IOP, or intraocular pressure, is a very important diagnostic indicator that determines the health of the visual organ.
It may increase or decrease.
Every person should have their intraocular pressure checked during their annual medical examination. This will help detect the presence of dangerous eye diseases at a very early stage of development. If you do not follow this advice and do not treat eye diseases, you may lose your sight.
General norm of IOP
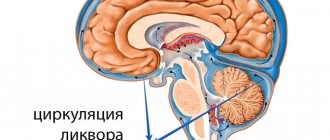
Intraocular pressure is the tone that occurs between the membrane of the eyeball and its internal contents. 2 mm3 of fluid enters each eye every minute, and the same amount is removed. With various pathologies, the difference between fluid inflow and outflow increases. It accumulates in the eyes, which leads to deformation of blood vessels and disruption of the optic nerve.
The pressure inside the eye is expressed in millimeters of mercury. The optimal value is 9 – 23 mmHg. When using the Maklakov method, the pressure increases - from 15 to 26 mmHg. Indicators may change throughout the day, depending on physical activity and other factors. But if pressure variability remains within normal limits, there is no need to worry. It is believed that the upper limit of normal is 21 mmHg. And all values from 21 to 23 mm are considered suspicious.
We recommend reading: Low eye pressure
Typically, IOP remains unchanged at any age. But it varies widely with different eye pathologies. Interestingly, it can change depending on the season, and this factor must also be taken into account in the diagnostic process.
The pressure may be asymmetrical in the right and left eyes. The discrepancy should not exceed 4 mmHg.
About other measurement methods
There are several basic ways to determine eye pressure. The first is palpation, that is, the doctor determines the IOP with his fingers through the patient’s eyelid. It is usually used after surgery, when it is impossible to use special instruments for examination.
Measuring intraocular pressure by palpation
Non-contact method. Obviously, the tonometer in this case does not contact the eye. Indicators of corneal deformation are determined using air pressure. The fastest results can be achieved with computer processing. Local anesthesia is not required and there may be no side effects.
Pneumotonometry
With the contact method, the measuring instrument is in contact with the eye, and therefore, to avoid pain, anesthesia is used. This type of tonometry can be:
applanation. Maklakov weights or a Goldman tonometer are used, very accurate results;
Goldmann applanation tonometer
impressive. Here measurements are made with an Icare or Scholz tonometer. The procedure itself is based on the use of a special rod, which is gently pressed into the cornea. Everything happens quickly and painlessly;
Icare tonometer
contour dynamic. It implies strict adherence to the measurement rules; the results are not as accurate as in the first case. But it has one advantage - it is the individuality of the blood supply.
Dynamic contour tonometer
Intraocular pressure in glaucoma
As glaucoma develops, intraocular pressure changes. It is most convenient to present them in the form of a table.
| Glaucoma stage | IOP indicator |
| Initial | IOP does not exceed 27 mmHg. Usually it exceeds the previous values by 4 - 5 mm. |
| Expressed | The indicator does not exceed 32 mm. |
| Deep | IOP is 33 mmHg. |
| Final (terminal) | More than 33 mmHg. |
Increased ophthalmic tone is the main problem of glaucoma. Almost all methods of treating this dangerous disease consist of reducing IOP. Even a small decrease in pressure inside the eye significantly reduces the risk of blindness.
Glaucoma is insidious in that it may not manifest itself as an increase in pressure. In this case, they talk about a variant of the pathology with low pressure. In the initial stages of the disease, a person may not feel the symptoms of the pathology at all and have good vision. The manifestation of glaucoma is always acute with the addition of headache, nausea, and sometimes vomiting.
Surgery
If the disease has led to serious eye damage, radical treatment methods are needed. If eye pressure increases, surgical intervention is prescribed. Today, several types of operations are known:
- Excision of the iris using a laser;
- Laser stretching of trabeculae.
