What is endocervix
The inner lining of the female genital tract is lined with columnar epithelium, which produces mucous secretion. The part that covers the cervical canal is called the endocervix (from the Greek endon - inside and the Latin cervix - neck).
This layer of cells has characteristics: the thickness of the endocervix, as well as the amount and viscosity of mucus, directly depend on the woman’s hormonal background.
Normally, the endocervix undergoes cyclic changes; it either becomes thinner or thickens depending on the phase of the menstrual cycle, during pregnancy, after childbirth, or abortion.
This restructuring of the mucosa in women who have given birth multiple times often contributes to the formation of an endocervix cyst on the cervix - a small cavity with gel-like contents.
Most cysts that form in the cervical canal are small and not cause for concern. The most vulnerable place is the transitional epithelium at the border of the canal and the cervical pharynx, which is often injured during childbirth.
An endocervix cyst can also form as a result of various diseases that lead to the development of multiple endocervix cysts on the cervix - cavities, also called nabothian vesicles.
They are formed as a result of blockage of the gland ducts, most often with fragments of exfoliated mucous membrane during endocervicitis.
A cyst formed in the endocervix, as a rule, does not resolve and requires observation and treatment.
The cervix with the presence of multiple endocervical cysts can become a serious threat to women's health.
However, the issue of cervical canal cysts remains controversial, it all depends on their cause and clinical manifestations.
Nabothian cyst: MRI
Magnetic resonance imaging is the most informative method for studying tumors in the nabothian glands. Indications for the examination are:
- Difficulties in establishing a diagnosis based on examination, laboratory tests and ultrasound.
- Inconsistency between the clinical picture of the disease and the data obtained as a result of previously conducted examinations.
- The need for a comprehensive study of the genitourinary system for the spread of infectious and inflammatory processes.
To obtain reliable examination results, the patient must:
- 2-3 days before the procedure, avoid gas-forming foods.
- Do not eat at least 4 hours before your scheduled test.
- Do not empty or overfill the bladder. The best option is a half-filled bubble.
- The examination of the reproductive system organs is carried out from the 7th to the 13th day of the menstrual cycle.
Symptoms
In most women, cysts in the cervical canal do not manifest themselves in any way, and only when they reach large sizes do the following symptoms appear:
- menstruation irregularities;
- bleeding;
- foreign body sensation;
- pain in the lower abdomen;
- impossibility of conception.
Menstrual disorder
Large formations narrow the cervical canal, preventing the free flow of menstrual blood. This leads to a delay in menstruation, the appearance of pain in the lower abdomen, an enlarged uterus, and the development of endometritis.
Bleeding
A slight discharge of blood after sexual intercourse or a visit to the gynecologist is typical, especially when it is located in the area of the posterior lip of the cervix, where there are more blood vessels.
Foreign body sensation
With large cysts, a woman experiences a feeling of a foreign object, especially during sexual intercourse or douching.
Pain syndrome
Pain in the lower abdomen is a characteristic sign of large formations on the cervix; they are often accompanied by bloody discharge.
Infertility
If large or multiple bubbles completely cover the lumen of the cervical canal, conception becomes impossible and infertility occurs.
In the photo on the left is the cervical canal, on the right is the appearance of the cyst during colposcopy.
Causes
There are many reasons leading to the formation of endocervical cysts, these include:
- Inflammatory process of the genital tract.
- Cervical erosion.
- Leukoplakia.
- Ectopic epithelium.
- Endometriosis.
- Damage to the mucous membrane.
- Urogenital infections.
- Acute viral infections.
Inflammatory diseases
Any inflammatory process of the female reproductive system can lead to the development of a cyst in the endocervix area on the cervix: colpitis (inflammation of the vagina), endocervicitis (inflammation of the cervix), endometritis (inflammation of the uterine mucosa), salpingo-oophoritis (inflammation of the ovaries and fallopian tubes).
Erosion
During the period of healing and scarring of erosion, the ducts of the endocervix glands may narrow, which leads to the accumulation of secretions, overflow and the formation of retention cysts (from the Latin retentio - delay).
Leukoplakia
This disease is characterized by keratinization of the epithelium, the formation of plaque in the form of white crusts that close the ducts of the glands and make it difficult for mucus to escape.
