Clinical (obsolete - general) blood test is a laboratory diagnostic method most often used in medical practice. Based on the results of this study, it is possible to assess the functional state of the hematopoietic system, as well as confirm or exclude some diagnoses.
Determining the WBC level is one of the important indicators in a general blood test
A clinical blood test (BAT) determines the amount of formed elements, as well as their ratio to plasma. In addition, HOW shows some specific indicators (ESR, hemoglobin). A very important parameter is the leukocyte formula. It determines the quantitative characteristics of various forms of leukocytes.
HOW indicators are denoted by the following abbreviations:
- RBC (red blood cells) – red blood cells;
- HGB (Hb) – hemoglobin;
- MCV – average volume of one red blood cell;
- HCT (Ht) – hematocrit;
- PLT (platelets) – platelets;
- WBC (white blood cells) – leukocytes;
- EO (eozynofile) – eosinophils;
- BA (basofile) – basophils;
- LYMP (lymphocytes) – lymphocytes.
After decoding, it becomes clear what WBC is in a blood test. The abbreviation WBC for white blood cells has been used since the introduction of international standards in all laboratories. Modern hematology analyzers issue forms with encrypted indicators.
Monocytes produce biological active substances: enzymes, complement proteins, coagulation factors.
The study of the number of leukocytes plays an important role in the process of diagnosing infectious, allergic and lymphoproliferative diseases. For healthy people, KAC is indicated at least once a year. This approach is due to the high screening value of the study.
What is WBC indicator
WBC in a blood test is a value that provides a real opportunity to detect an inflammatory process, infectious disease or allergic reaction in time; sometimes it helps to notice neoplasms at the very beginning of their development.
This is one of the main values in a general blood test. Often, together with it, the amount of other blood cells and specific indicators is determined. General analysis is also called clinical analysis.
When conducting this study, the following is determined:
- The number of red blood cells (erythrocytes), abbreviated RBC.
- Hemoglobin concentration in a specified blood volume (HGB or Hb).
- Mean erythrocyte cell volume (MCV).
- The number of platelets, called platelets (PLT).
- White blood cell (WBC) count.
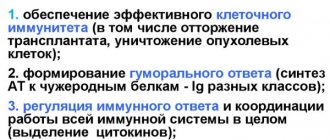
The figure describes the functions of WBC and their norm in a blood test.
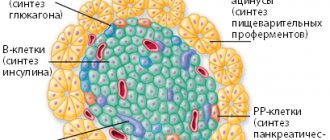
Leukocytes are divided into 5 groups, and each of them is responsible for a specific job of neutralizing foreign bodies that have entered the blood.
During the research, the quantity of each species is determined. In a cubic millimeter of blood under normal conditions there are from 6 to 8 thousand white blood cells.
Basophils
Basophils, or mast cells, are a type of white blood cell responsible for the release of histamine, that is, a hormone that provokes an allergic reaction in the body. Their normal content is from zero to one percent. Basophils in the blood increase in the presence of allergic diseases, chronic myeloid leukemia, megakaryoblastic leukemia, systemic mastocytosis, Hodgkin's disease, and a number of infections, for example, tuberculosis, chickenpox, and influenza. A reduced content of basophils indicates acute infection, anaphylactic shock, hyperthyroidism, and bronchial asthma.
So, let's look at the normal WBC indicators. We explained what it is in the blood.
How and under what conditions are leukocytes produced?
Blood cells that recognize and eliminate foreign elements are called leukocytes. These are special elements of the immune system that are responsible for protecting against pathogenic bacteria and viruses, foreign bodies, any objects that can cause harm, and cleanse it of dead or damaged own cells.
The term “leukocytes” is formed from a combination of two words from the ancient Greek language: “leukos” (white) and “cytos” (receptacle, body).
There are several types of such cells:
- Neutrophils make up 55% of the total. Protection against bacterial and fungal infections depends on them.
