Bacteriophages are viruses that selectively infect bacterial cells. Their vital activity and reproduction are possible only inside bacterial cells. By multiplying inside the cell, they cause destruction and death of the bacterium itself.
Modern medicine considers them as an effective, safe and perfect remedy in the fight against dangerous, difficult-to-treat bacterial infections. But treatment with bacteriophages causes mistrust and fear in many people.
Features of the structure and parasitism of bacteriophages
Bacteriophages represent a large and diverse group of viruses. Their sizes are one hundred times smaller than the size of bacterial cells. When magnified many times, the structure of phages is striking in its diversity; some of them look like crystalline complexes, intricately twisted among themselves.
Being intracellular viral parasites, they selectively destroy certain bacterial cells. They lack a cellular structure and consist only of genetic material covered with an outer protein coat. This forces them to look for suitable cellular complexes to actively multiply within them.
Habitat of bacteriophages
Bacteriophages are present wherever bacteria live, so their habitat is diverse. This can be the human body, air and water environment, soil, food products, clothing, etc.
Mechanism of action
A bacteriophage invades a bacterial cell for only one purpose - to use its cellular structures for its own reproduction. To do this, a smart virus injects its own genetic information into the body of the bacterium. The bacterium begins, according to the program established by the phage, to synthesize particles that are uncharacteristic for it, from which new bacteriophages are subsequently assembled. From the bacterial cell, only fragments remain, through which 100-200 synthesized phages emerge, capable of further damage to neighboring bacterial cells.
In the natural environment, bacteriophages play a critical role as natural regulators of the number of pathogenic microbes.
Areas of application of bacteriophages
In addition to the medical industry, they have found their application in other important areas.
- In agriculture - they are successfully used to prevent and treat plants and animals from bacterial infections.
- In genetic engineering, these small viral structures are used to naturally exchange genes between different bacteria, allowing the original structure of bacterial DNA to be changed in the desired direction.
What are bacteriophages?
It would be more accurate to formulate the question: “WHO are bacteriophages?”, since they are living beings.
What associations do you have when you hear the word “virus”?
Probably “ARVI”, “flu”, “disease”, “cold”, “microorganism”.
In our understanding, viruses are small evil creatures that feel bad when we feel good.
They live and multiply in our body, releasing toxins and other nasty products of their vital activity, which cause the temperature to rise, appetite to disappear, weakness to appear, headaches, etc.
Our immune system deals with some viruses in a week, while with others we have to live side by side all our lives and periodically endure their antics, because... they settle in us forever, for example, the herpes simplex virus.
But not only human viruses exist in nature. There are viruses that infect plants, animals, fish, birds, even insects. In a word, every living thing on Earth has its own viruses.
Bacteria also have them to regulate their numbers on our planet. So they are called “bacteriophages”, which means “bacteria eaters”.
If bacteriophages did not exist, bacteria would have long ago covered our mother earth with a thick layer and destroyed all living things.
So, bacteriophages are tiny viruses that can live and reproduce exclusively in a bacterial cell, and only in a cell of a certain type.
A little history...
Bacteriophages were discovered 100 years ago. Scientists began to study them, and noticed that sometimes phage therapy gives excellent results, and sometimes it turns out to be ineffective. As we found out later, the first bacteriophages were made with gross violations of production and storage technology.
With the advent of antibiotics, bacteriophages faded into the background, but, nevertheless, they were also used during the Great Patriotic War to treat wounds and prevent epidemics of intestinal infections.
Frankly speaking, we were told very little about them at the institute and it was somehow unclear. During my medical practice, bacteriophages were mentioned at various conferences and seminars, if at all, then in passing. That's why we didn't appoint them.
Now interest in them has awakened. This is due to the fact that antibiotic resistance has become rampant. Even at the stage of developing the next antibiotic, resistant strains are already appearing. And it often happens that millions spent on the creation and development of a new drug are thrown away. Such products do not even enter the market.
If resistance to the first antibiotics developed over 20-30 years, now it takes 2-3 years.
With each new generation of antibiotics, the period during which microbes develop protection against it is shortened.
Phage cocktails
A new round of interest in phage therapy has occurred in recent years. The fact is that antibiotics have also not become a panacea for the treatment of bacterial infections: these days, the development of new drugs has not kept pace with the increase in the number of bacteria with acquired resistance to existing antibiotics. Already today, in hospitals in England, about 40% of staphylococcal infections are caused by such strains, and in the United States, about 90 thousand patients die annually from hospital infections caused by drug-resistant bacteria. When recalculated for the world's population, this number is 3-5 million deaths per year!
WHO warns that the world will soon enter a “post-antibiotic” era, when there will be no treatment for common bacterial infections. And against this background, phage therapy looks like a very promising direction, the development of which can lead to the creation of effective personalized methods for treating diseases. For this, there is both the necessary knowledge about phages and the mechanisms of their interaction with bacterial cells, as well as technologies for working with viral agents.
For phage therapy today, only virulent lysis phages are used, mainly “tailed” phages of the order Caudovirales, as well as filamentous phages of the families Leviviridae (with a single-stranded RNA genome) and Inoviridae (with a single-stranded circular DNA genome).