Thanks to such interventions, it is possible to normalize the outflow of fluid, which normalizes blood pressure.
In advanced cases, glaucoma develops. However, thanks to modern methods, it is possible to provide the patient with a normal lifestyle. If a person does not take any measures for a long time, there is a risk of developing dangerous pathologies of the organ of vision.
One of these disorders is optic nerve atrophy. This phenomenon is characterized by deterioration of vision, which subsequently leads to complete blindness. Dangerous complications include detachment or complete rupture of the retina, which requires surgical intervention.
Normal IOP in children
The normal intraocular pressure in children is the same in both sexes. For young patients, it is allowed to use tonometry to determine the indicator of eye functioning in question.
Parents need to pay attention to their child's behavior. When intraocular pressure changes, the child may experience heaviness in the eyes, pain in the head, and feel tired. Fatigue is especially noticeable in the evening.
At the first symptoms of increased ophthalmic tone in a child, he should be urgently shown to a pediatrician or ophthalmologist. After measuring the IOP value, he will develop further measures. It is necessary to pay attention to the fact that glaucoma develops extremely rarely in children. An increase in IOP in young children often indicates a malfunction of the thyroid gland.
We recommend reading: Eye pressure in children
Drug therapy
Source: gipertenziya.info In addition to the listed methods, medications and lifestyle correction are used.
Doctors prescribe special drops for high eye pressure. Such substances improve the outflow of fluid and fill the eyes with nutrients. This allows you to cope with the problem at the initial stage of its development. Today there are many different drugs. However, doctors do not advise self-medication. That is why it is so important to contact an ophthalmologist in time, who will select the medicine.
Eye drops to reduce high blood pressure are divided into several groups:
- Carbanhydrase inhibitors (Azopt, Trusopt, etc.) Reduce the production of intraocular fluid. Possible side effects of these pressure eye drops: burning after instillation, redness of the eyes, bitter taste in the mouth.
- Prostaglandins (travatan, xalatan, taflotan, etc.) Increase the outflow of intraocular fluid. Side effects: darkening of the iris, lengthening of eyelashes.
- Beta blockers (Timolol, Betaxolol) Reduce the production of intraocular fluid. As a rule, they are prescribed together with prostaglandins. These pressure eye drops may affect your heart rate. May cause unwanted side effects in people with diabetes.
- Miotics are drugs that reduce the diameter of the pupil and thereby improve the outflow of intraocular fluid. One of the most prescribed drugs in this group by ophthalmologists is pilocarpine.
- Combined drugs that reduce the production of ocular fluid and increase the outflow - proxofeline.
All drops that reduce intraocular pressure (especially beta blockers) can cause complications. Therefore, these drops (antiglaucoma) should only be prescribed by an ophthalmologist.
A qualified specialist will not only prescribe drops taking into account the individual characteristics of the patient’s body, but will also monitor the effectiveness of the prescribed treatment.
With increased eye pressure, drops are intended to drain excess fluid from the eye, and they also nourish the eye with useful substances.
These include prostaglandins such as:
- Travatan
- Tafluprost;
- Xalatan;
- Travatan.
These drops are quite popular as they are effective on the eye, but have side effects. With prolonged use of drops, the patient's pupil narrows, therefore the field of vision decreases, and pain in the temples and frontal parts may occur.
There are also a number of drugs aimed at improving vision, these include carbonic anhydrase inhibitors: Trusop, Azop. They do not cause adverse reactions, but can negatively affect the functioning of the kidneys, so these drops should only be used as prescribed by a doctor. Self-medication is strictly prohibited.
How is intraocular pressure measured?
IOP analysis is called tonometry. There is no need for special preparation before this examination. It is recommended to fulfill certain conditions:
- You must come to the examination in loose clothing;
- the patient does not need to worry before and during tonometry;
- 4 hours before the examination you do not need to drink a lot of liquid;
- contact lenses must be removed.
