Insulin is a protein hormone produced by the pancreas. It has a great influence on metabolic processes in almost all tissues of the body. One of its main tasks is to control blood glucose levels.
Thanks to insulin, the process of glucose absorption by fat and muscle cells is accelerated, and the formation of new glucose cells in the liver is inhibited. Creates a supply of glycogen - a form of glucose - in cells, promotes the preservation and accumulation of other energy sources, such as fats and proteins. Thanks to insulin, their breakdown and utilization are inhibited.
If the pancreatic function is not impaired and the gland is in order, it constantly produces the amount of insulin necessary for the normal functioning of the entire body.
After eating, the volume of insulin increases, this is necessary for the high-quality processing of incoming proteins, fats and carbohydrates. In the event that there are functional deviations in the activity of the pancreas, a malfunction occurs in the functioning of the whole organism.
This disease is called diabetes mellitus. When insulin production is insufficient, type 1 diabetes mellitus occurs. In this disease, the beta cells of the pancreas, which produce insulin, are destroyed. The body is not able to properly assimilate incoming food.
To maintain the functioning of the body in a normal state, such a patient is given insulin “for food” before meals. The volume that should cope with the high-quality processing of incoming food. Insulin is also administered between meals. The purpose of these injections is to ensure normal functioning of the body in between meals.
When insulin is produced in the body in the required volume, but its quality is impaired, type 2 diabetes mellitus occurs. With this type of disease, the quality of insulin is reduced and it cannot have the desired effect on the body's cells. In fact, such insulin is of no use. It is unable to process glucose in the blood. With this type, drugs are used to stimulate insulin to act.
Why does a person need insulin?
Insulin is directly involved in metabolic processes occurring in the human body:
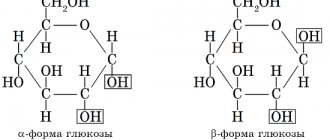
- Sugar, which a person receives from food, thanks to insulin, can penetrate the cells of the body's tissues. It is insulin that makes their membranes more permeable.
- Insulin stimulates the production of glycogen from glucose, which occurs in muscle cells and liver cells.
- Proteins are able to accumulate, synthesize and not disintegrate in the body also thanks to insulin. The hormone helps fat cells take up glucose and transform it into fat tissue. It is for this reason that excessive consumption of carbohydrate foods leads to fat deposits.
- Insulin has an anabolic effect (increases the activity of enzymes that promote the breakdown of glucose), as well as an anti-catabolic effect (prevents other enzymes from dissolving glycogen and fats).
The body needs insulin; it is involved in all processes that occur in it. However, the basic task of this hormone is to ensure normal carbohydrate metabolism. Insulin is the only hormone that can lower blood sugar levels. All other hormones help increase blood glucose levels. We are talking about adrenaline, glucagon, growth hormone.
Insulin begins to be produced by the pancreas after the level of carbohydrates in the blood rises. This happens when the food a person has eaten enters the stomach. Moreover, the food product may contain carbohydrates in a minimal amount. Thus, any food that enters the stomach causes the level of insulin in the blood to begin to rise. If a person is fasting, the level of this hormone begins to fall.
The process of insulin production is also influenced by other hormones, as well as calcium and potassium (if their values increase), fatty acids (if they are present in large quantities in the blood). Somatotropin (growth hormone), on the contrary, helps reduce insulin levels in the blood. Somatostatin has a similar effect, but to a lesser extent.
Insulin levels directly depend on blood glucose levels, so studies aimed at determining them are almost always carried out in parallel. To implement them, you need to donate blood to the laboratory.
Video: Insulin: why is it needed and how does it work?
Symptoms of deviation from the norm
Unstable insulin levels can be indicated by a variety of symptoms, with both high and low levels showing the same symptoms.
Symptoms of insulin instability:
- constant desire to drink water;
- you want to empty your bladder unusually often (pollakiuria);
- the skin becomes dry and tight, a rash appears on it;
- increased appetite (polyphagia);
- problems of a vegetative-vascular nature.
In women, unstable insulin leads to increased sweating (hyperhidrosis), facial pigmentation, and infertility.
Diabetes mellitus type 1 and 2: relationship with insulin
In type 2 diabetes, there is a change in the normal production and functionality of insulin. Most often, the disease manifests itself in elderly people who suffer from obesity. With excess accumulation of fat in the body, the number of lipoproteins in the blood increases. This helps reduce cell sensitivity to insulin. As a result, the body begins to produce it in smaller quantities. The level of insulin in the blood drops, and the level of glucose begins to rise, because there are not enough hormones to utilize it.