As discussed above, the activity spectra of phages are usually very narrow and limited to one or a few closely related bacterial species. On the one hand, such narrow specificity is good for therapy, since it allows you to eliminate a specific microorganism without disturbing the entire bacterial community of the human body. On the other hand, if emergency treatment is necessary (when there is no time to identify a specific bacterium causing the development of a pathogenic process in a wound or on a burned surface), it is necessary to have a drug that affects several types of bacteria, possible causative agents of infection. To solve this problem, phage cocktails are usually used - preparations containing several phages that differ in specificity.
This approach was also used by d'Herelle. D'Herelle's cocktail, which he brought from Paris back in 1930, is still one of the main phage preparations: it forms the basis of the Georgian pyophage and the Russian intestifage. In Tbilisi, based on phage cocktails, drugs were developed for the treatment of gastrointestinal diseases and purulent wounds for mass use in the event of epidemics or military operations. The results of army trials and a wide experiment on the prevention of childhood gastrointestinal disorders conducted in Tbilisi showed the good effectiveness of such drugs.
Phage cocktails are produced in a standardized manner and target bacterial communities commonly found in specific diseases. Of course, more effective cocktails are obtained when their components are matched to the bacterial community of a particular patient. To obtain such a cocktail, it is necessary to test the patient’s bacteria for sensitivity to phages from the collection in order to select the most effective phage strains. If the required phages are not in the collection, bacteria-specific phages are searched for in natural substrates.
In general, the search for bacteriophages is quite simple: a bacterial culture is exposed to samples from various sources: water bodies, soil, sewage, etc. If the bacteria die, they are separated from the solution by centrifugation, and the remaining solution is tested for activity. The phage is then propagated by growing on an appropriate bacterial culture. Moreover, phages can be lyophilized (vacuum dried) and directly used in capsules. In this form, the drug remains stable for 14 months at temperatures up to 55 °C.
Who is to blame for this?
- Doctors who unreasonably prescribe antibiotics or run YouTube channels “for everyone,” where, in order to increase their popularity, they name specific antibiotics for specific diseases.
- The deplorable state of our domestic medicine with its catastrophic shortage of doctors and ill-conceived organization of outpatient care. Sometimes it is easier to get an appointment with the Queen of Great Britain than with a doctor. Therefore, people are forced to go online and prescribe their own treatment, including antibiotics.
- The Internet, where articles in most cases are written by copywriters - people without medical education who do not understand the importance and seriousness of what they write about.
- Pharmacy employees who easily recommend antibiotics.
And don't tell me there isn't such a thing!
The other day I went to a group for pharmacy employees, and there one man asked how to treat ureaplasma ( although it is not the microbe that needs to be “treated”, but the disease ).
See what your colleagues write:
Friends, this is crazy!!!
With this state of affairs, it won’t be long until we have no antibiotics left, to which microbes are sensitive. The mortality rate will increase many times over!
I urge you, no, I BEG you: do not recommend antibiotics !
And I urge group administrators to at least sometimes use their brains and DELETE such information. She talks about the UNPROFESSIONALISM of pharmacists and pharmacists, since they do not know the principles of rational antibiotic therapy.
You and I work in the most fragile area of human life: health. Let us always remember the main commandment of medicine “DO NO HARM!”
How does a bacteriophage work?
The bacteriophage looks like an alien: a large head, a thin body, which experts call a “tail,” and several legs.
The most important place of the bacteriophage is the head. Everything is like ours. It contains a DNA (or RNA) molecule. It not only stores all the hereditary information about the virus, but also contains detailed “instructions” on how to grow and strengthen.
Bacteriophages are so simple that they cannot even reproduce on their own. To do this they need a bacterial cell.
How does a bacteriophage work?
There are signaling proteins (receptors) on the surface of bacteria. These proteins are different for different bacteria and even strains of bacteria. Each phage can detect only one type of signaling protein. only infect strain of bacteria.
The bacteriophage attaches to the bacterial cell using landing legs and, like a syringe, injects DNA into it from its head.
From this moment on, the bacterium disappears as an individual.
She stops eating, sharing, doing her dark deeds.
She becomes a slave, Isaura, a factory for the production of small cute viruses (young bacteriophages) and, with the help of her resources, begins to synthesize everything necessary for the assembly of new viral particles.
Eventually, there are so many of them, and the bacteria have so few resources that it bursts like a New Year's cracker, and newborn phages go free to search for new victims.
Look:
IMPORTANT:
If the bacteriophage does not find its signaling proteins, it will not attack the bacterium. It is strictly specific.
This leads to the following conclusion:
Bacteriophages are much safer than antibiotics, because They act only on pathogenic bacteria and do not act on beneficial ones, without which the body begins to function incorrectly.
