- Why does Crohn's disease occur?
- Signs of Crohn's disease
- What examination is necessary if Crohn's disease is suspected?
- Treatment of Crohn's disease
- Possible complications. Crohn's disease is a precancerous disease
Crohn's disease is a chronic, severe inflammatory disease of the gastrointestinal tract, which can affect any part of it, from the oral cavity to the rectum. Clinically, it is manifested by inflammation of the entire thickness of the wall of the digestive tube, the formation of ulcers and scars.
Crohn's disease in facts and figures:
- In 70% of cases, the pathological process develops in the small intestine, in 25% of cases - in the large intestine, in 5% of cases - in the esophagus, stomach or anus.
- Crohn's disease can begin at any age. Most often - at 20-50 years old.
- Men and women get sick approximately equally often.
- There is no exact data on how widespread the disease is. In the UK there is 1 sick person for every 1500-1800 people.
What is Crohn's disease?
In Crohn's disease, healthy areas of the intestine alternate with inflamed areas. Sometimes the pathological process covers large areas, and sometimes very small ones. Not only the intestines are affected by inflammation, but also the stomach and esophagus, but this does not always happen.
Most patients are diagnosed with damage to the small intestine in the area of the ileocecal canal. Sometimes the disease manifests in the ileum and spreads further. In this case, both the small and large intestines are affected. Its examination allows visualization of ulcers. They differ in shape and size. Healthy areas of the intestine are replaced by areas of stenosis and compaction. However, the structure of goblet cells and crypts is not disturbed.
Pathogenesis
Crohn's disease develops when, under the influence of various factors (hereditary predisposition and genetic mutations, microbial activity and disorders of the immune system), an inflammatory response from the immune system is activated. The action of the immune system leads to damage to the intestinal wall. At the same time, a distinctive feature of the disease is the occurrence of ulcers affecting the entire thickness of the intestinal wall.
Over time, the intestinal mucosa takes on the characteristic appearance of a “cobblestone pavement” - areas of ulcers and cracks alternate with areas of accumulation of immune cells and swelling of the mucous membrane (Fig. 2).
Figure 2. Cobblestone-like changes in the intestinal mucosa in Crohn's disease. Source: aboutkidshealth ca Source: unspecific. ru.
Crohn's disease in adults
Crohn's disease is considered a disease of the young - it affects mainly middle-aged people, with the peak incidence occurring between 15 and 35 years of age. Among the older age group, a second peak is observed - after 60 years.
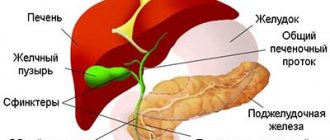
At the same time, the disease has a widespread nature of the lesions - unlike other diseases from the IBD group ("inflammatory bowel diseases"), it can affect any part of the digestive tract, from the oral cavity to the rectum (Fig. 3).
Figure 3. Crohn's disease can affect the entire digestive tract. Source: QuIBDO
Crohn's disease, like many others from the group of autoimmune diseases, has a chronic course - one way or another, once it occurs, it will accompany the patient for many years. However, with proper treatment, the symptoms of the disease can often be minimized.
Crohn's disease in children
The onset of Crohn's disease in children occurs on average at 10-15 years of age. Boys are more likely to get sick. Just like in adults, any part of the digestive tract can be affected in children, but most often the disease occurs in the form of ileocolitis, colitis and ileitis.
Classification
Depending on where the inflammation is concentrated, the following forms of Crohn's disease are distinguished:
- Ileitis (damage to the ileum).
- Ileocolitis (damage to the ileum and colon). This form of pathology is more common than others.
- Gastroduodenitis (damage to the stomach and duodenum).
- Colitis (damage to the large intestine).
- Jejunoileitis (damage to the small and ileal intestines).
Depending on the characteristics of the pathology, acute and chronic forms of Crohn's disease are distinguished.
Forecast
The prognosis of the disease varies significantly and is determined individually. The course of Crohn's disease can be asymptomatic (if the lesion is localized only in the anus in older people) or be extremely severe.
13-20% of patients have a chronic course of the disease. With proper treatment, the duration of periods of remission reaches several decades. As an independent disease, Crohn's disease very rarely causes death in patients, and the mortality rate remains extremely low. Typically, patients receiving maintenance therapy live to a ripe old age.