Ectopia
Atypical growth of the epithelium of the cervical canal into the vagina or, conversely, the so-called reflux of cells leads to blockage of the mucous glands and the formation of cavities.
Endometriosis
One form of endometriosis is endomyosis, when the lining of the uterus grows inside its body, including the cervix. When the ducts of the endocervix are compressed, the outflow of mucus is disrupted and cavities are formed.
Injury
Any damage to the mucous membrane of the cervix can lead to the formation of nabothian vesicles: during childbirth, abortion, as well as from an intrauterine device and chemical contraceptives.
Acute viral infections
The most dangerous are human papillomavirus and cytomegalovirus; they are activated against the background of weakened immunity, penetrate the cells of the mucous membrane, and destroy them.
Urogenital infections
Sexually transmitted infections are a common cause of cysts. These include: syphilis, gonorrhea, trichomoniasis, ureaplasmosis, chlamydia, HIV infection. All of them have a damaging effect on the mucous membrane.
Diagnosis
The presence of pathology is easy to diagnose in a gynecologist’s office - when examined using a mirror.
The second diagnostic method is cervical colposcopy. Using a special optical device, the gynecologist can magnify the area being studied several times. The device can capture images in the form of photos and videos. This will help control the progression of the disease. Also during the procedure, a smear is taken and a biopsy (tissue sampling) is done to study the nature of the changes in the tissues.
One of the diagnostic methods is cervical colposcopy.
To clarify the reasons for the formation of a cyst, they may prescribe:
- Ultrasound of the pelvic cavity;
- general analysis of blood and urinary composition;
- STD tests;
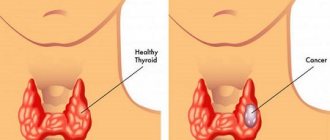
- tests for levels of progesterone and prolactin, estrogen and thyroid hormones;
- oncology analysis;
- bacterial culture (examination of the bacterial composition of the vagina and cervix);
- cytological analysis;
- collection of tissue from the affected area (histological analysis).
After identifying the provoking factors, the doctor decides to start therapy.
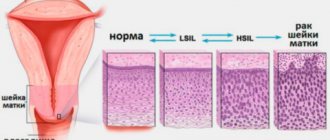
Classification
The classification of nabothian vesicles is of great clinical importance; they are distinguished by two characteristics: number and size.
By quantity they distinguish:
- single endocervix cysts - formed closer to the entrance to the cervical canal, larger in size, more often giving symptoms and leading to complications;
- multiple endocervix cysts are small in size, can be located along the entire cervical canal and remain unnoticed for a long time.
There are three groups of formations based on size:
- small, the size of which does not exceed 3 mm;
- medium - 4-10 mm in size;
- large – more than 10 mm.
Small cysts are more often formed after birth trauma and during the treatment of erosion, when the healing process is underway. They can be located along the entire canal with excessive function of the mucous glands of a hormonal nature.
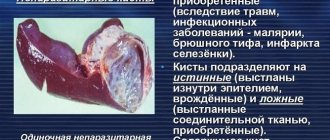
Types of cystic formations of the cervix
The cervix can become the site of the formation of two types of cysts, namely retention (nabothian) and endometrioid. The structure of a retention cyst is an enlarged cervical gland, the duct of which is blocked, and a mucous secretion accumulates inside. Nabothian cysts are quite common - they are diagnosed in 10-15% of patients of reproductive age, more often in those who have already given birth.
Prolapse and prolapse of the cervix: causes and methods of treatment
Endometrioid cysts form as a result of the progression of endometriosis, which has affected the vaginal portion of the cervix. Cystic formations of this kind are combined with heterotopias located in other locations.
Cysts are also classified according to the site of formation. According to this criterion, paracervical (location is the vaginal portion of the cervix) and endocervical (location is the cervical canal itself) cysts are distinguished. In addition, single and multiple cystic formations are distinguished. The size of the cavities most often does not exceed 1 cm, but there are also larger ones - 3 cm or more.
According to the method of formation and etiology, cystic formations are:
- traumatic;
- tumor;
- parasitic;
- inflammatory;
- dysontogenetic;
- retention.