Cost of drugs, where to buy
In pharmacology, there are quite a few types of bacteriophages, with the help of which you can get rid of a diagnosed disease after destroying bacteria and viruses. Modern biotechnological laboratories and production facilities create new medicines that rid the human body of infections without adverse reactions. The cost of bacteriophages depends on the region and the markup of the selected pharmacy chain.
| Drug name | Average price in Russia (RUB) |
| Staphylococcal bacteriophage | 760 |
| Bacteriophage Proteus | 690 |
| Bacteriophage coli | 640 |
| Bacteriophage Pseudomonas aeruginosa | 900 |
| Klebsiella pneumoniae bacteriophage purified | 560 |
| Bacteriophage coliproteus | 670 |
| Pyobacteriophage polyvalent purified | 830 |
| Pyobacteriophage polyvalent (Sextaphage) | 740 |
| Pyobacteriophage complex | 990 |
| Intesti-bacteriophage liquid | 620 |
You can purchase bacteriophages either in a regular pharmacy or online. If the patient has a list of medications to combat bacterial infections and viruses, then to select the appropriate medication, you should study the instructions and also read the reviews.
Differences between bacteriophages and antibiotics
1. The phage “hits” exactly on target, like a sniper. The action of the antibiotic is a “bombing” of an area where there are friends and strangers.
Therefore, antibiotics often cause intestinal dysbiosis. Phages - no.
2. Antibiotics necessarily act on other organs.
Amoxiclav, beloved by many doctors, can lead to antibiotic-associated colitis, hepatitis, and interstitial nephritis.
Cephalosporins damage the liver and kidneys and can cause ulceration of the oral mucosa.
Sumamed also does not have the best effect on the liver and kidneys, and can cause side effects such as palpitations, dizziness, headaches, and drowsiness.
I have collected the differences between antibiotics and bacteriophages
When are bacteriophages prescribed or can they be prescribed?
1. When the pathogen is resistant to all antibiotics.
2. For nosocomial infections. These are infections that occur in a hospital setting. The microbes that cause them have developed resistance to most antibiotics during their stay in hospital rooms. Thousands of patients die every year from diseases that, according to all medical canons, are perfectly treated.
3. If there are contraindications to most antibiotics.
4. If you are allergic to all antibiotics.
And…
1. Pregnant, lactating, newborns.
2. For mild infections, when you can do without an antibiotic, but you cannot do without antibacterial therapy.
3. Elderly people with a bunch of chronic diseases.
4. Together with an antibiotic to reduce its dose or increase its effectiveness, since the bacteriophage will also act on bacteria resistant to this antibiotic.
How to treat staphylococcus
To combat staphylococcus, a set of measures should operate in 3 directions:
- Impact on the source of infection itself by isolating people with staphylococcal infections, sanitizing coccus carriers among doctors and patients with antiseptics: lysozyme, furatsilin, rivanol, etc.
- Elimination of infection, which can be achieved by improving the sanitary and hygienic regime, strict adherence to asepsis and antiseptics in the hospital.
- Strengthening human immunity with the use of immunomodulators, including.
Such treatment with immunodrugs is called immunobiological. These include toxoids, antiphagins, vaccines, bacteriophages, gamma globulin and antistaphylococcal plasma.
Reasons for the limited use of bacteriophages
I see the reasons as follows:
First. Ignorance and misunderstanding of this group of funds.
Second. To prescribe a bacteriophage, you need to do a culture of the flora (stool, urine, throat, nose swab, etc.) and sensitivity to bacteriophages in order to select the optimal one.
Firstly, this analysis is not cheap, and secondly, the results will be ready in 4-7 days . In some situations, it is impossible to leave the patient without antibiotic therapy for this time.
Third. There are no clear guidelines for the use of bacteriophages for specific diseases: where, how and how much? Therefore, doctors' prescriptions are often empirical in nature.
Let’s say the doctor prescribed Sextafag into the nose, 2 drops 3 times a day. He was not satisfied with the result, and he increased the dose, for example, to 4 drops 3 times a day. But the best thing about working with phages is that it is difficult to harm the patient by increasing the dose.
Fourth. Treatment with phages, as a rule, is not included in the clinical recommendations of the Ministry of Health for the treatment of various diseases, because there are insufficient clinical studies proving the effectiveness of bacteriophages. And because we have been accustomed to using antibiotics for decades.
Fifth. Long-term course of treatment with phages: 1-2-3 weeks, more if necessary.
Sixth. It is easier to prescribe an antibiotic than to prescribe a culture, select a dose of phage, describe and explain how to use it.
Seventh. A course of treatment with bacteriophage costs a tidy sum. For many people this is unaffordable.
Interaction with other pharmaceuticals
Does not affect the therapeutic effect of other pharmaceuticals. After using disinfectants to disinfect affected tissues, a high-quality rinse with a sterile saline solution is required before introducing the bacteriophage.
Effect on driving and nervous system function
Does not have a negative effect on driving. Does not depress the central and peripheral nervous system. Not contraindicated for work involving excessive concentration. Not addictive.
Use for the treatment of pregnant and lactating women
There are no restrictions on the use of the drug in the treatment of pregnant women and nursing mothers in doses acceptable for an adult patient.
What diseases can be treated with phages?
- Bacterial infections of the ENT organs: sore throat, pharyngitis, laryngitis, rhinitis, sinusitis.
- Bacterial infections of the respiratory system: tracheitis, bronchitis, pneumonia, pleurisy.
- Surgical infections: wound suppuration, burn, abscess, phlegmon, trophic ulcer, bedsores, boil, carbuncle, panaritium, paraproctitis, mastitis, osteomyelitis, etc.
