Scleroderma is a rare systemic disease characterized by thickening, hardening of the skin and connective tissue.
There are 2 types of scleroderma: localized and systemic scleroderma .
Localized scleroderma is an inflammatory sclerotic lesion of the skin without involving internal organs in the pathological process.
Systemic scleroderma affects, in addition to the skin, also internal organs - the heart, alimentary tract, lungs, kidneys.
Scleroderma does not pose a danger to other people; the disease is not contagious. But it significantly reduces the quality of life of the patient himself and poses a direct threat to his life.
All patients with scleroderma should be observed by a rheumatologist. If time is missed, systemic scleroderma can cause numerous complications.
1
Consultation with a rheumatologist
2 Consultation with a rheumatologist
3 Consultation with a rheumatologist
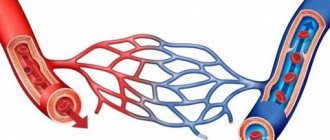
Lack of blood circulation in scleroderma leads to tissue necrosis in the extremities, gangrene and possible amputation of fingers or toes. Damage to kidney tissue is dangerous due to renal scleroderma crisis. Inflammation of the gastrointestinal tract, cardiac complications and pulmonary hypertension are also possible. Only timely, adequate treatment will help maintain health, and in some cases save the life of a patient with systemic scleroderma.
Why does scleroderma occur?
Scientists currently cannot yet accurately answer this question. It is believed that immune disorders, hereditary predisposition, viral infections, and contact with certain substances (pesticides, resins, solvents) play a role.
The appearance of the first symptoms of the disease or the next exacerbation is often caused by injuries, hypothermia, disorders of the nervous and endocrine systems, and vibration (in people who work in production).
Stages and types of scleroderma
This type of scleroderma has 3 stages:
In the first, round bluish-red plaques are formed. In this case, the patient’s skin is swollen, with a doughy consistency.
The second stage begins to develop within a couple of weeks. At this stage hardening occurs. The skin becomes waxy, adheres very tightly to the tissues, the pattern on the skin is smoothed out, hair on the affected area is completely absent, the skin at the site of the disease cannot be collected into a single fold.
At the third stage of the disease, the patient's skin becomes thinner and becomes parchment-like in appearance. This is the stage of atrophy.
There are also several subtypes of limited scleroderma. Linear scleroderma is one of them. It usually appears on the face, directly on the skin of the forehead and scalp. This type of scleroderma looks like the mark of a saber strike. In some cases, the patient may observe linear scleroderma in the chest area, as well as on the lower extremities. This location of the focus of the disease indicates the neurotrophic pathogenesis of the disease. This form of the disease often occurs in children.
Scleroderma can also be expressed in the form of small, round, fairly smooth, sharply defined, shiny spots. The spots have a porcelain-white color and a dense consistency. Most often, white spots are located on the neck, shoulders, genitals, upper chest, and in the mouth. This form of scleroderma is differentiated from lichen planus and leukoplakia.
Superficial scleroderma is another subtype of a limited form of the disease, similar to bluish or brown plaques. The center of the plaques is slightly sunken, and the vessels are visible in it. The patient with superficial scleroderma does not feel much anxiety. Plaques can usually be found on the back and skin of the lower extremities.
Systemic scleroderma is a serious disease that in most cases begins in early or teenage years and is more common in girls. At the very beginning, the disease will affect the patient’s hands and face, and then the disease spreads to the skin of the torso and the skin of the extremities. Foci of the disease gradually increase in size and begin to harden. The affected skin is fixed to the underlying tissues, noticeably changes its color and becomes yellowish. Sometimes vasodilation may occur. The skin is very tense, the mobility of the facial muscles is limited. The inguinal and axillary lymph nodes are enlarged. The initial symptoms of the disease are insomnia, a feeling of numbness in the limbs, and severe tightening of the skin. Then weakness, severe headache, pain in joints and muscles, general malaise appear, and the temperature also rises.
Symptoms of scleroderma
There is practically no organ that could not be affected by systemic scleroderma.
Skin damage begins with swelling on the face and hands, gradually these areas of the skin thicken and acquire a waxy color. Discolored spots appear, devoid of pigment, areas in which the vascular pattern is enhanced. The mouth decreases in size because the thickened skin tightens it like a pouch. The face becomes mask-like, the fingers resemble a dummy. Gradually the process spreads to other areas of the skin.