If your blood glucose level is elevated, then you need to start following a diet and get rid of fat deposits. In this case, the risk of developing diabetes mellitus is reduced, which means a person can avoid serious health problems.
Type 1 diabetes develops differently. With this type of disease, there is a lot of glucose around the cells, but they cannot absorb it, since there is not enough insulin in the blood for these purposes.
As a result of such disorders, the following pathological changes begin to occur in the body:
- Fat reserves from the reserve are not utilized in the Krebs cycle, after which they are sent to the liver. There, fat takes part in the formation of ketone bodies.
- The higher the blood glucose level, the more thirsty a person is. At the same time, sugar begins to be excreted in the urine.
- Carbohydrate metabolism begins to occur along the sorbitol pathway, which is an alternative pathway. This entails negative consequences, since excess sorbitol begins to accumulate in the tissues. When it accumulates in the eye lens, a person develops cataracts, when it accumulates in nerve fibers - polyneuritis, and when it accumulates on the walls of blood vessels - atherosclerotic plaques.
The body tries to prevent these disorders and begins to break down fats. This entails an increase in triglycerides in the blood and a drop in good cholesterol. Hyperlipidemia contributes to a decrease in immunity, an increase in fructosamine and glycosylated hemoglobin in the blood, and a change in its electrolyte balance. The person begins to feel worse and worse, while he is constantly tormented by thirst and urinates frequently.
Diabetes mellitus affects the functioning and condition of all internal organs, which explains the variety of clinical manifestations of the disease.
Causes of increased and decreased insulin in the blood
The following pathologies can lead to increased insulin levels in the blood:
- Insulinomas are tumor formations of the islets of Langerhans. They produce insulin in large quantities. At the same time, on an empty stomach the level of glucose in the blood will be reduced. To detect a tumor, doctors use a formula to calculate the ratio of insulin to glucose. In this case, the level of insulin in the blood is divided by the level of glucose in blood taken on an empty stomach.
- Early stage of type 2 diabetes mellitus. As the disease progresses, insulin levels will decrease and glucose levels will increase.
- Excess body weight. Sometimes it is the increased level of insulin in the blood that provokes the development of obesity, as a person’s appetite grows, he overeats and accumulates fat. Although it is not always possible to track the cause of obesity.
- Tumor lesion of the pituitary gland (acromegaly). If a person is healthy, insulin helps lower glucose levels. This, in turn, promotes the production of somatotropin. When acromegaly develops, such production does not occur. This feature is used when conducting stimulation tests aimed at determining hormonal balance. When insulin is administered in the form of intramuscular injections, the level of somatotropin does not increase either one or two hours after the injection.
- Hypercorticism. With this disease, there is an increased production of glucocorticoids in the body, which suppress the processes of glucose utilization. As a result, its values remain elevated despite high levels of insulin in the blood.
- Muscular dystrophy. It develops against the background of metabolic disorders, and the insulin level will be increased.
- The period of pregnancy can lead to an increase in insulin levels if a woman overeats.
- Hereditary diseases associated with fructose and galactose intolerance.
If a patient in a hyperglycemic coma is given an injection of fast-acting insulin, this will bring him out of this state. Insulin injections are also used to treat patients with diabetes, since its administration helps reduce blood glucose levels. In this case, the level of insulin itself will be increased in a person.
You can reduce insulin levels if you focus your efforts on treating the underlying disease that leads to disturbances in metabolic processes.
Low insulin levels are observed in type 1 and type 2 diabetes mellitus. In this case, non-insulin-dependent diabetes causes a relative decrease in insulin in the blood, and insulin-dependent diabetes causes an absolute drop in the hormone in the blood. Serious stress, physical activity and other factors that have an adverse effect on the body can also lead to its decrease.
Interpretation of analysis results. C-peptide rate (ng/ml)
The acceptable range is from 0.78 to 1.89. Concentrations below normal are observed when:
- type 1 diabetes;
- alcoholic hypoglycemia;
- stressful situation;
- removal of part of the pancreas.
C-peptide levels above standard values are typical for the following conditions:
- insulinoma;
- renal failure in the chronic stage;
- taking certain hormonal medications;
- hypoglycemia while taking tablet drugs from the group of sulfonylurea derivatives.