- Infections of the genitourinary system: urethritis, cystitis, pyelonephritis, vaginitis (colpitis), endometritis, adnexitis, etc.
- Intestinal infections.
- Intestinal dysbiosis.
- Infectious eye diseases (conjunctivitis, purulent corneal ulcers, etc.).
- Purulent-inflammatory diseases of newborns: omphalitis (inflammation of the umbilical wound), pyoderma (pustules on the body), conjunctivitis, sepsis, etc.
Types of bacteriophages
There are two types of bacteriophages:
1. Against different strains of the same pathogen: staphylococcal, streptococcal, dysentery, etc.
2. Against two or more pathogens: Sextaphage , Intesti-bacteriophage , Pyobacteriophage , etc.
Let me explain a little.
Ideally, for each disease, it is necessary to identify the pathogen and determine its sensitivity to bacteriophages.
In practice, it happens that there is no time to wait. Therefore, “cocktails” of bacteriophages are created that act on different types of bacteria or on different strains of the same bacterium.
These are the “polyvalent” bacteriophages: Sextaphage , Piobacteriophage , Klebsiella polyvalent bacteriophage , etc.
In such a “cocktail”, different bacteriophages feel great, do not fight and do not interfere with each other in dealing with their bacteria.
Today there are not so many bacteriophages:
When I began to understand this topic, I wrote to Microgen, naively believing that they would answer my questions, of which I had accumulated many.
For example:
- Why are some bacteriophages called polyvalent and others complex? What's the difference?
- Why is the word “polyvalent” missing from the name “ Intesti-bacteriophage ”, although it acts on several bacteria?
- Why do some have the word “purified” in their names, while others don’t?
- What is the difference between Piobacteriphage polyvalent and Sextafag if they act on the same bacteria?
But they didn’t answer me. Maybe they were afraid that some of my questions would be followed by others, and they would not be able to answer them? I'm digging deep.
Moreover, I noticed that after my letter to them, information about several bacteriophages disappeared from the site. For example, about the Klebsiella pneumoniae bacteriophage.
What does it mean?
Does this mean that it has ceased to be produced, and it can be replaced with Klebsiella polyvalent bacteriophage, Piobacteriophage or Sextaphage, which also act on this pathogen?
Well, God be with them.
Let's return to the table.
What conclusion can be drawn from this?
Several bacteriophages are suitable to influence the same pathogen.
Recently in our VKontakte group there was a question about whether it is possible to replace the Klebsiella pneumonia bacteriophage with purified polyvalent Klebsiella bacteriophage?
In theory it is possible. Especially if the patient was not tested for sensitivity to the bacteriophage, but the pathogen Klebsiella pneumonia was simply cultured.
But given that this bacteriophage was prescribed by a doctor, a non-synonymous replacement cannot be made.
Indications for use
The main purpose of bacteriophages is to destroy pathogenic microorganisms. Pharmacological drugs manufactured on their basis are increasingly included in complex therapy in the treatment of various infectious diseases.
When used correctly, bacteriophages help cope with various types of pathologies:
- Urogenital diseases.
- Surgical pathologies.
- Enteral diseases.
- Pathologies of ENT organs.
- Infectious lesions of the respiratory tract.
A suitable bacteriophage is prescribed only by a doctor after a comprehensive examination of the patient and identification of infection. Uncontrolled use of such drugs may be ineffective, since it is impossible to determine sensitivity to viruses without a special laboratory analysis.
If a patient has been diagnosed with a severe infectious disease, then he should be prescribed complex therapy. Staphylococcal bacteriophage can be used for regular treatment of postoperative wounds, as well as to reduce the likelihood of developing intrauterine infections according to existing epidemic indications.
What is the drug bacteriophage?
This is a transparent yellow solution, which, depending on the type of phage and the disease, is prescribed orally, rectally in the form of enemas, locally in the form of washings, instillations, lotions, rinses, moistened turundas, injection into the pleural, articular cavity, bladder cavity, uterus, etc. vagina.
If necessary, phages are used in nebulizers, but not ultrasonic ones.
Among bacteriophages there are especially popular ones. These are Staphylococcal bacteriophage, Pyobacteriophage, Sextaphage .
Sextaphage , for example, is often prescribed for sinusitis, prolonged green snot, laryngitis, tonsillitis, purulent conjunctivitis, absence of stool in a newborn, bloating (if microbes sensitive to the phage, for example, staphylococcus, are inoculated).
Staphylococcus aureus
Staphylococcus aureus (Staphylococcus aureus) is the most pathogenic for humans. It got its name because it forms a dense golden-colored coating (a special pigment) on nutrient media, while other bacteria are colorless. It is the causative agent of all kinds of inflammation of a purulent nature, without exception, in any tissue. It can affect the skin, soft tissues, respiratory, bone, joint, endovascular systems, and causes many pathologies: from acne to sepsis. Even today, it is one of the four most aggressive sources of nosocomial infections, especially in post-operative wound complications.
Examples of the use of bacteriophage in various diseases
Sextafag, or Pyobacteriophage polyvalent, usually prescribed ?
In the nose, in the ear for purulent otitis media, in the eyes: 2-3 drops 2-4 times a day, undiluted. Warm it in your hand first!
