The main clinical symptom of sacrolumbar radiculopathy is shooting or throbbing pain in the area where the nerves of the sacral plexus are located, which runs through the back of the pelvis and both limbs, reaching the feet. Patients with radiculitis complain of sudden (mostly acute and intense) shooting pain in the lower back, coccyx and sacrum areas, radiating to the buttocks, thighs, legs and feet. Depending on the location of the pinching, the clinical picture of the pain syndrome may vary. Sometimes patients talk only about discomfort and pain in the lower extremities, without connecting these symptoms with neurosurgical pathologies.
In order for the doctor to correctly make a presumptive diagnosis during the initial examination, the patient must report all existing symptoms, even if, in his opinion, they are not related to radiculitis.
The patient must report all existing symptoms
This is due to the fact that in some cases, radiculitis of the lumbosacral region does not have specific (characteristic only for this disease) manifestations. For example, acute heel pain may be perceived by a patient as a symptom of a heel spur, so obtaining a complete medical history is of great importance during the initial diagnosis.
You can suspect lumbosacral radiculitis if the following signs are present (usually a combination of them):
- attacks of lumbago and lumboischialgia (lumbago in the lower back with irradiation to the buttocks or lower extremities);
Attacks of pain - impaired motor activity (limping, twisted leg, etc.);
- partial paresthesia (numbness, stabbing or burning sensations, “goosebumps”, “freezing feet”);
Discomfort in the feet, numbness - changes in the skin (discoloration, dryness, thinning, appearance of uncharacteristic spots or rashes).
If the cause of radiculitis is endocrine diseases, secondary signs of pathology may be symptoms of a deficiency of certain vitamins and minerals: peeling and brittleness of nails, hair loss, peeling of the skin, and the appearance of sticking in the corners of the mouth.
Hair loss may be a secondary symptom
If your nails peel and break, it is important to rule out fungus.
A complete blood count often shows mild to moderate anemia (low hemoglobin).
Patients with diabetes and gout experience increased sweating
Diagnostics
Treatment of radiculitis is the responsibility of a neurologist. But if the course of the disease is complicated by injuries, intervertebral hernias or is of a discogenic nature, the intervention of more specialized specialists may be required, such as:
- traumatologists-orthopedists;
- vertebrologists;
- neurosurgeons.
To establish an accurate diagnosis, it is necessary to conduct a medical examination, including a number of procedures:
- Clarification of symptoms - determination of the intensity and characteristic differences of the pain syndrome, its duration, the presence of sensitivity disorders.
- Physical examination - allows you to determine the range of motion and muscle strength at the current time.
- Neurological examination - the patient's reflex reactions, activity and sensitivity of various parts of the body are checked.
- X-ray - gives a complete picture of the degenerative processes taking place.
- CT, MRI - allow you to accurately determine the degree of compression on the nerve roots.
- EMG - visualizes the nature and extent of damage to nerve fibers.
After identifying all the symptoms of lumbar radiculitis, treatment is prescribed, medicinal and using various modern therapeutic technologies.
Neurological symptoms
To determine the connection between shooting pains in the legs and lower back, the doctor can use special tests aimed at identifying reflex disorders.
Neurological changes
| Symptom | Description (how it appears) |
| Weak contraction of the calf muscles and absence of reflex flexion of the foot in response to irritation with a metal object (a blow with a medical hammer is used). |
| The patient needs to lie on his back, straighten the leg in which shooting pain occurs, and slowly raise its top. In people with radiculitis, when performing these actions, tension occurs on the sciatic nerve, which is manifested by severe pain (the patient cannot fully lift the straightened leg up). |
| This symptom is determined during the test to determine the Falre symptom. The syndrome is considered positive if the patient felt pain not only in the leg that he tried to lift, but also in the second limb. |
| The patient is placed face down on the couch so that the feet hang freely and are in a relaxed state. The doctor uses a medical hammer along the foot (strictly in the center) from the heel to the toes. With a normal plantar reflex, the toes and sole flex symmetrically. This does not happen with weakened reflex function of the foot. |
| The technique is almost the same as when diagnosing Falre's symptom, but the leg movement is carried out by a doctor (a symptom of tension of the sciatic nerve during passive flexion with fixation in the abducted position). |
The appearance of pain when pressing on diagnostic vertebroneurological points can also indicate lumbosacral radiculopathy. Such points are called Vallee points. They are located closer to the skin, and their irritation causes limited pain in the patient, which suggests neuralgic damage to the sciatic nerve.