Determining the level of insulin in the blood - why is it necessary?
Insulin level, as an independent blood indicator in absolute value, has a low diagnostic value. To make a conclusion about a particular disorder in the body, it is necessary to determine the level of glucose in the blood and correlate these two indicators.
The most informative test is the stimulation of insulin production with glucose, or, as it is also called, a stress test. It allows you to diagnose diabetes that has a latent course. In this case, the body’s response to produce insulin will be delayed, its concentration increases slowly, but in the future the level of the hormone will increase significantly. If a person is healthy, then insulin in the blood will increase smoothly.
There is another study that has diagnostic value in terms of determining disorders in the production of insulin in the body. This is a glucose loading test (fasting test). First, blood is taken from the patient on an empty stomach, which is examined for the level of glucose, insulin and the protein part that is part of the proinsulin molecule. Then the person must fast for 24 hours and drink limited water. Every 6 hours, his blood is taken to determine the indicator that raises doubts among doctors, that is, C-peptide, glucose or insulin, or all three substances at once.
In general, insulin levels in the blood do not increase in a healthy person. The exception is pregnant women, which is a normal physiological phenomenon for this condition. In all other cases, insulin levels should remain within normal limits.
If it increases, then this is a reason to suspect the following pathologies:
- A tumor of the pancreas, which is located in the tissues of the islets of Langerhans.
- Hyperplasia of tissues of the islets of Langerhans.
- Disturbances in the production of glucocorticoids in the body.
- Severe disturbances in liver function.
- Early stage of diabetes mellitus.
In some diseases, for example, hypercortisolism, acromegaly, muscular dystrophy, insulin levels are monitored in order to monitor the functioning of the body's internal systems.
Principles of correction
You can reduce high levels of the hormone by limiting the number of meals. Once a week you should have a fasting day. The level of hormonally active substances during this period returns to acceptable limits.
There is a so-called insulin index of products, which must be taken into account when drawing up a personal menu. This indicator specifies how much of the hormone the body will need to return sugar to normal after consuming a particular product.
It is important to normalize physical activity. Adequate exercise can lower insulin levels, restoring the sensitivity of cells and tissues to its action.
In addition, you need to adjust your diet: limit carbohydrates and increase the intake of foods containing fiber.
Donating blood for insulin
To calculate the level of insulin in the blood, you will need to take it from a vein. If insulin is determined in plasma, then the blood is drawn into a tube containing heparin. If insulin is determined in blood serum, then an anticoagulant is not required. The study must be carried out no later than 15 minutes after taking blood for analysis.
For the results to be reliable, a person must fast for 12 hours, cannot take any medications, and should also refrain from physical activity. Provided that it is not possible to refuse to take medications, this must be reflected in the analysis form.
30 minutes before taking blood from a vein, a person should go to the doctor’s office and lie down. He needs to spend this time in a calm and relaxed state. Otherwise, it will not be possible to obtain reliable data.
Insulin injections
Insulin is prescribed to people as a medicine for various diseases, the main one being diabetes mellitus.
Many people need insulin. Patients cope with its administration on their own. However, they first receive medical advice. It concerns the correct use of the device, the rules of antiseptics, and the dosage of the drug. All patients suffering from type 1 diabetes are forced to inject themselves with insulin in order to continue living normally. Sometimes the hormone is administered on an emergency basis; this is required when complications of the disease develop and in some other serious conditions. For type 2 diabetes mellitus, it is possible to replace injections with oral medications. The fact is that this type of disease requires the administration of insulin only when it is severe. Therefore, if complications develop, a person simply does not have the skills to administer insulin intramuscularly. It's easier for him to take a pill.
Insulin solution, which is based on human insulin substance, is a safe and effective remedy that produces a small number of side effects. The hypoglycemic hormone produced by the pig pancreas has the greatest similarity to human insulin. This is what has been used for many years to treat people. Modern medicine offers people insulin, which was obtained through genetic engineering. If a child needs therapy, he will receive exclusively human insulin, not animal insulin.
The introduction of the hormone allows you to maintain a normal level of glucose in the blood, preventing it from rising and falling to critical levels.
Depending on the person’s disease, his age and the presence of concomitant pathologies, the doctor selects the dose for him individually. The patient must be given full instructions on how and at what time he needs insulin injections. In addition, a person must adhere to a special diet, which is also agreed upon with the doctor. The daily routine, nature and intensity of physical activity should be changed. Only if all these conditions are met can therapy be made effective, which will help improve the quality of life.