- Basophils (0.5%) are scout cells; they find even single foreign elements. Their job is to increase blood flow, mobilize other cells to the site of inflammation, and fight allergens.
- Eosinophils (2.5%) are part of the innate immune system that protects against allergens, parasites, and helminths.
- Monocytes (5%) are responsible for the absorption of dangerous particles and dead cells.
- Lymphocytes (35%) support general immunity, store hereditary information, and regulate the functioning of other types of immune system elements.
White blood cells are produced by red (blood-forming) bone marrow. This organ is located in the internal cavities of the pelvic bones, sternum, and in the end sections of the tubular bones. It is also found inside the vertebrae, but in smaller quantities.
Hematopoietic bone marrow is the only source of cells called stem cells. Their main advantage is that they are close in structure to embryonic ones. The lifespan of leukocyte cells ranges from several hours to several years, depending on the type of leukocyte.
Some leukocytes capture and digest any foreign microorganisms and dead own cells, some produce antibodies that destroy all kinds of pathogens (disease-causing microorganisms) or accelerate blood flow to the necessary places. White blood cells are capable of accumulating hereditary memory, that is, “children” retain information about the threats that their “parents” had to face.
Causes of reduced lymphocyte levels
If the level of lymphocytes is low (less than 15%), then this is provoked by the following factors:
- Aplastic anemia is a bone marrow pathology.
- AIDS.
- Rapidly developing neoplasms.
- Adrenal hyperactivity.
- Pathologies of the nervous system.
- Sclerosis.
- Myasthenia gravis is an autoimmune disease that causes muscle weakness due to disruptions in neuromuscular transmission.
- Guillain-Barré syndrome is the human immune system that destroys its own cells – neurons.
- Taking medications from the steroid group.
WBC indicator table is normal
WBC in a blood test is a kind of description of the immune system in digital terms. Age has the greatest impact on white blood cell levels. In youth, the number of white blood cells in different sexes is almost the same.
Over time, the indicator decreases, as the effect of the immune system gradually deteriorates, and a difference appears in the number of leukocytes in women and men. On average, the leukocyte content is considered to be from 4 to 9.0 x 10 9/l.
| Age | Norm (x 10 9/l) | ||
| Children and teenagers | newborns | 5,5 — 12,5 | |
| up to 1 year | 6,0 — 12,0 | ||
| from 1 to 6 years | 5,0 — 12,0 | ||
| from 6 to 12 years | 4,5 — 10,0 | ||
| from 12 to 15 years | 4,3 – 9,5 | ||
| Adults | women | from 16 to 21 years old | 4,5-11,0 |
| approximately 40 to 60 years | 3,98-10,5 | ||
| over 60 years old | 3,7-9,0 | ||
| men | from 16 to 21 years old | 4,5-11,0 | |
| approximately 40 to 60 years | 4,2-9,0 | ||
| over 60 years old | 3,9-8,5 | ||
The WBC indicator for pregnant women is compared with other values. During this period, the woman's immune system is activated to protect not only her, but also the unborn child. In the first trimester, the values coincide with the standard ones, and then the number of white blood cells begins to increase and reaches 10-15 billion per liter of blood.
ESR (ESR) – ERYTHROCYTE SEDIMENTATION RATE
Norm ESR (ROE)
Women 12.0 - 20
mm/h Men
1.0 - 17
mm/h
For expectant mothers
During pregnancy, ESR can reach 20 – 30 mm/h.
Leukocytes - increase to 15 x 109/l.
These physiological deviations do not contradict the norm!
An important indicator—reflects the ability of red blood cells to settle or stick together. The mechanism of erythrocyte sedimentation has not been precisely established. It is known that the process depends on the size of the red blood cell, its bioelectric charge and the speed of blood flow. The main factor influencing ESR is the biochemical composition of blood plasma
ESR fluctuations:
- from 20 to 30 mm/hour – immunity in tension (after surgery, illness). Indicator of the presence of indolent infection.