With clear nasal discharge against the background of ARVI, bacteriophages are ineffective, because they have no application point.
But for bacterial rhinitis, when the snot becomes “colored”, it will come in handy.
The second method is to moisten a cotton pad into the ear and leave for an hour.
Gargling: 10-20 ml at a time. The bacteriophage was drawn up with a syringe, held in the hand, warmed, and poured into a glass to make it easier to take into the mouth. And so 2-3 times a day. There is no need to breed.
Inhalations through a nebulizer, but not ultrasonic: for laryngitis, bronchitis, pneumonia - 5 ml undiluted 1 time per day. The solution is sterile, and when used correctly, sterility is not compromised.
In case of sinusitis, the doctor additionally rinses the paranasal sinus with a bacteriophage.
Orally: depending on age, 5-30 ml 3 times a day an hour before meals (the instructions contain a table by age). For small children, it can be diluted in water, although the bacteriophage does not taste bad. It happens that a child vomits from delicious syrup, but he drinks the bacteriophage just fine.
For intestinal infections, the doctor can replace one oral dose by administering the drug through a “high” enema using a gas tube or catheter: 10-50 ml at a time, depending on age.
For cystitis, take orally. For chronic cystitis, the bacteriophage can be injected by a doctor directly into the bladder.
For stomatitis and periodontitis, take 10-20 ml of bacteriophage in your mouth and rinse. And so 3-4 times a day.
For trophic ulcers, bedsores, and purulent wounds, Pyobacteriophage, Sextaphage or Staphylococcal bacteriophage are more often used - in case of sensitivity of the pathogen. Moisten a gauze pad with the solution, apply it to the wound and fix it. Dressings are carried out daily or 2 times a day.
Intesti-bacteriophage is used to treat various intestinal infections: dysentery, salmonellosis, enterocolitis, colitis, or to correct disorders of the intestinal microflora. Although in the latter case, the doctor may prescribe Staphylococcal bacteriophage g, and Piobacteriophage , and Sextaphage - again, depending on the pathogen and its sensitivity to the phage.
It is used orally in age-specific dosages (they are indicated in the instructions) 30 minutes before meals or as an enema (if the patient vomits from any drug taken by mouth).
Or the doctor will prescribe taking it 2 times orally and 1 time as a “high” enema using a gas outlet or catheter.
The use of bacteriophages in clinical practice: the Renaissance
For citation. Kostyukevich O.I. The use of bacteriophages in clinical practice: the Renaissance // RMJ. 2015. No. 21. pp. 1258–1262.
Prerequisites for the use of bacteriophages Today, bacterial infections represent an extremely pressing health problem. And the reasons for this are not only increasing antibiotic resistance, but also the extremely negative health consequences of irrational antibiotic therapy.
Antibiotic resistance In recent years, virtually no new antibacterial drugs (ABPs) have appeared, while resistance to “old” ABPs is steadily increasing and in many cases has already reached a critical level. WHO draws attention to the fact that many discoveries in the field of drug treatment made in the 20th century may lose their significance due to resistance to ALD. As a result, most infectious diseases can simply get out of control [1]. The greatest danger is posed by hospital infections, now referred to as healthcare-associated infections (HAI), the prevalence of which already reaches 5–10% of the number of patients in hospitals, and mortality ranks tenth among the causes of mortality in the population [2]. However, the treatment of these diseases is extremely difficult due to the high incidence of antibiotic resistance (50–99%).
Difficulties in treating chronic infections with traditional antibiotics “Chronic infections... are very difficult, if not impossible, to treat with antibiotics” [3]. One of the significant reasons for the low effectiveness of therapy for chronic infections is the formation of biofilms, which prevent the penetration of antibiotics. In this regard, great hopes are placed specifically on bacteriophages, which work in this situation according to the “Trojan horse” principle: by infecting one bacterial cell, they penetrate with it under the biofilm, and after the death of the carrier cell, a large number of newly synthesized phages enter the colony, damaging other bacteria [3]. In addition, bacteriophages stimulate the activation of specific and nonspecific immunity factors [4, 5], which enhances their effectiveness in the treatment of chronic infections.
Side effects of antibiotic therapy In addition, clinicians in their practice are increasingly faced with unsatisfactory tolerability of antibiotics. Thus, the frequency of antibiotic-associated diarrhea has increased significantly in recent years and ranges from 2 to 30%, depending on the antibiotic used [6]. More and more patients are refusing to take ABP due to the development of side effects or due to fear (sometimes well-founded) of intestinal dysbiosis. And increasingly, unfortunately, we are faced with a violation of the principles of rational antibiotic therapy on the part of doctors themselves, which, of course, aggravates the situation with both resistance to ALD and the safety of antibiotic therapy. In this regard, the key tasks are the development and introduction into clinical practice of additional means of combating infectious diseases, which, undoubtedly, can be considered bacteriophages.
Bacteriophage (bacteria + Greek phagos - devouring; synonym: phage, bacterial virus) is a virus that selectively infects bacteria. Bacteriophages are widespread in nature; every gram of soil, every cubic centimeter of water and air, food, plants and animals contain millions of phage particles (from 10 to 100 million). These are the oldest inhabitants of the planet and are natural limiters of the spread of bacteria.