Are there insulin analogues? Previously, in Russian clinical practice, only original analogues of foreign-made insulin were used, such as, for example, Humalog (Eli Lilly, insulin lispro), Lantus (Sanofi, insulin glargine), Novorapid (Novo Nordisk, insulin aspart) and others, but now analogues have appeared Russian production. So, for example, the following drugs were registered: RinLiz (replaces Humalog), RinLiz Mix 25 (replaces Humalog Mix 25), RinGlar (replaces Lantus).
These drugs are convenient for the patient to use because they provide a stable effect and the required duration of action and have fewer side effects.
Indications for use
The main area of application of insulin is endocrinology. The hormonal drug is prescribed for therapeutic purposes to patients with established type I diabetes mellitus (insulin-dependent). Insulin can also be prescribed in case of autoimmune attacks on the body in type II diabetes mellitus.
Short-acting insulin, which remains active for 6 hours, is prescribed as part of complex therapy to lower blood sugar in certain diseases:
- Schizophrenia.
- Thyrotoxicosis.
- Chronic hepatitis.
- Stages 1-2 of liver cirrhosis.
- Stomach diseases.
- Furunculosis.
A special place is given to the drug in the treatment of general exhaustion, if it is necessary to restore the patient’s normal nutrition. In these cases, the anabolic effect of insulin is important, which helps to gain body weight.
In cardiological practice, insulin is used as part of polarizing mixtures. The solution is administered intravenously for spasm of the coronary vessels, leading to coronary insufficiency.
Insulin in bodybuilding
What happens to a healthy person after an insulin injection? This question can be answered by considering the practice of using hormonal drugs in a sports environment. Athletes use short-acting insulin in combination with anabolic and androgenic agents. The pancreatic hormone helps increase the permeability of cell membranes of muscle tissue. This facilitates easier and faster penetration of anabolic steroids into the muscles. In combination with insulin, lower dosages of steroids are required to achieve a pronounced effect than with solo courses.
To safely use insulin in bodybuilding, it is important to follow certain rules:
- Don't overeat. In the body, excess nutrients are transformed into fat deposits.
- Reduce the content of simple carbohydrates in your daily diet.
- Assess muscle growth using a measuring tape and a mirror, rather than by weighing yourself. Measurements of the volume of the biceps, thighs, and lower legs will indicate the effectiveness of insulin injections. An incorrectly calculated dose of the drug will lead to the formation of fat folds, for example, in the abdominal area.
Contraindications
The use of insulin is prohibited for diseases that are accompanied by hypoglycemia:
- Acute form of hepatitis.
- Cirrhosis of the liver.
- Hemolytic jaundice.
- Pancreatitis.
- Nephritis.
- Amyloidosis.
- Decompensated forms of heart defects.
- Peptic ulcer of the stomach and duodenum.
For some diseases, the prescription of insulin requires additional research in order to minimize possible negative consequences. Certain control and caution must be observed when prescribing the drug to patients with the following pathologies:
- Forms of diabetes mellitus, accompanied by signs of coronary insufficiency and cerebrovascular accident.
- Thyroid diseases.
- Kidney failure.
- Addison's disease, which affects the adrenal glands, develops adrenocortical insufficiency.
Side effects
Insulin is administered subcutaneously, and therefore the most common negative symptom is lipodystrophy, a pathological condition characterized by atrophy or excessive growth of adipose tissue in the injection area.
The insulin preparations that are currently available go through several levels of purification. These measures significantly reduce the risk of allergy symptoms. If allergic reactions develop, the drug used is discontinued, emergency hyposensitizing therapy is carried out and another type of insulin is selected.
Overdose
Failure to comply with doctor's instructions or exceeding the therapeutic dose always causes the development of hypoglycemia. In this condition, blood sugar levels decrease rapidly, which can lead to the death of the patient. An excessively high dose of insulin requires prompt medical intervention.
Clinical signs of hyperglycemia:
- Thirst.
- Frequent urination.
- Fatigue.
- Dryness of the oral mucosa and skin.
- Itching.
- Visual impairment, feeling of a veil before the eyes.
- Disorder of consciousness.
- Heart rhythm disturbance.
- Prekoma.
- Coma.
