Causes
The causes of pyelonephritis lie in its infectious origin. The most common causative agents of the disease are staphylococcus and Escherichia coli; other pathogenic microbes (Proteus, gonococcus, enterococcus) have a somewhat less frequent negative effect. Acute pyelonephritis can develop against the background of chronic tonsillitis, influenza, pneumonia, caries, and skin furunculosis.
In addition, many unfavorable factors, both general and local, contribute to the occurrence of pyelonephritis. The first include:
- hypothermia of the body;
- stress;
- diabetes;
- weakened immunity;
- neurological problems;
- hypovitaminosis;
- HIV infection;
- heavy abdominal operations.
Local unfavorable factors contributing to the development of pyelonephritis include impaired urine outflow. This process is especially pronounced with kidney stones.
Pyelonephritis in women occurs with some peculiarities - in more than 50% of cases the disease has an ascending nature and develops against the background of cystitis, colpitis, and urethritis. In young girls aged 18–22 years, the occurrence of pyelonephritis is associated with the onset of sexual activity and pregnancy. Pyelonephritis also occurs in girls, 8 times more often than in boys. The cause is the same urogenital infections and lack of personal hygiene.
Pyelonephritis in men develops closer to old age. The cause of the malaise is urolithiasis or prostate adenoma. Young men suffer more from congenital anomalies of the genitourinary system.
Features of drug therapy in women
Pyelonephritis detected in a woman requires treatment to be prescribed immediately; only a doctor should select drugs and doses. The disease can spread quickly and progress.
Timely therapy is especially important during pregnancy. In this case, the disease may pose a threat to its progression. Careful selection of medications is also important: many of them are contraindicated, especially in the early stages. Their use can cause irreparable harm to the baby's health.
Groups of drugs for pyelonephritis and their characteristics
Therapy for the inflammatory process in the kidneys in women should be comprehensive. For this purpose, medications from several pharmacological groups are used for pyelonephritis. The most commonly used antibiotics are penicillin and cephalosporin drugs. They are prescribed in the form of tablets or intramuscular injections for a course of 1 to 2 weeks. The best way to select a medication from this group will be to analyze the sensitivity of the pathogen.
Antimicrobial synthetic agents that act bactericidal are included in the treatment. They can be divided into groups: fluoroquinolones, nitrofurans, hydroxyquinolines, sulfonamides. Herbal medicines are used for a long time to improve the condition of the kidneys. Be sure to use symptomatic remedies. These can be antispasmodics, antipyretics, non-steroidal anti-inflammatory, painkillers.
Review of the most used products
The most commonly prescribed tablets for pyelonephritis are penicillin in nature. A medicine called “Amoxiclav”, produced in 250, 500, and 875 mg doses, has proven itself well. The active substance is active against a large number of pathogenic pathogens and effectively destroys them. Take orally before meals three times a day, course from 5 to 14 days, the drug is contraindicated in case of individual intolerance to the components, liver diseases. The dosage is calculated by the attending physician specifically for each patient; it is not recommended to prescribe in the first trimester of pregnancy.
The amoxicillin series of antibiotics is represented by Flemoxin Solutab, which is resistant to the acidic environment of the stomach. This helps it maintain its unchanged appearance, provide a good therapeutic effect, the drug is effective against Proteus, streptococcus, take it two or three times a day in the amount prescribed by the doctor.
For the treatment of pyelonephritis, Nitroxoline is used, an antimicrobial, antiprotozoal drug, available in 50 mg tablets. The active substance suppresses pathogens such as tubercle bacilli and Trichomonas. Adults are usually prescribed 100 milligrams four times a day; in severe cases, the dose is doubled; it should be used with caution in patients with impaired renal function.
"Furadonin" is an inexpensive drug that is often the choice in the treatment of cystitis and pyelonephritis; it has an antimicrobial and antibacterial effect. The medication is taken after meals with plenty of water; it should be taken into account that the urine may turn yellow.
Furagin has a wide spectrum of action, successfully helping to fight kidney inflammation in most cases. Resistance to this drug develops very slowly, which is its positive quality. Your urine may turn orange when you use this medication.