- 30 mm/hour and above – possible acute inflammation, an autoimmune process. This is a good reason to go to the doctor.
Read more: ESR - the norm in the blood of women, reasons for the increase
Symptoms of high and low WBC
WBC in a blood test is a number that can be used to fairly accurately assess the functioning of the immune system and overall health. A high value, above the upper limit of normal, is called leukocytosis. This is a signal about inflammatory processes occurring in the body or a decrease in general immunity.
Leukocytosis is not necessarily associated with disease. An increase in the indicator may also depend on heavy physical activity or stress. A small jump also occurs after eating and in women during pregnancy.
Symptoms of leukocytosis:
- causeless fatigue, lethargy;
- temperature increase;
- bruises or hematomas even with minor bruises, and sometimes for no reason;
- pain in the limbs or abdomen;
- decreased appetite and weight loss;
- labored breathing.
A low level of white blood cells is called leukopenia. The danger of this condition is that it does not have pronounced symptoms. Signs of the disease in the initial stage are easily confused with ordinary fatigue.
At a later stage, the following are observed:
- high temperature, chills;
- accelerated pulse;
- causeless anxiety;
- headache;
- exhaustion of the body;
- pneumonia, blood infection.
Swelling of the glands, enlargement of the spleen or tonsils is also possible. If leukopenia develops as a result of taking medications, then the onset of symptoms is explosive.
Increased values
An increase in the volume of white blood cells in the blood is called leukocytosis. There are physiological leukocytosis (occurs in healthy people in some situations) and pathological leukocytosis (indicates the development of diseases).
Possible reasons
A physiological increase in leukocytes in the blood occurs in the following conditions:
- a few hours after eating food;
- after psycho-emotional stress;
- after excessive physical exertion;
- after taking a cold or hot bath;
- in women before menstruation;
- in the second half of pregnancy.
In this regard, it is recommended to take a blood test in the morning on an empty stomach, avoiding significant physical and emotional stress the day before.
According to the WBC blood test, leukocytosis is a symptom of the following diseases:
- infections of various nature;
- meningitis is an inflammatory process of the membranes of the brain and spinal cord;
- erysipelas;
- otitis;
- bronchitis, pneumonia;
- inflammation of the subcutaneous tissue - abscess, phlegmon, panaritium;
- inflammation and suppuration of the abdominal cavity - appendicitis, peritonitis;
- acute pancreatitis;
- leukemia (tumor diseases);
- diabetic coma;
- chronic renal failure;
- heart attacks;
- traumatic tissue damage;
- eclampsia;
- uremia;
- thyroid diseases;
- acute bleeding.
Reasons for increasing and decreasing the WBC indicator
Leukocytosis is observed when:
- sepsis, purulent processes;
- acute inflammation;
- infections caused by viruses, bacteria, fungi or any other pathogens;
- malignant tumors;
- heart attack;
- various tissue injuries;
- in the last trimester of pregnancy;
- after childbirth, during breastfeeding;
- after vigorous physical activity.
A decrease in the WBC parameter can be caused by taking certain antibiotics, drugs from the sulfonamide group, non-steroidal anti-inflammatory drugs, drugs for epilepsy or to relieve spasms, and hormonal medications.
Leukopenia is observed when:
- hereditary pathologies that provoke underdevelopment of tissues or organs (bone marrow hypoplasia) or the absence of an organ or part thereof (aplasia);
- radiation sickness;
- damage to the bone marrow when taking certain medications or other chemical effects on the organ;
- acute intestinal infections (typhoid fever, paratyphoid fever and other types of typhus);
- viral infection;
- anaphylactic shock;
- metastases affecting the bone marrow;
- Addison-Beermer disease (pernicious anemia or malignant anemia);
- collagenosis (connective tissue pathology);
- myelofibrosis (excessive formation of connective tissue in the bone marrow, as a result of which its hematopoietic capacity decreases);
- dysfunction of the spleen, in which blood cells are removed too quickly, and a number of other diseases affecting hematopoiesis.