An overdose of insulin poses a danger to a person’s brain activity, and this is especially dangerous for older patients. The development of paralysis and paresis is possible. High doses of insulin affect the elasticity of vascular walls, which affects proper cerebral circulation.
At the first signs of a drop in sugar, the patient is offered sweet tea, fruit juice or honey.
For coma, intensive therapy consists of intravenous administration of 10-20 ml of 20% or 40% glucose solution.
Another treatment regimen is allowed:
- 1-2 mg of glucagon (insulin antagonist) - intramuscularly.
- 0.5 ml of 0.1% solution of adrenaline hydrochloride - subcutaneously.
- 150 ml of 10% glucose as an enema.
Interaction with other drugs
The effectiveness of insulin increases with simultaneous treatment with certain medications:
- alpha-blockers.
- Acetylsalicylic acid.
- Clofibrate.
- Fluoxetine.
- MAO inhibitors.
- Cyclophosphamide.
- Tetracycline.
- Ifosfamide.
The ability of insulin to lower blood sugar is observed when it is combined with certain drugs:
- Oral contraceptives.
- Chlorprothixene.
- Glucocorticosteroids.
- Diazoxide.
- Heparin.
- Lithium carbonate.
- Saluretics.
- Nicotinic acid.
- Thyroid hormones.
- Diphenin.
- Symptomimetic agents.
- Tricyclic antidepressants.
Terms of sale
Insulin drugs are available by prescription. The endocrinologist must write a prescription in Latin.
How to store insulin?
The best place to store insulin is in the refrigerator door. Optimal conditions are observed here - darkening, temperature from +2 to +8°C. Insulins of any type must not be frozen or heated. At temperatures above +35°C, the drug loses all medicinal properties. Patients who maintain an active, sporty lifestyle often use a thermal bag to store insulin.
Best before date
The expiration date on the packaging and bottle must match. It is 2 years from the date of release of the drug. If an opened bottle of insulin is stored under all conditions, it can be used for a month.
How can you tell if your insulin is bad?
If storage rules are not followed, the drug cannot be used. It is forbidden to inject an insulin solution that has changed color or in which any suspensions, fibers, or lumps have formed. If, when shaking the bottle with the suspension, no whitish suspension is observed, then the drug should be considered spoiled. Transparency is a sign of quality for ultra-short, short-acting and rapid-acting insulins. Extended-release insulin glargine should remain clear.
What types of insulin are there?
There are several types of insulin. It will need to be administered at different times of the day.
- Humalog and Novorapid are ultra-short-acting insulin preparations. Insulin of this type begins to act after 15 minutes, the maximum effect of hormones can be expected after 1-1.5 hours, and 4 hours after its administration there will be no insulin in the blood.
- Insuman Rapid, Actrapid NM, Humulin Regulator are short-acting insulins. The effect of the drug administration occurs within 30-45 minutes. Its effect can last up to 8 hours. The maximum effect should be expected after 2-4 hours.
- Humulin NPH, Insuman Bazal, Protafan NM are medium-duration insulins. The effect of their administration will occur in 1-3 hours, and they will act from 10 to 20 hours. Peak values of the hormone in the blood are reached 6-8 hours after administration.
- Insulin Glargine (Lantus) is a long-acting drug, the effect of which lasts for 20-30 hours. This hormone does not reach peak values, being distributed evenly throughout the entire duration of its action.
- Insulin Degludec is an ultra-long-acting drug whose effect can last for 42 hours. This drug is produced in Denmark.
The last two types of insulin are sufficient to be administered once a day. In emergency cases, they are not used, since their effect does not occur immediately, but after several hours. Therefore, when a coma develops, a person is given ultra-short-acting insulin.
Video: types of insulin used to treat diabetes:
Injections must be administered either under the skin or into the muscle. Information on this matter should be obtained from a doctor. The doctor gives instructions regarding the rules for mixing drugs, as well as the time of their administration, depending on meals. The diet for diabetes mellitus must be strictly followed, since the timing of injections and their dosage directly depends on this.
A little history
The hormone insulin, isolated from the pancreas, was first successfully used for medicinal purposes by the Canadian physician, physiologist, F.G. Bunting. For this, in 1923, at the age of 32, he was awarded the Nobel Prize in Physiology or Medicine along with his Scottish colleague, Professor MacLeod, in whose laboratory the young scientist conducted experiments on dogs. The discovery of insulin therapy completely revolutionized approaches to the treatment of diabetes. In recognition of the services of Banting, who tragically died in a plane crash during the Second World War, World Diabetes Day is celebrated on his birthday, November 14th.