There are several ways to measure pressure. In the case of using the Maklakov method, the cornea is pre-treated with an anesthetic solution. Next, a medical load is placed on it. During tonometry, the eyeball sag and this area is colored with pigment.
The Goldmann method uses a slit lamp and an ophthalmic probe. An anesthetic is also instilled into the eyes. A paper strip is placed on the eye, then pressure is applied to it. A trace of pigment remains on the organ of vision and is analyzed.
An alternative diagnostic method is impression tonometry. It is carried out only in an eye hospital. Upon contact with the eyeball, the tonometer automatically records the tone, and the diagnostic results are displayed on the monitor screen.
During pneumotonometry, compressed air is released onto the eyeball. Based on the reaction of the cornea to the air stream, an increase or decrease in intraocular pressure is judged. This diagnostic method does not involve the use of painkillers. Most often it is used to diagnose blood pressure in children.
The simplest way to determine ophthalmic tone is palpation of the eye. The patient himself can do this. He needs to close his eyes, look down. Next, you should rest your forehead on your thumbs, and touch your eyelid with your index fingers and lightly press on it. If the pressure is increased, the eyeball will be elastic (and if it is significantly higher than normal, it will be hard as a stone). On the contrary, when IOP decreases, the sclera will seem to be “pressed through.”
Folk remedies
With the help of folk remedies, you can not only stabilize the pressure in the eyes, but also replenish the body’s vitamin reserves, as well as improve metabolism.
Facilities:
- Rinse with aloe juice. Prepare a solution of 6 crushed aloe plant leaves and a glass of boiling water, pour over the leaves and boil for 5-6 minutes. Cool and wash the eye area with the resulting product 5-7 times a day. Make a course of such therapy lasting 2 weeks, after which you need a break for the same period.
- Tomato juice. Drink this delicious medicine 1/4 cup at a time, 4-5 times a day. The course of treatment is 21 days, after which you need to take a break and start therapy again.
- Honey and celandine. Take both ingredients in equal parts, mix and cook until thick. Leave to cool and apply this product on a napkin to your eyes.
- Nettle and lily of the valley flowers. For the infusion you will need 1 glass of crushed nettle and 2 small spoons of lily of the valley flowers. Mix the ingredients and add 2 cups of water at room temperature. Leave to steep overnight. In the morning, add 2 teaspoons of baking soda to the mixture. Use the product as an eye lotion.
The list of folk recipes for this disease is huge, but you need to carefully analyze the effect of the components of such home remedies.
What to do if you have high intraocular pressure? Only professional help is needed for such patients; it is not worth solving this problem on your own. After consulting a doctor, it will become clear to a person what medications he needs and what folk remedies can alleviate his condition.
Fundus examination
Fundus examination (ophthalmoscopy) is an examination of the retina, its vessels, optic nerve, and choroid. The method is based on the reflection of light rays from the fundus of the eye. Diagnosis is carried out using an ophthalmoscope. The doctor directs a light beam from the device lamp into the eye. In certain positions, the macula, the retina and its vessels, and the periphery of the eye are examined.
Ophthalmoscopy is one of the most commonly used eye examinations. There is an indirect ophthalmoscopy, in which the doctor receives an image with approximately 15x magnification.
Direct ophthalmoscopy involves magnifying the image approximately 5 times.
Diagnostics of fundus pressure is carried out after standard procedures - checking the visual field, visual acuity, measuring the size of the organ of vision. To be able to examine the fundus of the eye in more detail, the doctor instills drops that dilate the pupil for a short time.
It is recommended to do ophthalmoscopy once every 2 years. But if you are unfavorably prone to glaucoma, this procedure is done more often (ideally, once every six months, so that you can notice the signs of an incipient eye disease as early as possible.