Leukopenia can only be diagnosed through laboratory tests. A decrease in WBC is a sign of an emerging or existing disease.
Leukocyte formula: what is it and its norms
The leukocyte formula is the differentiation of leukocytes into 5 subclasses. Each subclass is responsible for a particular function in the body. Conducting this study is important in the differential diagnosis of inflammatory and infectious diseases, hematopathies, as well as for monitoring the treatment (chemotherapy).
Table of leukocyte formula standards for adults
| Indicators | Band neutrophils | Segmented neutrophils | Eosino-philes | Baso-phyla | Lymphocytes | Monocytes |
| Standard values | 1–6% | 47–72% | 1–5% | 0–1% | 18–37% | 3–11% |
Neutrophils (NEUT) are the most numerous class of leukocytes. It determines the body's primary defense against infections (through phagocytosis).
Leukemoid reaction in tuberculosis may cause increased neutrophil levels
Reasons for increased neutrophils:
- general leukocytosis;
- chronic myeloid leukemia;
- leukemoid reaction against the background of sepsis, tuberculosis, malignant tumors with metastasis to the bone marrow.
Conditions and/or diseases in which the neutrophil count is reduced:
- viral infection;
- cytostatic therapy;
- exposure to radiation;
- aplastic and B12-deficiency anemia;
- agranulocytosis.
The percentage of eosinophils in healthy people in the peripheral blood is insignificant. But their number increases in tissues (including blood) in allergic, parasitic and tumor diseases. The minimum level of these cells is observed in the morning. The maximum is closer to midnight. Under stress, the number of eosinophils decreases sharply.
Eosinophil levels are elevated in the following conditions:
- allergic reactions with hay fever, bronchial asthma, atopic dermatitis;
- helminthiasis;
- scarlet fever;
- Wiskott–Aldrich syndrome;
- systemic collagenoses (rheumatoid arthritis, periarteritis nodosa);
- chronic myeloid leukemia;
- lymphogranulomatosis;
- the use of sulfonamides, para-aminosalicylic acid;
- eosinophilic esophagitis, gastritis, colitis in newborns fed with cow's milk.
Basophils contain histamine granules. Their main function is to participate in immediate hypersensitivity reactions.
Basophil levels higher than normal may be due to allergies
An increase in the number of basophils may be a consequence of the following conditions:
- allergy;
- megakaryoblastic leukemia in Down syndrome;
- hematoblastosis;
- systemic mastocytosis;
- basophilic leukemia;
- condition after splenectomy;
- chronic hemolytic anemia;
- hypofunction of the thyroid gland.
An increase in the level of basophils in combination with an increase in the level of eosinophils or with their normal level indicates a myeloproliferative process.
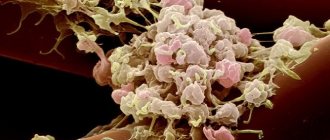
There are 3 populations of lymphocytes: T, B and NK (natural killer cells). Each population performs its own specific function.
Leukopenia is a decrease in the level of leukocytes in the blood. This condition most often indicates a weak reactivity of the immune response.
The level of lymphocytes increases in the following conditions:
- tuberculosis;
- whooping cough;
- chronic lymphocytic leukemia;
- chronic radiation sickness;
- thyrotoxicosis;
- bronchial asthma;
- lymphoma.
The amount of LYMP decreases in the following pathologies:
- aplastic anemia;
- some types of leukemia;
- infiltrative and miliary tuberculosis;
- glucocorticosteroid therapy;
- systemic lupus erythematosus;
- AIDS;
- sarcoidosis
Monocytes are the largest formed elements. They migrate from the blood to the tissues in response to chemotaxis. Monocytes produce biological active substances: enzymes, complement proteins, coagulation factors.