Author:
Nikita Aleksandrovich Korobov, anesthesiologist
Causes of Crohn's disease
Until now, scientists have not figured out the exact causes of Crohn's disease. There are only a few theories, but none of them are supported by scientific facts, among them:
- Hereditary predisposition.
- Theory of antigen formation.
- Infectious theory.
- Autoimmune theory.
Which one is correct is unknown. Therefore, each of them needs to be considered in more detail.
Theory of antigen formation.
Proponents of this theory believe that antigens from food attach to the intestinal walls. The person's own antibodies react to them. This triggers an inflammatory response in the form of Crohn's disease.
Infection theory
. There are scientists who suggest that Crohn's disease is a consequence of past infections. They believe that pathology is caused by various viruses and bacteria that live in the human gastrointestinal tract.
Autoimmune theory.
Most scientists are of the opinion that Crohn's disease is of autoimmune origin, that is, it develops due to malfunctions of the human immune system. These failures lead to immune cells attacking the intestinal tissues, causing inflammation and destruction.
Genetic factors
. Genetics play a critical role in the development of Crohn's disease. The likelihood of pathology occurring in people with a family history is 10 times higher. Crohn's disease often affects siblings and identical twins.
There is evidence that the probability of developing the disease in a child is 70% if one of the parents suffered from it. Moreover, the symptoms will coincide by 80%.
The likelihood of developing pathology increases in people who smoke and drink, and in citizens living in unfavorable environmental conditions. Frequent stress and chronic emotional stress increase the risk of Crohn's disease.
However, most scientists are of the opinion that Crohn's disease is still of an autoimmune nature.
Symptoms of Crohn's disease
The general symptoms of the pathology are caused by intoxication of the body and deterioration of its resistance.
Crohn's disease can be suspected based on the following signs:
- Chronic fatigue.
- Malaise.
- High body temperature.
- Anemia, blood clotting disorder.
- Abdominal pain, abnormal stool.
These symptoms are characteristic of some other diseases, for example, appendicitis, ulcerative colitis, IBS. Therefore, you cannot try to make a diagnosis yourself. If a person is plagued by cramping abdominal pain that does not stop for 6 hours, you need to consult a doctor.
Local symptoms
Symptoms of Crohn's disease can be both mild and quite intense. Most often, with each period of exacerbation they gain strength. During remission, a person lives a normal life without suffering from any pathological symptoms.
Local manifestations of Crohn's disease:
- Diarrhea. It is stool liquefaction that comes to the fore in patients with Crohn's disease. The process of digesting food occurs with disturbances, the intestines are constantly contracting, so the stool becomes thinner, and the urge to empty the intestines becomes more frequent.
- Increased body temperature, deterioration of health. Most often, the hyperthermic reaction is not too intense; the mark on the thermometer does not exceed 38 °C.
- Abdominal pain, intestinal cramps. Since the intestinal walls become covered with ulcers, and the organ itself becomes inflamed, a person experiences painful sensations. Sometimes they are weak, and sometimes they are very strong. In some cases, the pain is accompanied by nausea and vomiting.
- Blood in stool. Bleeding may be hidden, while blood is present in the stool, but it cannot be seen with the naked eye. If the intestines are severely damaged, blood will be visible.
- Lack of desire to eat, weight loss. A person gradually loses his appetite, which occurs due to persistent inflammation of the gastrointestinal tract.
- Pain in the anal area. It occurs when a person develops a fistula.
- Mouth ulcers.
Extraintestinal symptoms of the disease
Extraintestinal symptoms of Crohn's disease include the following:
- Visual disturbances with the development of keratitis, uveitis, conjunctivitis.
- Skin lesions in the form of pyoderma and erythema nodosum.
- Damage to articular tissues with the development of monoarthritis or spondylitis.
- Stomatitis.
- Disorders of the hepatobiliary system in the form of cirrhosis, fatty liver, cholangiocarcinoma.
- Kidney damage with the development of cystitis, hydronephrosis or pyelonephritis.
- Increased risk of developing cancer, namely colon carcinoma.
Prevention
The disease still remains completely unexplored by doctors. Therefore, in preventive measures, doctors advise listening to your body. Timely treatment will not only eliminate complications, but also reduce the number of relapses.
In order to avoid frequent inflammation, the patient should adhere to the following recommendations:
- diet therapy;
- reduce stressful situations;
- increase rest time;
- lead a correct lifestyle;
- spend time outdoors;
- to refuse from bad habits.