A new third-generation antibiotic with a high rating, which has recently been included in the treatment of pyelonephritis, is Suprax. It is active against most pathogenic microorganisms in humans and has a small number of contraindications and side effects.
A plant-based drug called “Canephron” is used in the complex treatment of the urinary system. It helps with acute and chronic infections, prevents exacerbation, and is preventive in the formation of stones. The components contained in the drug have an antiseptic, antispasmodic effect, improve kidney function, and enhance the effect of antimicrobial medications.
produces the homeopathic drug “Solidago compositum S” for the treatment of inflammatory diseases in urology. It has a detoxifying, regenerating effect, and has a diuretic effect without side effects. Available in ampoules, quite expensive, the treatment regimen is prescribed by a doctor.
Traditionally, it is used in the form of injections, one ampoule 1 to 3 times a week for a month or a month and a half. A good therapeutic response of this drug is also observed in urolithiasis.
If pyelonephritis has become chronic, various complications have appeared, kidney function has been impaired, “Restrukta with injection C” is added to the treatment. It relieves inflammation, intoxication, and has an immunomodulatory effect. The medicine should not be prescribed during pregnancy. The course of treatment is the same as the previous medication. There is also a whole list of drugs produced by this drug that are auxiliary in the treatment of diseases of the urinary system.
Drug treatment of pregnant and lactating women
Pyelonephritis in women in an interesting position is very common. The danger of this condition is that, if left untreated, spontaneous abortion may occur in the second trimester. Intrauterine transmission of infection to a child is also possible.
Self-medication in this case is unacceptable; the expectant mother is prescribed antibiotics. Moreover, their use will cause much less harm than an untreated infection.
Attention! Prescriptions should be made exclusively by a doctor: there are many drugs that can only be used from the second or even third trimester. Their use in the early stages can cause serious pathologies in the fetus. Medicines for pyelonephritis in pregnant women can be based on ampicillin, methicillin, oxacillin.
Medicines for older women
When treating pyelonephritis in elderly women, it is important to prescribe medications after examining the condition of all organs and systems. All existing diseases must be taken into account. It is necessary to carry out bacteriological culture of urine to determine the sensitivity of the pathogen to antibiotics.
Most often, broad-spectrum agents are prescribed: cefuroxime, nolicin, amoxicillin. For elderly patients, aminoglycosides and lolimixins are not used. Doses should be 25-50% lower than generally accepted. After acute symptoms are relieved, doctors recommend maintenance therapy for geriatric patients for more than six months. Every month for at least ten days a course of some nitrofuran (for example, Furazolidone) is prescribed.
Next, herbal infusions that have diuretic and antiseptic properties are used at home. Using a decoction of Chinese rose helps to quickly cope with the disease and serves as a good folk prophylactic.
Symptoms
The acute form of pyelonephritis begins suddenly. The patient's temperature rises sharply to 39–41°C, low back pain, dizziness, and nausea occur. Along with the fever, profuse sweat appears.
One of the most characteristic signs of acute purulent inflammation in the kidneys is stunning chills. Pain from pyelonephritis can be either dull or sharp, localized on one side of the back or spread throughout the abdomen. Primary pyelonephritis often goes away without any sensation.
In contrast, the secondary form of pyelonephritis, which occurs as a result of pinching or blockage of the urinary ducts, occurs with severe painful attacks, reaching the intensity of renal colic. If you do not seek help at this stage, pyelonephritis takes a chronic form or is accompanied by a suppurative process.
Specific signs of acute pyelonephritis:
- general intoxication of the body (lethargy, weakness, migraines, deterioration of health);
- pain in the lower back or lateral abdominal muscles;
- increased blood pressure;
- change in urine (turbidity, addition of blood);
- the appearance of pollakuria and nocturia;
- development of anemia.
Edema syndrome is not typical for pyelonephritis and, as a rule, excludes this pathological process. However, a disease complicated by glomerulonephritis can occur with pastiness.
Chronic pyelonephritis is characterized by sluggish symptoms and an undulating course - periods of remission are constantly replaced by relapses. Often, the sluggish form is associated in patients with any other urogenital pathology: cystitis, prostate adenoma, kidney stones.