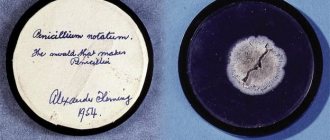
History of the creation and use of bacteriophages The history of the discovery of bacteriophages dates back to 1896, when the British chemist E. Hankin, studying the antibacterial effect of the waters of the Indian rivers Ganga and Jumna, first described certain agents that easily pass through membrane filters impenetrable to bacteria and cause the death of microbes . In 1917, an employee of the Pasteur Institute in Paris, F. D'Herelle, proposed the name “bacteriophages” - bacteria eaters; he later determined that they are bacterial viruses capable of causing specific lysis of bacteria [7].
In 1921, D. Masin and R. Bryong first described a successful method of treating staphylococcal skin infections using staphylococcal phage. Until the middle of the twentieth century. In the West, bacteriophages have been widely studied and effectively used as a therapeutic agent against a number of diseases, including dysentery, typhoid, paratyphoid, cholera and purulent-septic infections. However, since the discovery of penicillin by A. Fleming in 1928, a new era in the fight against infectious diseases began - the era of antibiotics. And bacteriophages, which at that time turned out to be less effective, were consigned to oblivion in the Western world. In the USSR, the development and research of bacteriophage preparations did not stop and were actively supported at the highest level. In the 1930s The Institute for Bacteriophage Research was created in Tbilisi, which in 1951 became part of the group of institutes for vaccines and serums. The literature indicates that in the USSR in 1930–1940. Phage therapy was actively used to treat a wide range of bacterial infections in the field of dermatology (Beridze, 1938), ophthalmology (Rodigina, 1938), urology (Tsulukidze, 1938), dentistry (Ruchko and Tretyak, 1936), pediatrics (Alexandrova, 1935; Lurie, 1938 ), otolaryngology (Ermolieva, 1939) and surgery (Tsulukidze, 1940, 1941). These articles were published in Russian and were not available to Western scientists. Nevertheless, past experience indicates the high effectiveness of phage therapy and prevention.
We can proudly admit that Russia has always occupied a leading position in the production and use of therapeutic and prophylactic bacteriophages. Production did not stop during the era of “worldwide cooling” to phage therapy and actively developed even during the Great Patriotic War. Thus, NPO Microgen has been producing bacteriophages since the 1940s. In Russia and on the territory of some former Soviet republics, bacteriophage therapy is actively used to this day. Penicillin was the first medicine to demonstrate the emergence of bacterial resistance to antibiotics, which is now increasing exponentially. Skepticism in the West towards phage therapy gave way to increased interest in it, and a new wave of research began [8]. In addition to Russia, which has the richest experience in the use of bacteriophages, researchers in other countries have also actively studied the possibilities of phage therapy [9–12].
Clinical use of bacteriophage preparations at present Phage therapy from the perspective of evidence-based medicine Over the past 10 years, the number of publications in the world's leading medical publications addressing the issues of therapeutic and prophylactic use of bacteriophages has increased several times and has already exceeded 3000 (in the PubMed database). The number of recently published works indicates a revival of interest in phage therapy. Recently completed clinical studies provide compelling evidence regarding the safety and effectiveness of phage therapy in animals and humans [13–15]. Dual therapy using phages and antibiotics led to significantly better results than monotherapy with antibiotics [16]. It has been shown that bacteriophages may be more effective than traditional antibiotics in destroying bacterial biofilms [17].
Bacteriophages are now called “the bright hope in the era of antibiotic resistance.” At the initiative of the leading US food and drug control organization, the Food and Drug Administration (FDA), active clinical trials of bacteriophage drugs have been underway since 2007 [18, 19]. In recent years, the FDA has approved the use of phage preparations as food additives (eg, Listex, EcoShield) [20]. European regulatory authorities are currently considering phages as biological agents, requiring further randomized trials. The current data, although encouraging, are considered insufficient to create international clinical guidelines for phage therapy.
Mechanism of action of bacteriophages The antibacterial effect of bacteriophages is due to the introduction of the phage genome into the bacterial cell, followed by its reproduction and lysis of the infected cell. Bacteriophages released into the external environment as a result of lysis re-infect and lyse other bacterial cells, acting until the pathogenic bacteria in the inflammation site are completely destroyed.
Advantages of phage therapy Thus, based on the accumulated data, the following prerequisites for the widespread use of bacteriophage preparations for therapeutic and prophylactic purposes can be formulated: 1. Efficiency in the treatment of infections caused by antibiotic-resistant bacteria, including HAIs. 2. Possibility of use for allergic reactions to ABP. 3. Low toxicity, allowing them to be considered the safest drugs, which determines the possibility of their widespread use in children, pregnant and lactating women. 4. High specificity (no effect on normal human microflora) provides a significant advantage in the treatment of any infectious diseases in patients with various disorders of the intestinal microflora (including bacterial overgrowth syndrome (SIBO) and other dysbioses), the prevalence of which in recent years has increased significantly over the years. 5. Highly effective in the treatment of chronic infections, especially those associated with the formation of bacterial biofilms. 6. Possibility of use in various forms: local applications, liquid and tablets; parenteral.