Scleroderma is characterized by Raynaud's syndrome - whitening and numbness of the skin of the face, lips, hands, and feet as a result of vascular spasm. This usually happens after hypothermia or emotional shock.
Damage to the joints of the hands leads to shortening of the fingers and thinning of their tips. The nails are deformed, and the fingers are constantly bent in such a way that the hand resembles a “bird's paw”.
Myositis (inflammation in the muscles) with systemic scleroderma manifests itself in the form of muscle weakness and impaired movement. The muscles atrophy - they decrease in size, and painful compactions appear in them.
Disorders of the digestive system manifest themselves in the form of heartburn, sour belching, or persistent constipation. Esophagitis (inflammation of the mucous membrane of the esophagus), duodenitis (inflammation of the mucous membrane of the duodenum) develops.
Also, systemic scleroderma can lead to disruption of the heart, lungs, and kidneys. If left untreated, these disorders can become life-threatening over time.
Causes
The main feature of scleroderma is the excessive production of collagen. Collagen is one of the building materials that make up the skin. Excess collagen causes tissue thickening and loss of elasticity.
The underlying cause of scleroderma remains unclear. For some unknown reason, the immune system is turned against the body's tissues and the result is excess collagen production. Currently, research is being conducted to identify the relationship between the immune system, the vascular system and the growth of connective tissue. Studies on twins have shown that there is no genetic factor. And although the cause of scleroderma has not been established, the mechanism of the disease is associated with autoimmune processes in which damage occurs to both the skin and other organs. An autoimmune process triggers excess collagen production, leading to tighter, thicker skin. In addition, changes in connective tissue lead to pressure on the vessels of both large arteries and small ones.
Modern diagnostic methods
The symptoms of systemic scleroderma are many-sided and expressed to varying degrees, so diagnosing the disease is often very difficult. The rheumatologist must carefully examine the patient, evaluate the symptoms, and prescribe a full examination.
All patients are prescribed a general urine and blood test. Breathing tests, ECG, ECHO-cardiography, CT and MRI help to assess the condition of various organs. In the diagnosis of systemic scleroderma, special immunological blood tests are greatly helpful, which can detect rheumatoid factor, antinuclear antibodies, LE cells, and assess antibody levels. If necessary, the doctor will prescribe a biopsy of the skin, muscles or other organs.
Sign up for an appointment with the doctor
Classification
There are three main forms of the disease:
- diffuse;
- limited (localized);
- juvenile scleroderma (manifested before the age of 16 years).
There is also a cross-over form, in which scleroderma is combined with systemic lupus erythematosus, rheumatoid arthritis and other connective tissue pathologies. In 1-2% of patients with scleroderma, the skin is not affected.
In Russia, it is customary to distinguish between the rate of progression and the stage of the disease, which helps in treatment.
Localized scleroderma
It is most often seen on the elbows and knees, but the face and neck may be involved. Internal organs are not affected. The disease has a benign course, involving only the skin. A synonym for this condition is linear scleroderma.
To describe a type of cutaneous sclerosis, the now outdated term “cross syndrome” (CREST) is used - a combination of several of the following symptoms:
- calcification;
- Raynaud's phenomenon (peripheral vascular disease);
- esophageal motility disorders;
- sclerodactyly (changes in fingers);
- telangiectasia (small dilations of blood vessels).
Crest syndrome in scleroderma, although accompanied by some changes in other organs, is a benign form of the disease.
Diffuse scleroderma
It manifests itself as thickening of the skin on the trunk and limbs, above the elbows and knees, as well as involvement of the face. There are rare cases of damage to internal organs typical of scleroderma with unchanged skin.
The systemic nature of the disease is most obvious in the skin, but the gastrointestinal, respiratory, kidney, cardiovascular, endocrine, musculoskeletal and genitourinary systems are also involved.
Treatment of systemic scleroderma
There is no cure for systemic scleroderma. But there are medications that help improve the condition and keep symptoms under control:
- Immunosuppressants are medications that suppress autoimmune processes. This group includes corticosteroids (adrenal cortex hormone preparations) and cytostatics.
