Pharmacodynamics and pharmacokinetics
The drug is used to prevent bronchospasms . It is a bronchodilator, or more precisely, a selective beta-2-adrenergic agonist . It increases the vital capacity of the lungs and mucociliary clearance , activates the ciliated epithelium, improves mucus secretion, dilates the coronary arteries, reduces potassium content, acts as a hyperglycemic and lipolytic agent, affects glycogenolysis and insulin secretion, and increases the risk of acidosis .
The medicine acts quite quickly, almost 5 minutes after application (maximum - after 30-90 minutes). The duration of the effect is about 5 hours.
10-20% of salbutamol after use ends up in the lower respiratory tract. They are absorbed into the lung tissue and blood, but are not broken down. The remaining amount of the active substance is retained in the inhaler or in the oropharynx, after which it is swallowed and actively broken down when passing through the liver and is converted into phenolic sulfate .
The degree of binding to plasma proteins is approximately 10%.
Salbutamol entering the blood is broken down within 72 hours in the liver and is excreted mainly in the urine in the form of phenolic sulfate or unchanged. A small part is excreted in the feces.
How to breathe Ventolin through a nebulizer
With frequent use of a bronchodilator, addiction may occur. The drug should not be used unless absolutely necessary. The medicine is prescribed only in the presence of attacks of respiratory failure.
Basic Rules:
- The procedure is performed in case of an acute attack of suffocation, as well as to prevent it due to the negative impact of irritating factors.
- If mucolytic drugs are prescribed in parallel during complex treatment, inhalations with Ventolin are initially given. After 30-60 minutes you can breathe in expectorant medications.
- Breathing should be smooth and deep. There is no need to breathe often, as the unpleasant symptoms will intensify.
- If the procedure is prescribed once a day, it is done in that half of the day in which the cough is more disturbing.
After inhalation, do not drink or eat for 1 hour. It is allowed to go outside in any weather 2 hours after the breathing event.
Side effects
As a rule, side effects include finger tremor headache , and anxiety. In addition, the following undesirable reactions are possible:
- hypersensitivity in the form of urticaria , hypotension , Quincke's edema , bronchospasm , collapse ;
- hyperactivity;
- paradoxical bronchospasm;
- muscle cramps;
- hypokalemia;
- lactic acidosis;
- tachycardia;
- strong heartbeat;
- dilatation of peripheral vessels;
- arrhythmia;
- extrasystole;
- supraventricular tachycardia;
- irritation of the mucous membrane of the mouth and pharynx.
Ventolin aerosol d/inhaled dose 100 mcg/dose 200 doses 17812
Description
Metered-dose inhalation aerosol: an aluminum inhaler equipped with a plastic dispensing device with a protective cap, containing a white or almost white suspension. After inhalation administration, 10–20% of the dose of salbutamol reaches the lower respiratory tract. The rest of the dose remains in the inhaler or is deposited in the oropharynx and is then swallowed. The fraction deposited in the respiratory tract is absorbed into the lung tissue and blood, but is not metabolized in the lungs. The degree of binding of salbutamol to plasma proteins is about 10%. Once in the blood, salbutamol is metabolized in the liver and excreted, mainly in the urine, unchanged or in the form of phenolic sulfate. The ingested portion of the inhalation dose is absorbed from the gastrointestinal tract and undergoes active metabolism during the first passage through the liver, turning into phenolic sulfate. Unchanged salbutamol and the conjugate are excreted primarily in the urine. Salbutamol administered intravenously has a T1/2 of 4–6 hours. It is excreted partly by the kidneys and partly as a result of metabolism to inactive 4′-O-sulfate (phenolic sulfate), which is also excreted mainly in the urine. Only a small part of the administered dose of salbutamol is excreted in feces. Most of the dose of salbutamol administered intravenously, orally or by inhalation is excreted within 72 hours. Salbutamol is a selective β2-adrenergic receptor agonist. In therapeutic doses, it acts on β2-adrenergic receptors of bronchial smooth muscle, having little or no effect on β1-adrenergic receptors of the myocardium. It has a pronounced bronchodilator effect, preventing or relieving bronchospasm, and reduces resistance in the respiratory tract. Increases vital capacity of the lungs. Increases mucociliary clearance (in chronic bronchitis up to 36%), stimulates mucus secretion, activates the functions of the ciliated epithelium. At recommended therapeutic doses it does not have a negative effect on the cardiovascular system and does not cause an increase in blood pressure. To a lesser extent, compared to drugs of this group, it has a positive chrono- and inotropic effect. Causes dilation of the coronary arteries. It has a number of metabolic effects: it reduces the concentration of potassium in plasma, affects glycogenolysis and insulin secretion, has a hyperglycemic (especially in patients with bronchial asthma) and lipolytic effect, and increases the risk of developing acidosis. After using inhalation forms, the action develops quickly, the onset of the effect is after 5 minutes, the maximum is after 30–90 minutes (75% of the maximum effect is achieved within 5 minutes), duration is 4–6 hours. Patients should be instructed on the correct use of the Ventolin® inhaler . Bronchodilators should not be the only or main component of the treatment of unstable or severe bronchial asthma. If the effect of the usual dose of Ventolin® becomes less effective or shorter lasting (the effect of the drug should last at least 3 hours), the patient should consult a doctor. An increased need for the use of inhaled β2-adrenergic agonists with a short duration of action to control the symptoms of bronchial asthma indicates an exacerbation of the disease. In such cases, the patient's treatment plan should be reconsidered. A sudden and progressive deterioration of bronchial asthma can pose a threat to the patient's life, therefore, in such situations, it is necessary to urgently decide on prescribing or increasing the dose of GCS. In such patients, daily monitoring of peak expiratory flow is recommended. Salbutamol should be used with caution in patients with thyrotoxicosis. Therapy with β2-adrenergic agonists, especially when administered parenterally or via nebulizer, can lead to hypokalemia. Particular caution is recommended when treating severe attacks of bronchial asthma, since in these cases hypokalemia may increase as a result of the simultaneous use of xanthine derivatives, corticosteroids, diuretics, as well as due to hypoxia. In such situations, it is necessary to monitor the level of potassium in the blood serum. Impact on the ability to drive a car and/or other mechanisms. No data.