Diagnostic methods
Most endocervical cysts are an incidental finding during a gynecological examination: colposcopy, ultrasound or tomographic examination.
To identify their nature and cause, an additional examination is prescribed, which includes:
- video colposcopy – an extended examination of the vagina and cervix using an optical apparatus with a magnification system;
- hysteroscopy - examination of the inner surface of the uterus, assessment of the condition of the endometrium, detection of endometriosis;
- ultrasound examination, which allows you to determine whether the wall and size of the uterus are normal, to identify deviations in the structure of the endocervix;
- cervical smear for oncocytology;
- research for urogenital infections, the most reliable are polymerase chain reaction (PCR), immunofluorescent analysis (ELISA);
- laboratory test: clinical blood test, urine test, test for HIV infection, Wasserman reaction.
In doubtful cases, a high-precision tomographic examination is additionally prescribed - magnetic resonance imaging (MRI), positron emission tomography (PET).
Ultrasound
Echography (sonography, ultrasound) is based on the property of living tissues to reflect ultrasonic waves. The denser the fabric, the less it absorbs and the more it reflects waves; on the display device it will have a light, white color (echo-positive).
If there are cavity formations, they absorb more ultrasound and reflect little.
This means that when examining the endocervix, cysts will appear on the display as black areas (echo-negative); they are usually round in shape, up to 3 mm in diameter, but the sizes can vary from 1 mm to 2 cm.
The second important echo sign is the heterogeneity of the structure of the endocervix; this is reflected on the display as an alternation of light and dark areas, that is, normal tissue and cavities.
Hysteroscopy
Endoscopic examination of the uterine cavity is an informative study based on fiber optic technologies.
A flexible fiber light probe with a miniature video camera is used to examine the entire inner surface of the uterus.
The study is painful, carried out under short-term anesthesia, in doubtful diagnostic cases.
For example, when an ultrasound shows signs of endomyosis and suspicion of cystic formations of the uterine cavity, as well as frequent bleeding of unknown etiology.
Hysteroscopy allows you to determine the pathology of the uterus, which is the cause of damage to the cervical canal.
Nabothian cysts: ultrasound
Ultrasound examination is a common method necessary to confirm or refute the diagnosis of Nabothian cyst (ultrasound photos clearly determine not only the size of the cavities, but also their number). The examination is prescribed after a gynecological examination and collection of biological material for laboratory research, and is carried out to study:
- Structural features of the epithelium.
- Features of blood circulation.
- Features of the vaginal microflora.
A Nabothian cyst is visualized on ultrasound as a thickening or focal compaction of the epithelium of the cervical canal, accompanied by its slight and uneven expansion. During inflammatory processes, hypertrophy and increased echogenicity of the uterus are determined echographically.
The procedure itself has no special features and can be performed either transabdomitally or using a transvaginal sensor. The differences between the listed methods are that in the first case, ultrasound waves are directed through the anterior wall of the peritoneum, in the second - through the vagina. The fact is that transabdominal examination cannot always obtain a complete picture of the disease, but a transvaginal sensor can detect even the most minor pathologies.
In addition, examination through the anterior wall of the peritoneum involves preparing the patient, namely:
- 3-4 days before the study, the woman needs to give up gas-forming products.
- 1-2 days before the procedure, the patient is recommended to start taking activated charcoal.
- The subject should not eat immediately before the ultrasound.
- Immediately before the procedure, the woman needs to drink 1 liter of water to fill the bladder.
Ultrasound examination is a fairly accurate method that allows you to diagnose a Nabothian cyst (ultrasound photos in both black and white and 3D (4D) versions can be viewed on the Internet). However, in some cases, the results of this procedure can be double-checked using a magnetic resonance imaging scanner.
Methods of therapy
The question of whether cysts need to be treated and with what methods is decided strictly individually.
If in women who have given birth and do not have any complaints, small formations are identified in the endocervix area and the examination did not reveal pathology, then they are limited to regular observation.
If Nabotian vesicles increase, they are subject to treatment, as well as medium-sized and large-sized formations that have clinical manifestations.
Today, more and more specialists consider these as a potential threat to a woman’s health and adhere to more active tactics.