Elevated monocyte levels may occur with rubella
The level of monocytes increases in the following diseases:
- tuberculosis;
- syphilis;
- brucellosis;
- rubella;
- scarlet fever;
- infectious mumps;
- mononucleosis;
- lymphogranulomatosis;
- infective endocarditis.
With mononucleosis, atypical mononuclear cells are present in the peripheral blood in an amount of more than 5%.
A clinical blood test is of paramount importance in the diagnosis process. The entire further diagnostic complex begins with it (biochemical research, instrumental and specific diagnostics).
Indications for WBC testing
WBC in a blood test is a value that is used to evaluate existing or potential health threats.
A blood test for leukocytes is prescribed in the following cases:
- suspected infection or inflammatory process;
- a prolonged increase in body temperature that does not subside;
- constant headaches, frequent discomfort in joints or bones;
- suspicion of impaired hematopoietic function;
- to monitor the treatment.
The appointment for the analysis is given by the attending physician. The first specialist to whom the patient turns should be a therapist. If necessary, this doctor prescribes laboratory tests or gives referrals to specialists. If the patient has a chronic disease, then you can immediately contact a specialized specialist.
How is WBC determined?
The WBC indicator is calculated by examining venous or capillary blood during a clinical analysis. The essence of the study is to count white blood cells in a certain volume of biological fluid, taking into account their types. The ratio of all types of leukocytes, expressed as a percentage, is called the leukocyte formula.
In modern conditions, blood samples are most often processed using automatic equipment (hematology analyzers), but it is possible to carry out this study using a microscope. Automation is able to test samples simultaneously according to several parameters (from 5 to 24), and build histograms (graphical presentation of information) for red blood cells, platelets, and leukocytes.
General information
A clinical, or general, blood test (CBC) is a type of study that involves studying a sample of biological material in order to identify abnormalities. Most often, a specialist determines the indicator of hemoglobin (hgb), red blood cells (rbc) and leukocytes (wbs or wbc).
It is the latter indicator that is considered the most important in diagnosing many pathological conditions.
There are several types of leukocytes in the human body, each of which plays an important role in the body.
In addition, it is necessary to determine the erythrocyte sedimentation rate (ESR) .
The indicator plays an important role in confirming the presence of diseases of inflammatory etiology.
In addition to indicating the total number of leukocytes in the analysis, it is necessary to write down the leukocyte formula, that is, the number of subtypes of white blood cells.
Experts usually distinguish 5 varieties that are studied during diagnosis:
- Neutrophils are responsible for identifying foreign cells in the body and quickly destroying them. After this, they die, new ones are formed and the cycle repeats. Only mature neutrophils are capable of coping with the pathogen, so the discovery of a large number of immature cells indicates a recent struggle.
- Basophils play an important role because they are a kind of indicators that react to allergens. They transmit a signal to other cells, which leads to the development of a reaction.
- Eosinophils become active only when a parasitic infection enters the body.
- Monocytes are immature cells that quickly respond to the appearance of pathogens and destroy them.
- Lymphocytes are responsible for human immunity, since they have the ability to “remember” many pathogens and prevent their re-development.
When studying the leukocyte formula, it is possible to identify the presumptive cause of a particular deviation. The total number of leukocytes is also important, but a detailed analysis is required to clarify the diagnosis.
Preparing and conducting WBC analysis
The number of leukocytes is not a constant value; it depends on age, nutrition, time of day and state of health. To obtain the most accurate data, it is necessary to exclude the influence of food and drink, stress and medications on the blood composition. And even in this case, a blood test for WBC does not always provide enough information; this may require additional checks.
On the eve of blood sampling, it is necessary to refrain from fluoroscopy and physiological procedures. High mental load can also affect the result. If the patient is already receiving drug treatment, it is necessary to discuss with the doctor the temporary withdrawal of drugs or injections. When this is not possible, you should warn about the medications you are taking.