Frederick Grant Banting was the scientist who first obtained insulin extract and successfully used it in the treatment of diabetes. One of the youngest Nobel Prize laureates ever since it was awarded.
Instructions for using insulin
Specifics of insulin administration
Insulin is administered by subcutaneous, intramuscular or intravenous injection. Only short-acting drugs can be injected into a vein for certain medical indications - hyperglycemic coma or pre-comatose state.
Insulin in suspension form is used exclusively intramuscularly. Injecting the drug into a vein is prohibited! Before administration, the insulin ampoule is warmed to room temperature for faster absorption. For insulin injections, a plastic syringe is used, which has virtually no “dead space”, unlike glass instruments. A set of the drug in a plastic syringe ensures that the exact dosage is maintained.
Experienced diabetics prefer syringe pens into which cartridges with insulin solution are installed. The main advantage of these syringes is that the solution does not need to be drawn up before each injection. They can be used for injections of short-, medium- and combined-acting drugs. The needles of insulin syringes are small in size - length 8 -12 mm, thickness 0.3 - 0.4 mm. These features help minimize pain during injections.
Insulin injection areas
With the question: “Where should I inject insulin?” Patients with a newly diagnosed diagnosis and relatives of patients turn to an endocrinologist. The fastest way for the hormonal drug to enter the bloodstream is when administered subcutaneously in the area of the anterior abdomen. The outer upper arm and anterior thigh area are suitable for subcutaneous injections, but absorption is slower here. The slowest absorption occurs when insulin is injected into the subscapular region or into the subcutaneous fat of the buttocks.
The preferred area for subcutaneous insulin injection depends on the type of drug. Short-acting solutions are transparent. They must penetrate the blood quickly, so the front surface of the abdomen is suitable for injections, except for the area around the navel. Long-acting insulin is produced as a cloudy solution. Its slow absorption allows for administration into the surface of the thigh and buttocks.
The patient must follow a strict sequence of changing injection sites. A specific area must correspond to a specific time of day. A morning injection of short-acting insulin can be performed in the abdomen, an afternoon injection in the thigh, and an evening injection subcutaneously in the buttock area. This rule is due to the need to calculate XE (bread units) for different times of the day.
Rules for subcutaneous insulin administration
- Check the validity period of the drug, type, dosage on the bottle.
- Wash your hands with soap and treat the injection site with an antiseptic solution.
- Heat the bottle with the solution in your hands to the optimal temperature. Do not shake the preparation under any circumstances to prevent the formation of air bubbles.
- Treat the bottle cap with an alcohol solution.
- Air is drawn into the syringe as much as the required units of the drug. Release it into the bottle and collect the required amount of insulin (in units). Considering the features of the syringe, you can draw a little more solution, about 10 units.
- Adjust the dose by fixing the syringe at eye level.
- In order to remove air bubbles, lightly tap the body of the syringe.
- When injecting the drug, count to 5 or 10 and remove the needle. Massaging the injection site is strictly prohibited! Massage promotes rapid absorption, and too active absorption can cause hypoglycemia.
It is not recommended to treat the surface of the skin with an alcohol solution. Ethyl alcohol destroys insulin, which after its administration can cause lipodystrophy. Before injection, it is enough to wash and dry the corresponding area of skin with a napkin, if necessary. In certain cases, insulin is administered through clothing.
For the injection, choose a place 2.5 cm from the navel or 3 cm from the shoulder, thigh, upper gluteal region. If the injection site is the shoulder or thigh, use your thumb and index finger to form a triangle from the skin, without grasping the muscle. The needle is inserted into the base of the formed triangle with an upward cut at an angle of 45°. It is important to ensure that the needle does not enter the muscle layer, since absorption of the drug here occurs much faster than from subcutaneous fat. For an injection in the stomach or buttock, it is not necessary to form a fold. In this case, the needle is inserted at an angle of 90°
The optimal time for insulin injections is 30 minutes before meals. This is due to the fact that the drug is absorbed into the blood within an hour. The best time to eat is 15-30 minutes after the injection.
How to choose the best insulin?