Such an unexpressed course of chronic pyelonephritis significantly complicates diagnosis and delays treatment.
Among women
Symptoms of pyelonephritis in women generally do not differ from the standard ones, however, there are a number of signs that are characteristic only of the weaker sex:
- pyelonephritis usually begins with cystitis - trips to the toilet become frequent and painful, nagging pain in the bladder and chills appear;
- chronic inflammation develops unnoticed, much like discomfort before menstruation - aches in the lower back and lower abdomen, general deterioration in well-being;
- Ladies with curvy figures may experience no pain.
Pyelonephritis in women in the last stages of pregnancy manifests itself only as pain when urinating. The rest of the symptoms are mild.
In men
Pyelonephritis in men also has several characteristic details. Firstly, instead of pain, there may be pronounced tension in the abdominal muscles from the affected organ. The symptom causes some discomfort and misleads the patient.
Secondly, chronic pyelonephritis in men is often accompanied by an increase in blood pressure to critical levels. This symptom is not typical for women.
In children
In children, the pathological process occurs much less frequently than in adults and is usually asymptomatic, or the child, due to his age, simply cannot talk about poor health.
Parents should be alert to the following symptoms:
- mood swings, causeless whims, crying;
- frequent urination, worse at night;
- lethargy, fatigue, refusal of active games;
- loss of appetite;
- pallor of the skin.
For young children suffering from pyelonephritis, abdominal syndrome is characteristic. It manifests itself as severe discomfort in the abdomen in the absence of diseases of the gastrointestinal tract.
Diagnostic measures
It is often impossible to diagnose pyelonephritis in the initial stages of the disease due to the fact that the symptoms of this disease are similar to many other pathologies, or the process occurs in a latent form.
Pyelonephritis is often detected in a patient during examination for other diseases.
In this regard, if even slight discomfort occurs in the lumbar region, you should immediately contact a specialist in nephrology or urology.
The doctor will examine the patient, clarify the medical history and prescribe appropriate diagnostics to refute or confirm the pathology.
Pyelonephritis can easily be confused with the following diseases:
- infectious processes - sepsis, malaria;
- hydronephrosis, in which the renal cavities expand and the organ ceases to function;
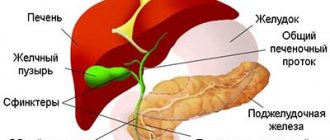
- acute pancreatitis (inflammatory process of the pancreas);
- pyelonephrosis, in which the kidney cavity is filled with purulent masses, stones or urine;
- appendicitis;
- cholecystitis - inflammation of the gallbladder;
- Kidney infarction is a condition in which, due to blockage of a vessel in the kidney, necrosis of its tissue occurs;
- pus in the tract leaving urine, in the acute stage;
- pneumonia;
- shingles;
- splenic infarction;
- glomerulonephritis in the acute stage, in which inflammation of the glomeruli of the kidney occurs.
Lab tests
They should be carried out to diagnose the disease, without fail, namely:
- General blood test , which allows you to determine the presence of an inflammatory process in the body (increased ESR, a large number of leukocytes).
- Biochemical blood test , which determines the amount of urea, creatine, and potassium in the patient’s body. If potassium is increased, then we can talk about kidney failure.
- General urine analysis . With pyelonephritis, the urine is dark in color, protein is found in it, and the pH level is elevated.
- Urine culture test , with which the doctor qualitatively determines the name of the antibiotic for the patient.
- Urinalysis according to Nechiporenko, which makes it possible to see an increased number of leukocytes compared to red blood cells.
- The prednisolone test makes it possible to detect a disease that occurs in a latent form. To conduct the study, a woman is given a medicine into a vein, after which, after an hour, two and three, it is necessary to collect portions of urine. After 24 hours, the analysis is sent for testing. If an increased number of leukocytes is detected, then the diagnosis of pyelonephritis is confirmed.
- Urinalysis according to Zemnitsky , which may reveal a decrease in the density of urine.
In addition to testing, the doctor may prescribe additional tests:
- Ultrasound of the kidneys to assess the general condition of the organ;
- excretory urography, which gives an idea of the mobility of the kidney;
- computed tomography, with its help, you can study the kidneys in more detail in comparison with ultrasound;
- cystometry, identifies pathological processes in the bladder if they exist;
- cystography - X-ray contrast study.