Limitations of phage therapy At the same time, bacteriophages are currently used in real practice much less frequently than one would expect, given the large amount of positive information. The following reasons can be identified that limit the use of bacteriophages: 1. First of all, this is the lack of regulatory documents and insufficient awareness of specialists [21]. 2. There are still some bacteria pathogenic for humans (according to the approved list of biological agents [22]), for which lytic phages have not yet been found, including representatives of the 3rd biosafety level, such as Rickettsia, Ehrlichia and Coxiella ( causative agents of ehrlichiosis, epidemic typhus, Rocky Mountain fever). 3. Production of antiphage antibodies. The problem of immune interaction between the human body and phages is still under study. The smallest amount of antibodies to bacteriophages is produced in newborns and infants, which determines the greatest effectiveness of phage therapy in this group. 4. Quite rare, but still there are side effects of phage consumption, which are usually associated with massive breakdown of bacterial cells with the release of endotoxin. To be fair, it should be noted that such effects are much more significant with antibiotic therapy. In most cases, these adverse events can be mitigated with the help of enterosorbents.
Principles of rational phage therapy It should be noted that the use of bacteriophages, like any ABP, should be based on rational principles. 1. Preliminary determination of the sensitivity of bacteria to the drug and the lytic activity of bacteriophages in the laboratory. All bacteriophages can be divided into moderate and virulent (or lytic). A. Temperate bacteriophages incorporate their genetic material into bacterial chromosomes and multiply synchronously with the host cell, without causing lysis for a long time. Temperate bacteriophages play a significant role in the evolution of bacteria, contributing to the acquisition of additional virulence factors and antibiotic resistance by pathogens. It has now been proven that many virulence factors in pathogenic bacteria are encoded precisely with the help of prophage genes. B. Virulent phages always lead to the destruction of bacteria (lytic effect) and the release of mature phage particles that infect new bacterial cells. In this regard, bacteriophages used to treat infectious diseases must be exclusively virulent, i.e., lead to the death of bacteria. The lytic activity of bacteriophages prescribed for treatment must be previously tested in the laboratory. 2. The choice of delivery system plays a key role in successful phage therapy. Recent advances in phage therapy indicate that local (targeted) delivery has been more successful for localized infections, while the parenteral route is recommended for systemic infections [23]. When using oral forms of drugs, it is necessary to take into account the sensitivity of phages to the action of gastric hydrochloric acid and, in this case, give preference to delivery in an acid-resistant shell.
Bacteriophage preparations and their use in clinical practice Today there is an extensive list of phage preparations used in the treatment of a wide range of bacterial infections. On the territory of the Russian Federation, the only drugs registered as medicines are bacteriophages from the NPO Microgen. The main drugs and the spectrum of their antimicrobial action are presented in Table 1 [24].
The use of bacteriophages for gastrointestinal diseases Treatment of gastrointestinal infections with bacteriophages has a significant advantage over antibiotics in terms of the effect on normal intestinal microflora. Phage therapy has been shown to be effective against pathogens of gastrointestinal tract infections such as enteropathogenic E. coli [25], S. sonnae, flexneri, Salmonella E, P. vulgaris, mirabilis, S. aureus, P. aeruginosa, Enterococcus, etc. In the practice of a gastroenterologist it is possible distinguish 2 main groups of patients for whom bacteriophage therapy may be indicated: 1) with acute bacterial infections (acute gastroenteritis, gastroenterocolitis); 2) with various disturbances of normal intestinal microflora (SIBO in the small intestine, colon dysbiosis), which occur to one degree or another in most patients with gastrointestinal diseases.
Phage therapy of acute bacterial diarrhea Treatment of acute bacterial diarrhea sometimes presents significant difficulties due to the low effectiveness of antibacterial drugs and the development of side effects. It has been shown that due to the effect of antibiotics on normal intestinal microflora, the mechanism of natural colonization resistance is inhibited. In addition, the direct mechanism of the immunosuppressive effect of antibiotics is known. All this can lead to long-term persistence of the causative agent of acute intestinal infection (AI) during antibiotic therapy [26, 27]. Thus, according to some studies, in patients who received ABP in the acute phase of salmonellosis, subsequent bacterial excretion of Salmonella was significantly more common in comparison with individuals who received only pathogenetic therapy [28]. Indications for the use of bacteriophages in acute intestinal infections today can be formulated as follows: – as monotherapy – in mild forms of acute intestinal infections; – in combination with antibacterial therapy or sequentially – for moderate and severe forms of acute intestinal infections; – during bacterial excretion (in convalescent or transient bacterial carriers); – in the complex therapy of enterocolitis of opportunistic and staphylococcal etiology; – to correct disorders of intestinal microbiocenosis [29]. A prerequisite for phage therapy is stool culture with determination of phage sensitivity. In the case of an unverified pathogen, preference should be given to complex preparations of bacteriophages (intesti-bacteriophage), which have a wide spectrum of action against pathogens of major intestinal infections.