In moments of exacerbation of the disease, you need to seek help from a doctor and follow all his recommendations.
Psoriasis Diabetes mellitus Irritable bowel syndrome Ulcerative colitis of the intestine Intestinal cancer Intestinal dysbiosis
Diagnosis of Crohn's disease
To make a diagnosis, a comprehensive examination of the patient will be required. It is important not only to detect the disease itself, but also to clarify the degree of its development and the activity of the pathological process. This is the only way to select the optimal therapy and improve the patient’s quality of life.
Diagnosis is carried out dynamically, with each episode of exacerbation of the pathology, which will prolong remission. Depending on the results obtained at each specific stage of the disease, the treatment regimen is adjusted.
Anamnesis collection. During your first visit to the doctor, you will need to answer the following questions from the doctor:
- How long ago did the first signs of the disease appear?
- How often does the pathology worsen?
- Is there any relationship between periods of exacerbation and certain events (eating, smoking, taking medications, etc.)?
- How does the person feel at the time of admission?
- Has the disease been previously treated?
When the doctor receives the necessary information, he will refer the patient for testing.
Analyzes.
With the help of tests, it will be possible to understand how much the disease has affected a person’s health. The patient will be required to provide urine, feces and blood. Using a blood test, it will be possible to determine whether there is a decrease in the level of hemoglobin in the blood, whether the value of leukocytes in the blood is increased, and also to determine the ESR.
In addition to a general blood test, a biochemical study is carried out, during which the following values are determined:
- Fibrinogen level (values will be increased).
- Level of gamma globulin fraction (values will be increased).
- Albumin level (values will be reduced).
- The presence of C-reactive protein in the blood (indicates an inflammatory reaction).
- Vitamin B12 and folic acid levels (values will be reduced).
An immunological blood test can detect many immune complexes, as well as a decrease in the number of T-lymphocytes.
A urine test can also determine the stage of development of the disease. If it has an acute course, then protein and blood will be found in the urine. Its analysis also makes it possible to clarify whether the kidneys are involved in the pathological process or whether there is an infection of the urinary system.
Blood, white blood cells, and epithelial cells are found in the stool of a patient with Crohn's disease. Sometimes parasites and bacteria are found in stool. It is good if feces are tested during the acute period of the disease. This way the research will be as informative as possible. To clarify the diagnosis, the doctor can collect tissue from the intestinal mucosa and send it for examination.
Colonoscopy.
This study is carried out using special equipment. A tube with a camera is inserted into the colon, which displays an image on a monitor. This allows the doctor to visualize the condition of the intestines from the inside. If the doctor discovers ulcerative defects or other tissue changes, he takes them and sends them for further examination.
Endoscopy.
This test is prescribed to all patients with Crohn's disease. A tube with a video camera is inserted into the anus or mouth. With its help, the doctor assesses the condition of the gastrointestinal tract.
Endocapsule colonoscopy
. This is a modern study that allows you to assess the condition of the entire digestive tract with maximum comfort for a person. He will simply need to swallow a capsule, which will pass through the intestines, taking a series of pictures. The doctor will only have to study them. This study makes it possible to examine each section of the small intestine, which is impossible with classical endoscopy.
Signs that will indicate Crohn's disease:
- Erosion. They look like small ulcers with scar tissue formed around them. The erosions are surrounded by healthy areas of the intestinal wall.
- Ulcerative defects. They affect the intestines deeper than erosions, sometimes reaching the muscular structures of the organ.
- Swelling of the mucous membranes. Between the ulcers, swollen areas of tissue will be noticeable. Therefore, the intestines from the inside resemble cobblestones.
- Scarring. These inelastic tissues pull the walls of the defects together, thereby narrowing the intestinal lumen.
- Fistulas. They are represented by channels that are formed due to the destruction of organ tissue. Fistulas can connect the intestine to other organs, such as the bladder, or to the external environment, such as the abdominal wall and skin.
X-ray
. During the examination, photographs of the abdomen are taken. This helps prevent colon expansion and intestinal perforation.
Irrigography
. This procedure involves examining the intestines using x-rays, but using a contrast agent. Both air and barium can act as a contrast.
Ultrasound.
The study provides information about the size of intestinal loops and the presence of effusion in the abdominal cavity.