Table of IOP indicators depending on the measurement methods used
It is important to keep the dynamics of intraocular pressure under control in order to promptly detect the development of glaucoma, a disease that causes partial and complete loss of vision.
| Norm | Initial manifestations of glaucoma, stage 1 | Glaucoma, stage 2, moderate | Glaucoma, stage 3 | Glaucoma, end stage | |
| Instrumental method (tonometry) | 10-25 | 24-26 | 26-36 | – | – |
| Computer diagnostics | 10-20 | 21-22 | 22-26 | 26-33 | 33-35 and above |
Using a tonometer, it is not possible to determine IOP in advanced glaucoma. According to medical standards, women over 40 years of age should visit an ophthalmologist to monitor intraocular pressure at least three times a year. Men should make such visits at least twice a year.
It is necessary to take timely measures to normalize ophthalmic tone in order to maintain eye health and visual acuity for a long time.
Reasons for deviation from the norm
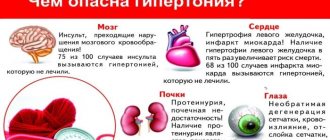
An increase in intraocular pressure occurs due to the influence of such pathogenic factors:
- increased stress on the organ of vision (for example, prolonged viewing of TV shows or reading in poor lighting conditions);
- unfavorable family predisposition;
- pathological changes in the organ of vision;
- diseases of internal organs;
- chemical intoxication;
- imbalance of hormones;
- unfavorable environmental conditions;
- using certain eye drops;
- violation of the integrity of the eye membranes;
- prolonged stress;
- heart and vascular diseases;
- in women – menstrual irregularities, menopause;
- smoking;
- drinking large amounts of alcoholic beverages;
- insufficient intake of vitamins and minerals into the body.
Reasons for decreased IOP:
- hypotension;
- retinal disinsertion;
- inflammation of the iris;
- dehydration;
- keratitis;
- conjunctivitis;
- blepharitis.
If low pressure inside the eye persists for more than a month, the nutrition of the eye may be disrupted, retinal detachment, optic nerve dystrophy and, as a result, complete blindness. The patient needs to urgently come to see a doctor if a halo appears when looking at a bright light.
Symptoms
After 45-50 years, women experience increasing disturbances in blood microcirculation in the eye. There are deviations in the optical properties of the retina. The changes are associated with hormonal characteristics and a lack of estrogen during menopause.
Cases of low blood pressure are less common. A common problem is increased IOP.
The pathology is accompanied by the following symptoms:
- rainbow circles before the eyes, goosebumps when focusing on the light;
- redness of the whites;
- rapid eye fatigue;
- feeling of pain;
- discomfort when reading books, working at the computer, watching TV;
- narrowing of the field of view;
- decreased visual acuity at dusk;
- pain in the temporal part, in the forehead area.
The symptoms of low blood pressure are more expressive:
- dry mucous membranes;
- loss of healthy shine in the eyes;
- prolapse of the eyeball.
The reasons for deviation of IOP from the norm are: age-related changes, congenital pathologies, ophthalmological diseases accompanied by an inflammatory process.
Useful video
These videos provide useful information about intraocular pressure:
Normal eye pressure varies within fairly narrow limits. Any change in it indicates the development of dangerous eye diseases. Timely diagnosis helps to detect them at the earliest stage.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 20 ratings, average: 4.60 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.
Prognosis for recovery and prevention of disorders
Age-related changes are not a menacing fate that hangs over everyone. The patient can take care of himself and prepare in advance for aging. Prevention measures:
- Do daily exercises for the body and eyes;
- if possible, play sports;
- maintain blood vessels in good condition with good nutrition and quality rest;
- give your eyes a rest.
If the first signs of illness have already appeared, you should immediately contact an ophthalmologist and measure your eye pressure. All doctor’s prescriptions must be carried out responsibly, then you will be able to preserve your vision.
Patients over 41 years of age need to annually monitor the dynamics of age-related changes and visit an ophthalmologist. A preventive examination allows you to immediately detect increased eye pressure and take measures to prevent glaucoma and vision loss.