Phage therapy for SIBO One of the promising, but so far little-studied areas is the correction of disorders of the normal intestinal microflora with bacteriophage preparations. As is known, SIBO is clearly associated with the use of ABP. At the same time, if there are signs of bacterial overgrowth in the intestine, the only recommended tactic today is the prescription of antibiotics or intestinal antiseptics. This, of course, causes bewilderment for both patients and sometimes doctors themselves. It turns out that we are “treating complications of antibiotic therapy with antibiotics”... And in this case, phage therapy can have significant advantages, targeting opportunistic microorganisms that are “out of control”. A prerequisite before starting therapy is stool culture to determine sensitivity to phage drugs. Preference should be given to complex drugs that affect pathogenic and opportunistic intestinal microflora (intestinal bacteriophage).
Prospects for the use of bacteriophages We are on the threshold of the “Renaissance” of bacteriophage therapy, which opens up new prospects in the treatment of antibiotic-resistant microflora and also has a good safety profile. In Russia today, phage therapy is successfully used for a wide range of diseases, and, of course, justifies itself in various disorders of the intestinal microflora. The targeted action of the drugs allows us to maintain a fine line of normal flora balance, which is extremely important for our patients.
How to use bacteriophage correctly?
Phages are gentle guys. They like temperatures of 2-8 degrees, so they should be stored in the refrigerator.
Today they are available in the form of a solution in 100 ml bottles and 20 ml bottles, 4 pieces per pack.
To collect the required amount of phage from the vial, you need to open the central part of the cap. Underneath there is a rubber stopper.
Treat it with alcohol and insert a needle of a disposable syringe with a volume of 5-10 ml (the volume of the syringe depends on the single dose).
Draw up the required amount of phage, disconnect the syringe from the needle, and hold it in your hand to warm it.
Next, place in a clean container and take orally. Or take the required amount with a pipette. Or moisten a gauze pad with phage. Or take it into your mouth to gargle.
The needle remains in the rubber stopper until the bottle is empty.
For another bottle, take another syringe.
The bottle with a needle stuck into it is stored in the refrigerator.
However, if the bacteriophage is prescribed for oral administration and in an enema, you don’t have to bother with the syringe, open it, take the required amount, close it with a rubber stopper and place it in the refrigerator. Do not place the rubber stopper with the inside on the table and do not leave the bottle open.
Before opening the bottle, you need to shake it and see if the solution has become cloudy. It should be transparent.
The clear solution can be used throughout the expiration date.
Answers to the most frequently asked questions
Is it possible to overdose on a bacteriophage?
Cases of overdose have not been described. In the body, the phage is sent to the source of infection, where there is its victim. It multiplies as long as HIS bacteria exist. After this, it is eliminated from the body naturally.
Is resistance to phages developing?
According to specialists from NPO Microgen, resistance to them does not develop. First of all, because they themselves are constantly evolving. But you can find publications on the Internet where this statement is disputed.
How often can I take Bacteriophages?
As often as required.
Is it possible to take phage together with other drugs?
Bacteriophages are compatible with any drugs.
Are there any side effects from phages?
Rarely. The bacteriophage contains a preservative; there may be an individual intolerance to it.
Is it possible to use Bacteriophage without testing the sensitivity of the pathogen to it?
It's possible if you don't mind the money. This pathogen may be insensitive to the phage. Each bacterium has several strains (varieties); one strain may be sensitive to the phage, while another may not.
Can bacteriophages be recommended to customers?
Theoretically, polyvalent phages ( Sextaphage , Piobacteriophage ) can be recommended, especially since these drugs are over-the-counter. But in practice, a phage may be ineffective if the pathogen is insensitive to it.
To whom will they come with complaints?
Right! To you.
So, it is better to let the doctor take responsibility for prescribing the phage.
Why might a phage be ineffective?
1. No analysis was done for flora and sensitivity to bacteriophage.
2. Inadequate dosage. Or the doctor chose not the best method of introducing the bacteriophage in this particular situation.
3. We didn’t finish treatment. Average course of phage treatment: 7-14 days. If necessary, the doctor can extend it.
4. The conditions of storage and use were violated.
5. Some microorganisms are capable of forming biofilms in organs. These are conglomerates of bacteria where neither phages nor antibiotics can penetrate.
How to transport phages correctly?
The manufacturer writes that transportation at temperatures from 9 to 25 degrees is allowed for no more than 1 month.
What is Otofag, Fagodent, Fagoderm, Fagogin?
These are cosmetic gels with bacteriophages for hygiene and normalization of the microflora of the ear, oral cavity, intimate area, skin and soft tissues. They are not produced by NPO Microgen, but by another company.
What is better: to use a phage together with an antibiotic or separately?
In each specific situation, this is decided by the doctor. My opinion: if they are used together, it still will not protect against the negative consequences of using an antibiotic. Therefore, if you can do without an antibiotic, it is better to use one bacteriophage.
Contraindications
Bacteriophages are prohibited from being taken by patients who have individual intolerance to the components included in the composition. To reduce the likelihood of adverse reactions, you should consult in advance with your doctor, who will help you draw up a treatment regimen and prescribe the dosage.
If the drug was stored in improper conditions, then its further use is unacceptable. The positive therapeutic properties of the drug are preserved provided that the patient stores the opened bottle in a cool place.