Valle's pain points
Note! At home, sacrolumbar radiculitis with a predominant lesion of the roots of the sacral region can be identified by asking the patient to cross his legs (the sore leg should be on top). If the nerve endings are pinched, a person will not be able to do this due to intense pain.
If the nerve endings are pinched, a person will not be able to sit in this position
Complications
Complications from radiculitis are rare, but with untimely diagnosis and treatment, with prolonged compression of the nerve roots, disruption of nerve trophism (nutrition) and slowing of blood circulation, the following most often develop:
- Ischemia and infarction of the spinal cord.
- Inflammation of the meninges – spinal epiduritis or spinal cord arachnoiditis.
- Hemiparesis or paraparesis (partial paralysis of the limbs).
- Atrophic paralysis - develops as a result of prolonged compression of the spinal nerve and disruption of the innervation of the limbs.
Radiculitis - clinics in
Choose among the best clinics based on reviews and the best price and make an appointment
Family
Scoliosis Treatment Center named after K. Schroth
Moscow, st.
Azovskaya, 24, building 2 POM VI/KOM 5,6,7/ET 1 Sevastopolskaya
+7
- Consultation from 1500
- Exercise therapy from 2700
0 Write your review
Family
Oriental Medicine Clinic "Sagan Dali"
Moscow, prosp.
Mira, 79, building 1 Rizhskaya
+7
- Consultation from 1500
- Diagnostics from 0
- Reflexology from 1000
0 Write your review
Family
Center for Chinese Medicine "TAO"
Moscow, st.
Ostozhenka, 8 building 3, 1st floor Kropotkinskaya
+7
- Consultation from 1000
- Massage from 1500
- Reflexology from 1000
0 Write your review
Show all Moscow clinics
Forecast
A favorable prognosis is possible in case of timely diagnosis and comprehensive treatment, including all possible directions.
Only with this approach can one expect recovery without fear of relapse. In the case of development of ischemia and, as a consequence, spinal cord infarction, it is impossible to predict a complete recovery, since the consequence of such complications is often a violation of the motor and sensory functions of the body.
Sciatica: inflammation of the sciatic nerve Osteochondrosis of the lumbar spine Ankylosing spondylitis Tick-borne encephalitis Osteochondrosis of the cervical spine Vertebral artery syndrome
Radiculitis - specialists in Moscow
Choose among the best specialists based on reviews and the best price and make an appointment
VertebrologistOrthopedist
Gromov Ilya Sergeevich
Moscow, st.
Azovskaya, 24, building 2 POM VI/KOM 5,6,7/ET 1 (Scoliosis Treatment Center named after K. Schroth) +7 Registration
0 Write your review
VertebrologistOrthopedist
Kudryakov Stepan Anatolievich
Moscow, st. Azovskaya, 24, building 2 POM VI/KOM 5,6,7/ET 1 (Scoliosis Treatment Center named after K. Schroth)
+7
Registry
0 Write your review
Orthopedist
Prevention
As a preventive measure for radiculitis, it is recommended to carry out therapeutic exercises (not during an exacerbation). This is necessary to strengthen the muscles, which will remove excess stress from the spine and create a natural muscle corset. Swimming is beneficial for the spine, but in this case it is necessary to avoid hypothermia and sudden movements. It is advisable to fight excess weight, which increases pressure on the vertebrae. It is better to perform heavy physical work in a corset, try not to lift heavy objects, and do not stay in an inclined position for a long time.
It is also important to monitor your posture and proper nutrition. First of all, reduce the amount of salt in the diet, increase the intake of fiber (eat more raw vegetables, fresh salads). It is better to cook by steaming, avoiding fatty, fried, spicy foods. Sweets, coffee and strong tea should also be excluded if possible. Garlic, lemon juice, bananas are useful. Sometimes radiculitis is aggravated due to a lack of vitamin B12 in the body - it is advisable to add it and other nutritional supplements to the diet.