A woman must also visit a gynecologist.
Nature of pain
As mentioned above, pain with pyelonephritis can manifest itself in different ways. During the latent period, symptoms of the disease are practically absent. Occasionally, pain is localized in the lumbar region and lateral abdominal muscles. With primary pyelonephritis, discomfort affects both sides, with secondary pyelonephritis - only one.
Exacerbation of the pathology is manifested by sudden, sharp pain, up to renal colic. Moreover, the unpleasant sensations do not depend in any way on the position of the body. During an attack, pain may radiate to the groin area and spread along the front surface of the thigh.
Chronic pyelonephritis is characterized by dull aching sensations in the lumbosacral region, radiating to the lower abdomen.
Manifestation of acute pyelonephritis
Acute pyelonephritis can occur in any woman in the absence of the necessary hygiene and preventive measures. Although pathogens usually enter through the urethra, sometimes the infection enters the body hematogenously, that is, through the blood. Symptoms of pyelonephritis in women are as follows;
- increase in body temperature to 38-39 degrees;
- increased heart rate;
- increased blood pressure;
- presence of nausea and vomiting;
- the appearance of pain in the lumbar region and lower abdomen;
- frequent urination;
- swelling of the limbs;
- unpleasant vaginal discharge;
- change in the color and odor of urine;
- presence of blood in urine;
- feeling of weakness and lethargy;
- the appearance of severe sweating and/or chills.
Signs of pyelonephritis in women resemble symptoms of cystitis, so to clarify the diagnosis, blood and urine tests and an in-person examination by a nephrologist or therapist are required. On examination, pain may be observed in the costovertebral angle on the side of the affected kidney. Increased blood pressure is more common in women with diabetes and neurological abnormalities. Micro- or macrohematuria is characteristic of only 10% of patients. The complicated process is accompanied by urosepsis, acute renal failure, and necrosis of the renal papillae.
Some women may have their own individual manifestations associated with age and general health. To clarify the diagnosis, laboratory, ultrasound and instrumental examination are required. Laboratory testing involves blood and urine tests, smears for the presence of pathogens. Ultrasound of the kidneys, bladder and abdominal cavity allows you to determine the condition of the entire genitourinary system. In addition to these studies, if necessary, X-rays and chromocystoscopy are performed. A CT scan is prescribed to rule out urolithiasis.
Classification
The modern classification of pyelonephritis includes many signs. Most of them are grouped according to the type and nature of the development of the pathological process.
Systematization begins with the division of the disease into acute and chronic pyelonephritis. Each is then considered by causal factor:
- primary - occurs against the background of inflammatory processes in the body;
- secondary - is mechanical in nature and manifests itself when there are disturbances in the outflow of urine.
Based on the number of affected organs, they are distinguished:
- unilateral pyelonephritis - most often localized in the right kidney;
- bilateral pyelonephritis - both organs are involved in the infectious process.
According to the phases of inflammation, the acute pathological process is divided into a latent (hidden) stage and an active stage, which is characterized by a surge of symptoms. Chronic pyelonephritis often goes into remission and then recurs again. This wave-like course of the disease can continue for a very long time.
Signs of chronic pyelonephritis
Girls and women very often suffer from diseases of the genitourinary system. Chronic pyelonephritis is considered one of the most common kidney diseases. Recognizing the disease is not so easy, because the manifestation of the chronic form of the disease does not have clear symptoms. In chronic pyelonephritis, the inflammatory process affects one or two kidneys at the same time. The disease often develops during puberty, defloration, pregnancy or menopause.
Chronic pyelonephritis is replaced by phases of exacerbation and remission, therefore, when performing an ultrasound, foci of inflammation with scar tissue are observed in the kidneys. During the pathological process, the death of healthy tissues and the formation of renal failure occur. Since the disease does not cause much discomfort, women are in no hurry to seek help. But the constant inflammatory process prevents the kidneys from performing their functions properly, which leads to disruption of water-salt metabolism and the appearance of edema. In an advanced state, a purulent infection develops, which can lead to serious complications.