CT and MRI
. These studies are indicated for patients with complicated pathology, when there is a suspicion of damage to other organs. In addition, MRI provides information about the condition of the lymph nodes, the narrowing of certain areas of the intestine, the extent of its damage, and the presence of fistulas.
Biopsy and histology
. A biopsy involves taking the changed organ tissue. The resulting biopsy is sent for histology. The research is carried out in a laboratory where the materials are carefully studied. This will allow the doctor to make the correct diagnosis.
Rule out conditions similar to Crohn's disease
. There are a number of pathologies that may have symptoms similar to Crohn's disease.
Therefore, it is important to carry out differential diagnosis with such disorders as:
- Salmonellosis, dysentery and other intestinal infections.
- Appendicitis.
- Chronic infections of the pelvic organs.
- Celiac disease, in which the human body cannot tolerate gluten.
- Enteritis and chronic non-ulcerative colitis.
- Nonspecific ulcerative colitis. Unlike Crohn's disease, this pathology does not affect the entire intestine.
- Autoimmune diseases: scleroderma and systemic lupus erythematosus.
- Bowel cancer.
Which doctor treats Crohn's disease?
To identify and treat Crohn's disease, you need to consult a gastroenterologist. The doctor will examine the patient and give him a referral for tests and instrumental examination. The doctor will then be able to make an opinion about the person's health status.
Sometimes, to clarify the diagnosis, consultation with specialists such as:
- Immunologist.
It will detect abnormalities in the functioning of the immune system.
- Nephrologist.
Patients with suspected kidney disease are referred to this specialist.
- Hematologist.
The doctor will prescribe a blood transfusion to the patient if necessary.
- Infectious disease specialist.
The specialist is engaged in detecting infectious causes of pathology.
- Dermatologist.
His consultation is needed in case of skin lesions.
A visceral surgeon examines a patient when surgery is indicated. A consultation of specialists can maximize the prognosis of a patient with Crohn's disease.
General recommendations
If a person is overcome by Crohn's disease, then he needs:
- Switch to portioned meals. Eat small meals at least 5 times a day.
- Compose your diet in such a way that the ratio of proteins, fats and carbohydrates does not exceed 150, 70 and 250 grams, respectively. The energy value should not be more than 2100 calories per day.
- Minimize the amount of salt consumed in foods. Or better yet, give it up altogether. The maximum allowable amount is 8 grams per day.
- Eat more foods with calcium and potassium.
- Drink 1.7-2 liters of liquid per day.
- Prepare food by steaming, baking or boiling.
It is also necessary to minimize stress in everyday life and ensure healthy, restful sleep. In case of exacerbation, bed rest is indicated, which is important to observe until the condition improves.
Treatment methods
Treatment of Crohn's disease is based on taking medications. They allow you to relieve the inflammatory reaction, reduce the frequency of intestinal contractions, get rid of stool disorders, reduce cases of exacerbation of pathology, and achieve stable remission.
If the pathology is severe, then serious medications are required. Sometimes in the acute phase of the disease the help of a surgeon is necessary. You can only decide on therapy together with a specialist who knows the patient’s medical history.
There is no specific medicine that could help cope with Crohn's disease once and for all. Therapy must be comprehensive. The sooner it is started, the higher the chances of success.
Main tasks that need to be solved:
- Improve the patient's well-being.
- Reduce pain intensity.
- Get rid of diarrhea.
- Stop blood loss.
- Saturate the body with nutrients.
Anti-inflammatory treatment
. Drugs that are prescribed to relieve the inflammatory reaction vary depending on the characteristics of the pathology.
Sulfasalazine and Mesalazine are taken orally, but they work in the rectum. If the inflammatory process is localized in the small intestine, these drugs will be useless.
Prednisolone and other corticosteroid hormones quickly eliminate inflammation, regardless of where it is concentrated. However, they have many side effects, including: tissue swelling, facial hair growth, sleep disturbance, hypertension, diabetes, osteoporosis, cataracts, glaucoma, decreased immunity. Each patient's body reacts differently to corticosteroids.
Budesonide (Budenofalk) is a latest generation corticosteroid. It has a pronounced therapeutic effect, but at the same time does not cause so many complications. However, the drug does not act along the entire length of the intestine, but only in certain areas of it. Hormone therapy should not exceed 4 months. Otherwise, the treatment will do more harm than good. After completing the course, patients are transferred to small doses of immunosuppressants.
Immunosuppressants.