Infectious agents can accumulate in the mucous secretion of the vesicles, which, when the immune system is weakened, make themselves felt, causing an inflammatory process.
Treatment of endocervical cysts combines two methods - surgical and conservative. Various methods are used for removal:
- opening or piercing - performed when the location of the formation is accessible;
- cryodestruction (removal by freezing using liquid nitrogen) – used for a hard-to-reach location in the lumen of the cervical canal;
- radio wave coagulation (cauterization) is an effective method, but painful and requires anesthesia;
- Laser destruction is a very accurate, painless and effective method, but is used to a limited extent, only in external locations close to the vagina.
Sometimes there is a need for surgery when the entire cervix is affected by cysts, or there is pathology of the uterus (fibroids, endomyosis) and its appendages (inflammatory, tumor process). The uterus, cervix and appendages are removed.
Conservative treatment
There are no medications that would effectively act on the endocervix and help get rid of cysts located in the cervix. Conservative measures are an addition to surgical treatment and are aimed at eliminating or preventing complications, these include:
- Relieving inflammation and pain.
- Impact on pathogenic microflora.
- Restoration of damaged tissues.
- Improving metabolic processes.
- Boosting immunity.
Medications
To eliminate inflammation and pain, non-steroidal anti-inflammatory drugs are used: Paracetamol, Ibuprofen, Ketoprofen, Butadione, Nise and their analogues.
To eliminate pathogens, antibiotics, antifungals, and antivirals are used, depending on what microflora is identified in the patient.
Antibiotics are selected with a wide spectrum of action, in accordance with the sensitivity of bacteria to them (Amoxiclav, Cefotaxime, Sumamed, Ciprofloxacin and others).
Antibacterial drugs and antiseptics are also prescribed locally in the form of vaginal tablets, suppositories, ointments, and bath solutions (Metronidazole, Hexicon, Betadine, Polygynax suppositories).
To restore tissue and eliminate the side effects of antibacterial agents, antihistamines are prescribed: Loratadine, Cetirizine, Fenkarol, Erius.
In order to improve the processes of cellular metabolism, vitamin and mineral complexes are prescribed: Multitabs, Vitrum, Undevit, Complivit, Centrum and their analogues.
To increase resistance to infectious agents, immunomodulators (Echinacea, Cat's Claw, Ginseng, Interferon, Amiksin) are prescribed.
The choice of a drug from any of the listed groups should only be made by a doctor on an individual basis.
Treatment of cervical retention cysts
Gynecologists at the Yusupov Hospital take an individual approach to the choice of management tactics for patients with nabothian cysts. If a cyst is found in a woman under 45 years of age, surgical intervention is required. If there is an asymptomatic cervical cyst measuring less than one centimeter in diameter, a wait-and-see approach is followed. Such cysts do not transform into a malignant tumor, do not grow and do not cause discomfort.
To relieve swelling, pain and other signs of inflammation, patients are prescribed Dicloberl vaginal suppositories. Sometimes treatment is carried out with ichthyol ointment. This method has been used for a long time, but it is not always effective. Tampons are moistened in ichthyol ointment and placed in the vagina for 10-20 minutes. They have anti-inflammatory and anti-edematous effects. In the presence of accompanying microflora, ichthyol destroys microorganisms and prevents septic complications. Conservative treatment methods are used as symptomatic therapy, which affects the development of the cyst. If a cervical cyst is accompanied by severe symptoms, gynecologists at the Yusupov Hospital perform surgery with removal of the lesion and further symptomatic therapy.
The following methods of surgical treatment of cervical cysts are used:
- Surgery;
- Electrocoagulation;
- Cryocoagulation;
- Laser vaporization;
- Radio wave therapy.
Surgery involves puncturing the cyst with a needle and aspirating the contents. The operation in the presence of large cysts is performed under ultrasound guidance. This is a fairly simple method, but when used there is a risk of developing infectious complications. Electrocoagulation, cryocoagulation, laser vaporization, radio wave therapy are methods in which doctors use the physical properties of electric current, liquid nitrogen, laser and radio waves to remove the cyst. These methods are less invasive than puncture, but technically more complex. The presence of special equipment and work experience allows doctors at the Yusupov Hospital to widely use them in clinical practice.