Causes of chronic pyelonephritis:
- acute untreated cystitis;
- the presence of otitis, urethritis, cholecystitis;
- diabetes;
- obesity;
- vaginal infections;
- immunodeficiency;
- constant hypothermia;
- oral infections;
- weakening of the body's defenses.
The reason may be heredity, working in a cold and damp room, or a sedentary lifestyle. Chronic pyelonephritis manifests itself:
- low-grade fever;
- chills and fever;
- arthralgia;
- headache;
- dizziness;
- intoxication of the body;
- weakness;
- lack of appetite;
- vomiting (rarely);
- pain in the ureters or lower back;
- unpleasant sensations when urinating (pain, burning, itching);
- dysuria;
- frequent urge to urinate at night;
- bacteremia;
- dry skin;
- cloudy urine.
The described symptoms are often attributed to fatigue and stress, so treatment usually begins in the acute stage.
Diagnostics
Diagnosis of pyelonephritis begins with a general examination and questioning of the patient. Then the patient is prescribed a number of laboratory and instrumental measures that clarify the picture of the disease:
- general analysis of urine and blood;
- urine culture;
- Ultrasound of the kidneys;
- survey and excretory urography;
- CT;
- retrograde pyeloureterography.
Ultrasound of the kidneys in pyelonephritis does not always reveal pathological changes in the required volume, so ultrasound examinations are often supplemented with nephroscintigraphy and abdominal aortography.
Differential diagnosis of pyelonephritis is carried out with chronic glomerulonephritis, hypertension, cystitis.
Why does pyelonephritis “prey” on women?
The cause of the inflammatory process in the kidneys is pathogenic microorganisms. In 90 cases out of 100, the causative agent of the infection is Escherichia coli; much less frequently, Pseudomonas aeruginosa, Proteus, enterococci and staphylococci become the cause of the disease.
The infection enters the kidneys through the urethra. In women it is quite wide and short (approximately 3 cm). Since the urethra is located in close proximity to the entrance to the vagina and anus, pathogenic microorganisms enter from there first into the urethra, and from there into the bladder.
The entry of infection into the kidneys from the bladder is referred to as the “ascending route.” How does this happen? Urine is expelled upward from the bladder. This process is called reflux. Bacteria can also enter the kidney via an ascending route without the presence of reflux, although this significantly increases the likelihood of developing pyelonephritis.
It occurs in cases where the natural outflow of urine is obstructed:
- the presence of stones;
- structural defects of the bladder;
- inability to release urine due to an unforeseen situation (being in a public place without access to a toilet).
Once in the kidneys, the infection initiates an inflammatory process.
In addition to the ascending route of infection into the kidneys, a descending route is also noted. Pathogenic microorganisms can be delivered by blood flow to the kidneys from any source of infection: from a diseased tooth, from the intestines, from the respiratory tract, etc.
Treatment
Simple acute kidney pyelonephritis is treated in a hospital setting with conservative therapy. Medicines are prescribed taking into account the cause of the disease, the severity of the patient’s condition and the presence of concomitant pathologies.
Drug treatment of pyelonephritis includes the following groups of drugs:
- antibiotics and antiseptics - Nitroxoline, Furagin, Urosulfan, Chloramphenicol, Gentamicin (i.m.), Doxycycline, Cefuroxime, Amoxicillin;
- immunomodulators (i.m.) - T-activin, Timalin;
- NSAIDs - Voltaren, Ortofen;
- multivitamins, tincture of Ginseng, Eleutherococcus.
For difficulty urinating, drug therapy is combined with catheterization of the ureter.
Chronic kidney disease is much more difficult to treat. Pathology requires much more time and effort. The main therapy is supplemented with the prescription of diuretics (Furosemide) and drugs that improve blood circulation (Curantil). In case of severe septic kidney damage, nephrectomy is resorted to.
Treatment of pyelonephritis in women is carried out as usual. Often, recovery in the acute form of the disease is apparent, therefore, within a year after therapy, patients should be monitored at a dispensary.
Rehabilitation for pyelonephritis of any complexity lasts about 2 months and includes exercise therapy, therapeutic nutrition, physiotherapeutic procedures and herbal medicine.