Rules for preparing for blood collection:
- limiting any load on the day before taking the test;
- sufficient night rest;
- refusal of alcohol both the day before and on the day of collection;
- stopping smoking before coming to the medical facility (it is advisable not to smoke from the very moment you wake up);
- fasting for 10-12 hours before taking the test;
- postpone breakfast or a morning cup of coffee until after donating blood, you can drink weak tea without sugar;
- Before entering the office, take a short rest (10 minutes) in order to calm down and even out your breathing.
If a repeat analysis is required, blood sampling should be carried out in the most similar conditions: in the same laboratory, at the same time, and even the route to the medical facility should preferably be done under the same conditions (on foot or by transport).
Blood for general analysis is taken from a vein or from a finger, usually the ring finger. A blood test from a vein is considered the “gold standard”, but capillary blood (from a finger) is often used. There is a scatter in the research results, but it is quite small and has almost no effect on the accuracy of the assessment. However, a specialist must decide on the type of blood for research (venous or capillary).
Laboratory microscopy
Calculation of the hematocrit number is included in the general clinical blood test. A separate study of this indicator may be prescribed in case of unsatisfactory results of OKA: anemia (anemia) and high concentration of red blood cells, as well as in case of bleeding of various etiologies (origins), in case of dehydration (dehydration) of the body. HCT is an important indicator of chronic hematological diseases.
To obtain objective final data, on the eve of the study, the patient is recommended to eliminate heavy foods (fatty and fried foods) from the diet, eliminate alcohol-containing drinks, and limit sports and other physical activities. The blood sampling procedure is carried out in laboratory conditions, in the morning.
Before the analysis, it is advisable to give up breakfast and smoking. The hematocrit value is determined using a laboratory device into which a glass graduated tube containing the blood sample being tested is placed. An anti-clotting agent is first added to the biofluid.
Under the influence of centrifugal forces (centrifugation), the blood is stratified. Red blood cells precipitate, clearly demonstrating their volume, and the plasma rises to the top. The remaining formed elements (leukocytes and platelets) are concentrated between them.
Brief scheme for hematocrit allocation
In modern laboratories, the process of measuring red blood cell volume is fully automated. The measurement value of hematocrit in clinical microscopy is taken as percentages or units (% multiplied by a factor of 0.01).
Decoding the results of the analysis of the WBC indicator
Independent interpretation of research results by a non-specialist can only give a superficial idea of the state of health. This is enough for preliminary conclusions, but choosing medications and treatment regimens on your own is dangerous. The result of incorrectly deciphering the WBC indicator is the risk of erroneous self-medication, which can lead to very disastrous consequences.
When processing WBC values, the patient’s gender, age, as well as previous or existing diseases and medications taken should be taken into account. Understanding the overall picture of a person’s health can only be achieved with appropriate knowledge and experience. And even under such conditions, doctors often prescribe additional tests to clarify or clarify certain aspects of the patient’s condition.
At what WBC indicator should you consult a doctor?
The number of leukocytes under normal conditions fluctuates over a fairly wide range. It can increase during the day, after eating, with overheating or hypothermia, or physical activity. This is the so-called physiological leukocytosis, this condition does not require seeing a doctor.
In women, the normal limits are slightly expanded, since the WBC value is also influenced by hormonal levels.
However, if the indicator is above or below the limit established for the patient’s gender and age, then contacting a specialist is necessary. The first thing you should do is visit a therapist.
An increase in WBC is not a disease in the literal sense of the word, but only a signal of problems that have arisen. More information will be needed to make an accurate diagnosis. A careful survey and examination of the patient is necessary; additional studies are not excluded.
How to get your WBC back to normal
You can reduce the WBC level, if its increase is caused by an illness, with the help of medications. If the increase in the indicator is caused by physiological reasons, then over time the value will return to normal. The increase in the number of leukocytes occurs mainly due to diet. In this case, medications act only as an auxiliary tool.