- Vasodilators help improve blood flow in affected vessels.
- If the digestive system is affected, the doctor will prescribe medications that reduce the acidity of gastric juice.
- For Raynaud's syndrome, antibiotic ointments are used to protect the skin from infections.
When the exacerbation subsides, the doctor prescribes a course of massage and physical therapy. Rehabilitation treatment is provided to help reduce pain, improve movement in the affected muscles, and restore performance and ability to cope with daily activities.
In severe cases, surgery may be required. If ulcers appear on the fingers and gangrene develops as a result of severe Raynaud's syndrome, amputation is performed. In cases of severe pulmonary hypertension (increased pressure in the pulmonary vessels), the question of lung transplantation may arise.
Timely treatment begins to help maintain performance and the ability to engage in daily activities, improve the quality of life, and avoid dangerous complications. Make an appointment with a specialist doctor by phone: +7 (495) 230-00-01
The material was prepared by oncologist, dermatovenereologist at the Medicine 24/7 clinic, Ekaterina Yuryevna Vertieva.
Vascular damage
Most patients with scleroderma experience Raynaud's syndrome, a severe spasm of the peripheral arteries that is usually localized in the arms. The patient experiences a three-phase change in the skin tone of the fingers.
- First, the patient's fingers turn pale - and the border between the brush of a normal shade and a pathological one is clearly visible.
- Then the fingers begin to turn blue due to poor supply of oxygen and essential nutrients, as a result of which hemoglobin accumulates in them.
- Then redness of the fingers occurs after the elimination of vascular spasm and reactive plethora.
In addition to changes in the color of the fingers, patients may experience numbness or tingling. If the disease is not treated for a long time, it may result in symptoms such as dry gangrene of the fingers, ulcers that do not heal well, and even their death.
Patient reviews
To cope with a disappointing diagnosis, reviews of patients who are receiving treatment and trying to live a normal life will help.
Tatyana M., 45 years old “I suspected something was wrong with my health at an early stage, but I found quite logical excuses for my fatigue and constant weakness: I get tired at work. The medical examination also did not give any answers, since it was casual, and I did not complain about being unwell, but now I regret it. It was necessary to sound the alarm earlier, because the sooner treatment was started, the better. Now I’m trying to monitor myself regularly and monitor the dynamics so as not to completely start the process.”
Vladimir K., 58 years old “It all started with a spot on my leg, with which my wife sent me to the hospital. It turned out that everything was serious. Within a year, joints began to ache, and problems with the functioning of the kidneys and esophagus appeared. I am receiving medication and trying to maintain a healthy lifestyle. But as the doctor said, this is forever, but not a death sentence. Hope for Western progressive treatments may reach us.”
Marina K., 30 years old “I was diagnosed with systemic scleroderma a year ago after giving birth. Today I take hormones and methotrexate. Until the weakness passes, there is just a constant feeling of weakness. Tell me, who is being treated with what? Maybe the doctor chose the wrong drugs?”
Systemic scleroderma is a dangerous autoimmune disease that manifests itself not only by damage to the skin, but also by negative changes in internal organs. Timely detection of disorders and comprehensive treatment can alleviate the patient’s condition, slow down degenerative processes, and prevent serious consequences in the form of disability. Therefore, it is recommended to consult a doctor when the first signs of a disorder appear.
General information
Scleroderma is a systemic disease of connective tissue, so it is characterized by gradual progression with clinical manifestations in the form of damage to the epidermis, malfunction of internal organs and the musculoskeletal system. Its characteristic feature is a cascade of circulatory disorders, inflammation and generalized fibrosis.
The disease is not considered common, since an average of 30-150 cases are registered per million people per year. The diagnosis is given to people from different age categories, including young teenagers and children. But most often older women suffer, since it occurs 7 times more often in them than in men. The prognosis always depends on the severity of the pathology and the age of the patient.
Lifespan
The prognosis for patients after detection of systemic scleroderma is not encouraging, since in the diffuse form the average life expectancy after the start of treatment is 5 years. More favorable assumptions are made by doctors and the limited form or chronic course of the disease. In this case, planning a pregnancy with normal delivery is allowed. The prognosis for them is from 10 to 15 years. Patients need to register with a dispensary and undergo regular examinations every 3-6 months.