Preventive measures for pyelonephritis
Although pyelonephritis is treatable, the best “cure” is prevention. It is very important to promptly treat all urological diseases. Often patients use folk remedies, which further aggravates the situation. Symptoms partially disappear, but the disease itself progresses. Therefore, well-chosen drug therapy helps prevent kidney disease. Women should empty their bladder completely, avoid hypothermia, and use condoms to prevent STDs.
With pyelonephritis, women often experience unpleasant vaginal discharge, so it is necessary to visit a gynecologist. Vaginal flora smears allow you to determine the presence of vaginal ailments that need to be treated without delay. Never use other people's towels, even close relatives. In case of a chronic process, it is recommended to avoid swimming in public pools.
Buy quality shoes that don't get wet. Make time for moderate exercise to avoid congestion in the pelvic organs. After questionable sexual contact, treat the genitals with an antiseptic. If you suspect an infection, consult your doctor immediately. Never disregard doctors' recommendations.
Diet
For any form of pyelonephritis, the patient is recommended to increase fluid intake: clean water, lingonberry leaf decoction, cranberry juice or fruit drink. Strong meat and fish broths, hot seasonings, fried and pickled foods, baked goods should be excluded from the diet, and salt intake should be limited.
The diet of patients with pyelonephritis should consist of dairy and plant products, white meat, boiled fish, vegetables and fruits. Once a week, the patient is allowed to eat the yolk of an egg in the form of an omelet or soft-boiled. Read more about diet for kidney disease→
Treatment of pyelonephritis at SM-Clinic
- Treatment is carried out according to evidence-based medicine protocols, we achieve recovery in the shortest possible time and do not burden the body with useless medications.
- Acute pain syndrome is effectively relieved.
- Complex therapy is prescribed so as not to dull the symptoms, but to ensure the elimination of the pathology.
- For acutely ill patients, home care and 24-hour hospital care are available.
To receive prompt, qualified help, make an appointment with a nephrologist online.
Complications
Complications of pyelonephritis develop in the absence of treatment or inappropriate selection of medications. Thus, the acute form of the disease often ends in purulent paranephritis, kidney abscess or tissue necrosis.
Chronic pyelonephritis often causes acute renal failure, kidney shrinkage, sepsis and bacterial shock. If complications of bilateral pyelonephritis develop, the patient may need lifelong hemodialysis or transplantation.
Consequences of the disease
If not treated correctly, pyelonephritis can become chronic.
The chronic form of this disease is dangerous because in most cases it is asymptomatic and is detected by chance.
Untreated pyelonephritis also has a negative impact.
The consequences of such situations are extremely unpleasant. This is pedunculitis, in which the kidney becomes inflamed in the hilum area, then moves to the stalk, then sclerotic changes occur.
Necrotizing papillitis is also possible, as a result of which the renal papillae are killed. Renal failure, leading to kidney necrosis, is also extremely dangerous.
Facts and statistics
- Every year in the United States, an average of 1 person out of every 7 thousand people falls ill with pyelonephritis. 192 thousand of them are undergoing inpatient treatment in specialized departments of hospitals and clinics.
- Women suffer from pyelonephritis 4-5 times more often than men. Acute pyelonephritis occurs more often in women who are sexually active.
- In 95% of patients, treatment of pyelonephritis gives a positive result within the first 48 hours.
- In childhood, pyelonephritis develops in approximately 3% of girls and 1% of boys. 17% of them develop cicatricial changes in the renal parenchyma, and 10-20% develop hypertension.
- Plain water can significantly improve the condition of a patient with pyelonephritis. Drinking plenty of fluids maintains normal fluid balance and also dilutes the blood and helps eliminate more bacteria and their toxins. This occurs due to frequent urination in response to increased fluid intake.
- Although even slight movement can cause severe pain with pyelonephritis, it is important to urinate as often as possible. Although the patient feels discomfort during urination, this is the only way to get rid of the causative agent of the disease - bacteria are removed from the body only with urine. Uncontrolled growth of microorganisms will worsen the condition, causing sepsis (blood poisoning) and can even cause the death of the patient.