Diathermocoagulation. The method has long been used in gynecological practice and has 2 main methods of administration:
- Contact - in this case, the device has direct contact with the neoplasm tissue, or the nozzle is embedded into the thickness of the tissue;
- Non-contact – involves the presence of a micro-arc, which cauterizes the cyst at a certain distance and does not require contact with the tissue.
The advantage of this method is the ability to study the pathological focus, as well as complete excision of pathological tissue.
Unfortunately, the risk of recurrence of a cervical cyst when removed using diathermocoagulation is quite high.
Chemical removal. Removing a cervical cyst using a chemical method involves using a special solution. In our country, the most prominent representative is solkovagin. It contains a set of strong acids: nitric and acetic.
To carry out the procedure, the vagina and cervix are wiped with a tampon soaked in saline solution. Then the mucous membrane is anesthetized with local anesthetics and a tampon soaked in the vagina is applied. Leave for a certain period of time, and then wipe with a clean swab.
The disadvantage of this method is that it cauterizes the entire surface of the vaginal part of the cervix, and not just benign neoplasms.
Cryodestruction. This method is part of the chemical effect. But it has long been separated into a separate technique. In this case, a special gun with liquid nitrogen is used. It freezes modified tissues, which promotes their death. This happens because sudden exposure to cold temperature provokes a stoppage of blood circulation in the cyst with the formation of ice crystals in the capillaries and vessels. They destroy the tissue from the inside.
Removal of a uterine cyst (on the vaginal part of the cervix) does not require additional pain relief, since liquid nitrogen also blocks the conductivity of nerve receptors, which ensures a complete absence of pain.
Laser therapy. This is a relatively new method of combating benign tumors, which is one of the most optimal at the moment.
Laser treatment is permitted for young patients who have not yet given birth. When the indication for other methods is a history of childbirth.
The technique is quite painful, so before the procedure, the vagina and cervix are treated with a local anesthetic, and conduction anesthesia is also administered.
In this case, the risk of bleeding is reduced to zero, since laser radiation coagulates damaged vessels during cauterization.
The development of nabothian cysts on cervical erosion is common. Therefore, similar cauterization methods can be used simultaneously for erosion and cervical cysts.
Cauterization of the cervix usually precedes surgery, but what to do first is up to the attending physician.
The presence of special equipment and work experience allows doctors at the Yusupov Hospital to widely use them in clinical practice.
Complications
Despite the apparent harmlessness and benign nature of endocervical cysts, they can pose a risk of developing a number of complications, such as:
- formation of a permanent focus of infection, maintenance of the inflammatory process;
- suppuration, abscess formation;
- obstacle to conception;
- complication during childbirth as a result of impaired cervical dilatation;
- rupture during pregnancy, which can cause miscarriage;
- cervical ruptures during childbirth.
It is believed that Nabothian cysts are a background pathology that creates favorable conditions for the development of cervical cancer.
How to detect the disease
Treatment of cervical cysts is prescribed only after a complete examination of the patient and an accurate diagnosis. Since the disease is often asymptomatic, women do not go to the doctor. The pathology is detected accidentally during a routine gynecological examination. In the speculum, Nabothian cysts are visible as yellow or white round formations. Endometriosis is identified by its characteristic dark red color.
Other research methods:
- Oncocytology test to assess the condition of the cervix;
- Examination for infections to identify the cause of nabothian cysts and concomitant cervicitis;
- Ultrasound of the cervix;
One of the methods for examining the cervical canal is transvaginal ultrasound.
- Colposcopy with biopsy of suspicious areas.
According to indications, hysteroscopy with curettage of the cervical canal is performed.
Prevention
Preventing the formation of endocervical cysts is quite realistic and accessible. You need to be careful about your health and adhere to the following rules:
- avoid infection by following the rules of safe sexual intercourse;
- promptly treat inflammatory diseases;
- do not use intrauterine devices;
- avoid termination of pregnancy;
- support the immune system: give up bad habits, eat well, move more;
- Visit your gynecologist regularly.
“It is not always in the power of a doctor to heal a sick person” - this phrase said by the ancient Roman philosopher Ovid has not lost its relevance.
However, preventing gynecological diseases is “in the power” of any woman.