It is impossible to raise the WBC value with medications alone. The diet should be prescribed and monitored by the attending physician. In general, it is recommended to increase the proportion of protein foods and foods rich in vitamins, especially ascorbic and folic acid. Meals with a high content of lysine and choline are also needed.
Medications
Medicines to reduce WBC are prescribed depending on the disease that caused leukocytosis:
- for inflammation, anti-inflammatory drugs;
- bacterial infections are treated with antibiotics;
- viruses respond to antiviral drugs;
- helminthiasis is treated with antiparasitic drugs;
- allergic reactions are stopped with antihistamines.
All medications have their contraindications and side effects, so only a doctor has the right to select medications and calculate a treatment regimen, based on the patient’s medical history.
Traditional methods
To increase the WBC level, the following compounds are used:
- Pollen. Mix two parts pollen with one part honey and leave for three days. Take a teaspoon with milk.
- Sweet clover infusion (cold). Add cold boiled water (2 cups) to two teaspoons of dried crushed herb, leave for four hours, strain. Drink a third of a glass 20-40 minutes before meals three times a day.
- Oat decoction. Pour unpeeled oats (2 tablespoons) with hot water (400 ml), boil for 15 minutes, strain. Drink half a glass three times a day for a month.
You can reduce your WBC using the following means:
- Infusion of linden inflorescences. Pour a tablespoon of flowers with hot water (200 ml), boil for five minutes over low heat. The daily dose is two to three glasses.
- Blackthorn berries. Pour a kilogram of berries with water (400 ml), mash. Leave for a day, sweeten to taste, and boil over low heat. Wait until the infusion cools, then strain. Take 50 g. before meals three times a day.
Other methods
The following will help you increase your WBC:
- fresh vegetables and berries, fruits, buckwheat, herbs, oats;
- seafood, red caviar, chicken eggs, nuts, dry red wine in small doses;
- increasing the proportion of fruits and vegetables that are red in color, pomegranate is especially recommended;
- Beetroot juice increases the level of leukocytes, perfect for the prevention of malignant tumors;
- the proportion of meat, liver and animal fats should be reduced.
Elevated WBC levels associated with obesity are corrected with a competent diet developed by specialists. Regular fasting is not considered a diet. Uncontrolled refusal of food can cause great harm to health.
Decoding
Now let's go through each of these indicators and figure out what they mean.
HGB - hemoglobin - Hemoglobin
Hemoglobin is a protein that carries oxygen throughout the body and delivers it to the necessary tissues. If there is not enough of it, the cells begin to starve and a whole chain of symptoms develops: weakness, fatigue, dizziness, hair loss and brittle nails, snags in the corners of the lips and others. These are symptoms of anemia.
The hemoglobin molecule contains iron, and vitamin B12 and folic acid also play an important role in its formation. If there are not enough of them, hemoglobin synthesis is disrupted in the body and anemia develops.
There are also hereditary forms of anemia, but they occur much less frequently and deserve separate analysis.
Normal hemoglobin is 120-160 g/l for women and 130-170 g/l for men. You need to understand that in each specific case the standards depend on the laboratory. Therefore, you need to look at the reference values of the laboratory in which you took the test.
Elevated hemoglobin numbers most often occur due to blood thickening, if a person sweats excessively during the heat, or takes diuretics. Climbers and people who often go to the mountains may have even higher hemoglobin - this is a compensatory reaction to a lack of oxygen. Hemoglobin can also increase due to diseases of the respiratory system - when the lungs work poorly and the body constantly lacks oxygen. Each specific case needs to be examined separately.
A decrease in hemoglobin is a sign of anemia. The next step is to figure out which one.
RBC - red blood cells - Erythrocytes
Erythrocytes are red blood cells that transport hemoglobin and are responsible for the metabolic processes of tissues and organs. It is hemoglobin, or rather its iron, that colors these cells red.