- Cranberry juice is considered a good helper in the fight against pyelonephritis. The juice can be drunk pure or diluted with water (see how to make cranberry juice). In this case, you should completely avoid drinking alcohol, sweet carbonated drinks and coffee.
What antibiotics can be prescribed without analysis?
In most cases, the causative agent of infection in an ordinary person who does not live in a dormitory or boarding school is E. coli. Therefore, at the first stage, 3rd generation cephalosporins may be prescribed, to which the microorganism has no resistance. One drug may be sufficient; if the patient is intolerant to cephalosporins, reserve drugs are recommended.
In patients weakened by concomitant diabetes, the cause of acute pyelonephritis is often staphylococcus, sensitive to ciprofloxacin and other drugs. In all cases, toxic drugs with a selective effect on the kidneys - nephrotoxic drugs, which are predominantly excreted by the liver - are not used. Additionally, intravenous solutions are prescribed to improve metabolic processes in the kidneys and replenish fluid deficiency.
We will call you back
Leave your phone number
What does a severe course of the disease promise?
The effectiveness of pyelonephritis therapy is not always determined only by the sensitivity of microorganisms to drugs and the correctness of treatment measures; there is a group of causal factors that worsen therapeutic prospects:
- Pregnancy, firstly, the growing uterus interferes with the passage of urine; secondly, there are significant restrictions on the use of medicines; thirdly, the notorious hormonal changes.
- In men, pyelonephritis is worse because it occurs in old age against the background of irreparable urological problems and concomitant diseases.
- Immune disorders, especially HIV, help develop infections with an atypical pathogen, which is fundamentally not pathogenic.
- Out-of-control diabetes mellitus and autoimmune diseases affecting connective tissue. In principle, any chronic disease worsens the prognosis of kidney infection.
Diagnosis of pyelonephritis by blood test
Diagnosis of kidney inflammation using a general blood test tends to zero in terms of specificity. There will be a lot of leukocytes, with a predominant proportion of neutrophilic forms, especially stab ones, accelerating the erythrocyte sedimentation reaction (ESR). This is a typical blood condition in any infection, proof that there is an inflammatory process in the body, but this is not enough to make a diagnosis of pyelonephritis.
Biochemical analysis will show the functionality of the paired organ only if the disturbances are significant.
Take care of yourself, book a consultation now
Risk factors leading to kidney inflammation
If there is an obstruction to the normal flow of urine, there are factors that increase the likelihood of developing a urinary tract infection. The reasons are almost the same as those that help initiate acute cystitis:
- Sexually transmitted infections and the costs of sexual behavior;
- Age-related decrease in hormone production, dyshormonal disorders and the use of hormonal drugs, most often contraceptives;
- Immune capabilities linked to blood group, which are referred to as “secretory type”;
- A complication of diabetes mellitus is damage to small vessels or microangiopathy.
Pyelonephritis in pregnant women
The incidence of bacteriuria during pregnancy is 4-7%. Pyelonephritis develops in approximately 30% of pregnant women from this group (1-4% of the total number of pregnant women). Most often, symptoms of pyelonephritis appear in the second trimester. Among the complications of pyelonephritis in pregnant women are:
- Anemia (23% of cases);
- Sepsis (17%);
- Renal failure (2%);
- Premature birth (rare).
An increased incidence of asymptomatic bacteriuria in pregnant women is observed among representatives of a low socioeconomic class, as well as in multiparous women.
When can pyelonephritis not be treated at home?
Primary inflammation of the kidneys can develop completely without a reason - “sitting on a cold stone”, but in most cases the cause of the infection is based on a violation of the correct flow of urine from the renal pelvis through the ureter into the bladder and beyond.
All patients with acute pyelonephritis are hospitalized to identify a process that interferes with the passage of urine. Outpatient treatment is provided only in cases of uncomplicated inflammation of the kidney, with absolute confidence that nothing prevents urine from flowing along the natural path.
Treatment in a hospital is absolutely indicated:
- with a single kidney or the presence of a second unhealthy one,
- clinical signs of purulent inflammation and septic reaction,
- with immunodeficiency and lack of response to antibiotic treatment.
Our expert in this field:
Dmitriev Sergey Viktorovich
Urologist, Ph.D.
Call the doctor