These drugs reduce the inflammatory response, but this happens at the expense of immune suppression. Sometimes patients with Crohn's disease need to take 2 medications at once.
Drugs that can be used:
- Azathioprine (Imuran) and Mercaptopurine (Purenetol).
It is these medications that are most often used in the treatment of intestinal diseases. However, even their short-term use contributes to the development of such side effects as: decreased bone marrow function, hepatitis, pancreatitis. Long-term treatment increases the risk of lymphoma and skin cancer.
- Infliximab (Remicade), Certolizumab Pegol (Cimzia), Adalimumab (Humira).
These drugs affect a protein called tumor necrosis factor, reducing its activity. Prescribing them to patients with Crohn's disease allows them to achieve stable remission.
Immunosuppressants should be used in the treatment of patients immediately after diagnosis. They are necessarily prescribed to patients with severe pathology. However, tumor necrosis factor inhibitors are not used to treat patients with tuberculosis, viral hepatitis and other dangerous diseases.
- Methotrexate (Rheumatrex).
The drug is used in the treatment of cancer patients, people with psoriasis and rheumatoid arthritis. However, it can achieve remission in patients with Crohn's disease.
- Cyclosporine (Sandimmune Neoral, Ecoral, Panimune Bioral), Tacrolimus (Advagraf, Prograf, Astrograf
XL, Tacrosel).
These drugs are indicated for use by patients with Crohn's disease complicated by fistulas, as well as by those patients for whom classical anti-inflammatory drugs do not help achieve remission. It must be remembered that Cyclosporine can cause a variety of adverse reactions, including damage to kidney and liver tissue. Therefore, drugs based on it are prescribed in short courses. - Natalizumab (Tysabri) and Vedolizumab (Entyvio).
These drugs prevent molecules that are located on the surface of the intestine and integrins (leukocyte molecules) from binding. This prevents an autoimmune reaction, so symptoms of Crohn's disease do not occur. For severe and moderate pathology, Natalizumab is prescribed. Taking it can cause the development of multifocal leukoencephalopathy, which affects the brain, which can even cause a person to become disabled. Therefore, a trial use is required before starting the course. Vedolizumab does not cause the same severe health effects and works the same as Natalizumab.
- Ustekinumab (Stelara).
This drug was developed to treat psoriasis, but research shows that it can treat Crohn's disease.
Antibiotics
. Antibacterial drugs are indicated when the patient develops complications of Crohn's disease, which are accompanied by infection, including abscesses and fistulas. These drugs do not affect the underlying pathology.
More often than others, medications are prescribed such as:
- Metronidazole (Flagyl, Trichopolum, Klion).
In past years, the drug of choice in the treatment of Crohn's disease was Metronidazole. When prescribing it, you need to remember that it can cause muscle pain, numbness, weakness, and tingling in the limbs.
- Ciprofloxacin.
This drug can reduce the intensity of symptoms of Crohn's disease. If there is a need to take antibiotics, then modern medical science recommends giving preference to Ciprofloxacin rather than Metronidazole.
Other medicines
. There are drugs that can improve the quality of life of patients with Crohn's disease and reduce its manifestations.
Such means include:
- Medicines to stop diarrhea.
If it is uncomplicated, then Citrucel can be used. For severe diarrhea, Loperamide or Imodium is indicated.
- Medicines for pain relief.
For Crohn's disease, the analgesics familiar to most people, such as Ibuprofen or Naproxen, are not prescribed, as they can worsen the course of the pathology. Acetaminophen (Tylenol) is used for pain relief.
- Iron supplements for the treatment of iron deficiency anemia.
- Vitamin B12 injections for the treatment of B12 deficiency anemia.
- Vitamin D and calcium supplements. Crohn's disease increases the likelihood of developing osteoporosis. To prevent this from happening, the patient is prescribed vitamins and minerals.
Surgical intervention
Surgery for Crohn's disease is used only when other treatment methods have failed to achieve remission. More than half of patients undergo at least one bowel intervention. Despite this, the possibility of relapse of the pathology cannot be excluded. Therefore, doctors resort to radical methods only in extreme cases.
Laparoscopy is preferred. This minimally invasive procedure is easier to tolerate by patients and does not cause serious complications.
Indications for surgical intervention are:
- Formation of intestinal strictures, which prevents stool from leaving the intestine normally.
- Formation of fistulas.
- Intestinal suppuration.
- Development of intra-abdominal bleeding.