Standards for men are 4.2-5.6*10*9/liter. For women - 4-5*10*9/liter. Which again depends on the laboratory.
Red blood cells can increase due to fluid loss through sweat, vomiting, and diarrhea when the blood thickens. There is also a condition called erythremia, a rare bone marrow disorder where too many red blood cells are produced.
A decrease in levels is usually a sign of anemia, more often iron deficiency, less often another.
MCV - mean corpuscular volume - Average volume of red blood cells
The norm is 80-95 for men and 80-100 for women.
The volume of red blood cells decreases in iron deficiency anemia. And it increases with B12 deficiency, with hepatitis, and decreased thyroid function.
HTC - hematocrit - Hematocrit
This is the percentage of formed elements of blood to its total volume. The indicator helps the doctor differentiate what is causing anemia: loss of red blood cells, which indicates a disease, or excessive blood thinning.
PLT – platelets – platelets
These are blood elements responsible for the formation of a thrombotic clot during bleeding. Exceeding normal values may indicate physical stress, anemia, inflammatory processes, or may indicate more serious problems in the body, including cancer and blood diseases.
A decrease in platelet levels in recent years often indicates constant use of antiplatelet agents (for example, acetylsalicylic acid) to prevent myocardial infarction and ischemic cerebral stroke.
And a significant decrease in them can be a sign of hematological blood diseases, including leukemia. In young people - signs of thrombocytopenic purpura and other blood diseases. It can also appear due to the use of antitumor and cytostatic drugs, hypothyroidism.
WBC - white blood cells - leukocytes
These are the main defenders of our body, representatives of the cellular immunity. An increase in the total number of leukocytes most often indicates the presence of an inflammatory process, predominantly of a bacterial nature. It may also be a sign of so-called physiological leukocytosis (under the influence of pain, cold, physical activity, stress, during menstruation, sunburn).
Norms for men and women usually range from 4.5 to 11.0*10*9/liter.
A decrease in white blood cells is a sign of immune suppression. The most common causes are viral infections, taking certain medications (including non-steroidal anti-inflammatory drugs and sulfonamides), and weight loss. Much less common are immunodeficiencies and leukemia.
Possible complications
Leukocytosis is not dangerous in itself, it is a kind of emergency signal from the body. However, an increase in leukocytes that is not associated with physiological reasons cannot be ignored, since the time to start treatment will be missed. This will significantly increase the risk of complications from the underlying disease.
A decrease in WBC level means a weakened immune system. The body becomes defenseless against any infections. And the lower the value, the more dangerous the disease becomes. Even ordinary hypothermia can give rise to a serious illness, provoke serious complications, and in critical conditions, death is not excluded.
Elevated or decreased WBC levels are not a disease. This is a signal indicating that a person has health problems. The WBC indicator in a blood test provides information about the state of immunity, the presence of inflammation or other diseases. To bring the blood composition back to normal, it is necessary to identify and treat the underlying disease.
Leukocyturia – leukocytes in the urine
The presence of leukocytes in urine is a physiological phenomenon, and their number should not exceed 5 cells in the field of view of the microscope. An amount higher than normal is called leukocyturia. In this condition, the urine has a cloudy color and an unpleasant odor, and traces of blood may appear. A common symptom of leukocyturia is pain in the lower abdomen.
The most common cause of leukocyturia is acute or chronic urinary tract infection. However, elevated white blood cell levels may indicate more serious conditions, such as:
- stones in the kidneys;
- adnexitis;
- glomerular, interstitial pyelonephritis;
- bladder cancer;
- prostate inflammation or cancer.
However, don't panic because elevated levels of white blood cells in the urine, as well as in the blood, can be associated with intense sports, fever, dehydration, or the use of certain medications (anti-tuberculosis, anti-cancer, blood pressure-lowering medications).