It is impossible to give a general answer to this question. The selection of insulin, the selection of dosage and the method of its administration is carried out by the treating endocrinologist during the patient’s hospitalization. This takes into account the clinical symptoms of the disease, the severity of the patient’s condition, the time of appearance of signs of a decrease in glucose levels, and the duration of the glucose-lowering effect.
Rules for calculating the dose and administration of insulin
For each patient, the dose of the drug is selected individually. Short-acting insulin begins to act very quickly, but the drug effect lasts for a short time. The solution can be administered both subcutaneously and intramuscularly. In some cases, intravenous injections are indicated.
Short-acting insulin can be injected once or several times a day. The number of injections depends on the clinical picture of diabetes. The injection is given 15-20 minutes before a meal. After this time, a sugar-lowering effect begins to appear, the peak of which is recorded after 2 hours. Its duration is approximately 6 hours.
Scope of application of short-acting insulin:
- In a hospital setting.
When selecting the required therapeutic dose in case of hyperglycemic coma, precoma. The precomatose state is urgent to change the patient's insulin activity.
- In combination with a course of anabolic drugs.
The dosage in this case is 4-8 units 1-2 times a day. The amount of insulin is minimal and cannot cause any serious consequences.
Long-acting insulins are divided into several types, depending on the duration of the effect:
- Semilong.
- Long.
- Ultralong.
Injections of long-acting drugs are performed much less frequently, due to the fact that the therapeutic effect lasts from 10 to 36 hours.
The long-acting drug is available in the form of a suspension. It is injected only subcutaneously, intramuscularly. Intravenous administration of long-acting insulin is prohibited. Due to its pharmacological characteristics, this type of insulin is not used during coma or precoma.
When selecting a drug, the doctor takes into account the time of maximum glucose-lowering effect. It is at this time that you need to eat. If necessary, mixing two long-acting drugs in one syringe is allowed.
The combined administration of long-acting and short-acting insulin is necessary when the patient needs to maintain optimal sugar levels for a long time. A combination of drugs with different effects is used to quickly normalize blood glucose. Long-acting insulin is usually recommended for morning injections. The injection is given in the morning, before breakfast. In some cases, long-acting medications can be given at other times of the day.
Patients with diabetes must adhere to a special diet. This requirement is mandatory when treating with insulin. The calorie content of food depends on the patient’s weight and lifestyle. If the patient is underweight, but at the same time there is daily physical activity, at least 3000 kcal per day should be supplied to the body along with food. Excess weight and a sedentary lifestyle means consuming no more than 1700-2000 kcal.
How to draw medicine into an insulin syringe?
Correctly drawing one type of insulin into a special syringe is not particularly difficult. To do this, you need to do several sequential steps:
- Fill the syringe with air until the required number of units of the drug is marked.
- Puncture the cap of the bottle and release air from the syringe inside.
- Holding the bottle upside down at eye level, draw a little more than the required amount of the drug into the syringe.
- In order to remove the formed air bubbles, lightly tap the syringe barrel with your finger and move the piston to the desired mark.
To correctly draw insulin from the bottle, a puncture must be made in the center of the stopper, preferably with a needle from a regular syringe. All subsequent steps are performed with an insulin syringe, inserting a needle into the previously made puncture.
Insulin dose calculation
According to the rules for calculating the drug, the daily dosage should be no more than 1 unit per kilogram of the patient’s weight. The therapeutic dose depends on the type of disease and the characteristics of the clinical picture.
For type I diabetes, the following recommendations have been developed:
- 0.5 IU per 1 kg - in the case of a newly diagnosed disease;
- 0.6 units per 1 kg - with compensation within 12 months;
- 0.7 units per 1 kg - with unstable compensation;
- 0.8 units per 1 kg - for decompensation;
- 0.9 IU per 1 kg - complicated course of the disease, phenomena of ketoacidosis;
- 1.0 units per 1 kg - for women in late pregnancy.
In order not to make a mistake in dosage calculations, you can consider one of the examples. If a patient needs to be administered long-acting insulin at a dose of 0.6 units with a weight of 75 kg, then the volume will be 0.6 x 75 = 45. Half of the resulting amount is taken, rounded down, i.e. the dose is 20 units. In the morning, before breakfast, 12 units are administered, before dinner - 8 units.
Short-acting insulin with the same parameters (weight 75 kg, dose 0.6 units) is calculated according to the rule: 0.6 x 75 = 45, 45 - 20 = 25. For a morning injection, take 9-11 units, before lunch - 6- 8 units, in the evening - 4-6 units.