- Formation of a perforated intestinal ulcer.
After the operation, the patient is prescribed medication.
Complications of Crohn's disease, prognosis
Complications of Crohn's disease include the following:
- Anemia.
- Intestinal bleeding.
- Perforation of the intestinal wall.
- Urolithiasis disease.
- Cholelithiasis.
- Formation of an abscess in the intestine.
- Intestinal obstruction.
- Formation of fistulas.
As for the prognosis, it can be made only after a full examination of the patient.
Disability
Disability is given to patients with Crohn's disease when the pathology is severe. To obtain disability, a person will need to pass a commission.
Her verdict could be as follows:
- Assignment of the third group.
It is given to patients in whom episodes of exacerbation of the pathology occur several times a year, there is mild pain, body weight decreases, and only the small or only the large intestine is affected.
- Assignment of the second group.
It is given to patients whose entire intestine is affected. The patient is constantly plagued by pain and diarrhea, fistulas have formed, anemia has developed, the intestines work with serious disturbances, and weight loss occurs.
- Assignment to the first group.
It is given to patients whose weight decreases by more than 30% and who develop disorders of the cardiovascular and endocrine systems. In this case, the intestines must be completely affected, and the person is no longer able to take care of himself on his own.
Sample menu for the week
A sample menu for the week will look like this.
Monday:
- Breakfast: steam cutlet, rice porridge flavored with butter, green tea.
- Second breakfast: biscuits, kefir.
- Lunch: vegetable soup, boiled fillet, cottage cheese casserole, compote.
- Afternoon snack: kefir, toast with pate.
- Dinner: boiled sea fish, pureed buckwheat porridge, rosehip decoction.
- Late dinner: kefir, baked apple.
Tuesday:
- Breakfast: oatmeal, steamed chicken cutlet, weak tea.
- Second breakfast: kefir, fruit jelly, crackers.
- Lunch: soup with meatballs, a few slices of bread, chicken pate.
- Afternoon snack: baked apple, kefir.
- Dinner: steamed omelet, biscuits, juice.
- Late dinner: green tea, homemade pureed cottage cheese.
Wednesday:
- Breakfast: vegetable puree soup, boiled chicken fillet, weak tea.
- Second breakfast: kefir, banana pudding.
- Lunch: baked zucchini, steamed cutlet, grated rice porridge with butter, rosehip infusion.
- Afternoon snack: crackers, jelly.
- Dinner: beef soufflé, grated rice porridge, potato soup, weak tea.
- Late dinner: kefir, baked apple.
Thursday:
- Breakfast: soft-boiled eggs, oatmeal, kefir.
- Second breakfast: biscuits, weak tea.
- Lunch: baked fish, boiled grated vegetables, cottage cheese casserole, rosehip decoction.
- Afternoon snack: jelly, crackers.
- Dinner: rice porridge, steamed omelette, chicken cutlet.
- Late dinner: kefir.
Friday:
- Breakfast: noodles, steamed chicken cutlet, juice.
- Second breakfast: kefir, cottage cheese casserole.
- Lunch: vegetable soup, baked vegetables, boiled fish.
- Afternoon snack: soft-boiled egg, a few pieces of dried bread, weak tea.
- Dinner: rice porridge flavored with butter, chicken soufflé, boiled vegetables.
- Late dinner: kefir, biscuits.
Saturday:
- Breakfast: steamed omelet, dried bread, grated homemade cottage cheese, weak tea.
- Second breakfast: kefir, biscuits.
- Lunch: fish soup, baked vegetables, steam cutlet, rosehip decoction.
- Afternoon snack: jelly, crackers.
- Dinner: steamed meatballs, rice porridge, weak tea.
- Late dinner: kefir, baked apple.
Sunday:
- Breakfast: steamed fish, grated buckwheat porridge, weak tea.
- Second breakfast: fruit jelly, biscuits.
- Lunch: vegetable soup with meatballs, boiled chicken fillet, oatmeal, rosehip infusion.
- Afternoon snack: weak tea, homemade pate, a few pieces of toasted bread.
- Dinner: meat soufflé, grated steamed vegetables, soft-boiled egg, jelly.
- Late dinner: kefir, crackers.
If you wish, you can independently create a sample menu for the week, including only recommended products in your diet. Portions should be small to avoid overeating. In severe cases of Crohn's disease, you must strictly follow the doctor's instructions regarding nutrition, since there are restrictions in the choice of dishes.
Diets for Crohn's disease
There is a theory that Crohn's disease develops due to dietary errors. However, it is unproven, although following a diet may improve the patient's condition. There is no universal nutrition system; it is compiled on an individual basis. It is imperative to adhere to a diet during an exacerbation of the pathology.
Diet options for Crohn's disease:
- High calorie food. It is prescribed to patients who begin to lose weight.
- Low salt diet. It is prescribed to patients receiving hormone therapy.
- Lactose-free diet. It is indicated for patients who are lactose intolerant. They are strictly prohibited from dairy products.
- Low fiber content. It allows you to cope with intestinal obstruction.
- Low fat diet. It is indicated for patients with inflammation in the small intestine, when fat absorption is difficult.
Folk remedies
Traditional medicine suggests using herbs and other plants that can have a positive effect on the severity of the inflammatory process in the digestive tract, as well as on the general condition of the patient. It is worth remembering that Crohn's disease is a serious disease, untimely and inadequate treatment of which can lead to fatal complications. That is why treatment with folk remedies should always be agreed with your doctor.
The following may be used to treat Crohn's disease:
- Infusion of chamomile flowers.
This plant has antispasmodic (eliminates spasm of the intestinal muscles), anti-inflammatory, antibacterial and wound-healing effects. The infusion should be prepared directly on the day of use. To do this, pour 2 tablespoons of raw material into 1 glass of hot boiled water and heat in a water bath for 20 minutes. After cooling, take 1-2 tablespoons orally 3-4 times a day 30 minutes before meals. Also, the resulting infusion can be used for intestinal lavage (in the form of an enema). - Enema with a decoction of marshmallow root.
To prepare the decoction, add 4 tablespoons of crushed raw materials to 1 liter of water, bring to a boil and boil for 3 to 5 minutes, then cool for 2 hours. Use warm to wash the intestines 1 – 2 times a day. It has a local anti-inflammatory effect, which is effective for Crohn's disease of the large intestine. - Infusion of yarrow.
The essential oils and tannins contained in this plant determine its anti-inflammatory, anti-allergic, wound-healing and antibacterial effects, which makes the drug effective both during exacerbation of the disease and during remission. To prepare the infusion, 5 tablespoons of crushed raw materials need to be poured with 500 milliliters of warm boiled water and heated in a water bath (without bringing to a boil) for 15 - 20 minutes. Strain and take 2-3 tablespoons warm 30 minutes before each meal. - Infusion of celandine herb.
When used orally, it has an anti-inflammatory and antibacterial effect at the level of the mucous membrane of the stomach and intestines. It also has a pronounced immunosuppressive and cytostatic effect (that is, it inhibits the formation of leukocytes and their destruction at the site of inflammation, which reduces the activity of the inflammatory process). In addition, it has a certain antispasmodic effect at the level of the muscular layer of the gastrointestinal tract, biliary and urinary tracts. To prepare the infusion, add 4 tablespoons of crushed raw materials to 400 ml of boiled water and heat in a water bath for 15 minutes. After this, cool to room temperature, strain and add another 100 ml of warm boiled water. Take 2 tablespoons orally 3-4 times a day before meals.
Features of Crohn's disease in childhood
In children, Crohn's disease occurs with some features:
- The main symptom is diarrhea.
- There is often no blood in the stool.
- The pain may be mild or very severe.
- The child will lag behind in physical development.
- Children develop arthritis, joint pain appears, erythema nodosum forms, vision deteriorates, and ulcers form in the mouth.
Diagnosis and treatment in children is similar to that in adult patients, but the dosage of drugs is reduced.
Intestinal obstruction
When considering the topic of symptoms and treatment of Crohn's disease, it is necessary to talk about this complication. Intestinal obstruction accounts for as much as 3.8% of all emergencies in abdominal surgery.
This is a serious pathology, manifested in disruption of the movement of semi-digested food masses through the digestive tract.
Obstruction may be small or large intestinal, partial or complete, chronic or acute, acquired or congenital.
Just like many other diseases, it has several stages. In the early stages, a person is only concerned about local abdominal symptoms and pain. Then stool retention, abdominal asymmetry, bloating begin to make themselves felt, and gases stop passing. At the last stage, hemodynamics are disrupted and peritonitis develops. All stages pass very quickly - from 2 to 36 hours.