Compound
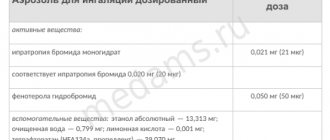
Aerosol for inhalation dosed 1 dose active substance: salbutamol sulfate 120.5 mcg (equivalent to 100 mcg of salbutamol) excipients: tetrafluoroethane - 1 dose in an aluminum aerosol can (complete with dosing device); 1 cylinder in a cardboard pack.
Application
bronchial asthma: - relief of attacks of bronchial asthma, incl. with exacerbation of severe bronchial asthma; - prevention of bronchospasm attacks associated with exposure to an allergen or caused by physical activity; - use as one of the components in long-term maintenance therapy of bronchial asthma; COPD accompanied by reversible airway obstruction; chronic bronchitis. The drug is prescribed to pregnant women only when the expected benefit to the patient outweighs the potential risk to the fetus. During post-registration surveillance, rare cases of various malformations in children, including the formation of a cleft palate and malformations of the limbs, were identified when mothers took salbutamol during pregnancy. In some of these cases, mothers took multiple concomitant medications during pregnancy. A cause-and-effect relationship with taking the drug has not been established. Salbutamol is likely to pass into breast milk and is therefore not recommended for use in nursing women unless the expected benefit to the patient outweighs the potential risk to the baby. There is no data on whether salbutamol present in breast milk has a harmful effect on the newborn. Adverse reactions are listed depending on the anatomical and physiological classification and frequency of occurrence, which is defined as follows: very often (≥1/10), often (≥1/10) 100 and <1/10), sometimes (≥1/1000 and <1/100), rarely (≥1/10,000 and <1/1000) and very rarely (<1/10,000), including isolated cases. From the immune system: very rarely - hypersensitivity reactions, including angioedema, urticaria, bronchospasm, hypotension and collapse. Metabolic disorders: rarely - hypokalemia (therapy with β2-agonists can lead to significant hypokalemia); very rarely - lactic acidosis. Very rare cases of lactic acidosis have been reported in patients receiving IV salbutamol and Ventolin Nebula to treat exacerbations of asthma. From the nervous system: often - tremor, headache; very rarely - hyperactivity. From the cardiovascular system: often - tachycardia; sometimes - strong heartbeat (pulsation, palpitation); rarely - dilatation of peripheral vessels; very rarely - arrhythmia, including atrial fibrillation, supraventricular tachycardia and extrasystole. From the respiratory system, chest and mediastinal organs: very rarely - paradoxical bronchospasm. From the gastrointestinal tract: sometimes - irritation of the mucous membrane of the mouth and pharynx. From the musculoskeletal system: sometimes - muscle cramps. It is not recommended to use salbutamol and non-selective beta-adrenergic receptor blockers, such as propranolol, at the same time. Salbutamol is not contraindicated in patients receiving MAO inhibitors. In patients with thyrotoxicosis, it enhances the effect of central nervous system stimulants and tachycardia. Theophylline and other xanthines, when used simultaneously, increase the likelihood of developing tachyarrhythmia; agents for inhalation anesthesia, levodopa - severe ventricular arrhythmia. Simultaneous administration with anticholinergic drugs (including inhaled ones) may increase intraocular pressure. Diuretics and corticosteroids enhance the hypokalemic effect of salbutamol. Inhalation. Only a doctor can decide whether to increase the dose or frequency of use of the drug. It is not recommended to use the Ventolin® inhaler more than 4 times a day. The need for frequent use of maximum doses of Ventolin® or a sudden increase in dose indicates a worsening of the disease. Adults (including elderly patients) Relieving an attack of bronchospasm: the recommended dose is 100–200 mcg (1–2 inhalations). Prevention of bronchospasm attacks associated with exposure to an allergen or caused by physical activity: the recommended dose is 200 mcg (2 inhalations) 10–15 minutes before exposure to the provoking factor. Long-term maintenance therapy: the recommended dose is up to 200 mcg (2 inhalations) 4 times a day. Children Relieving an attack of bronchospasm: the recommended dose is 100–200 mcg (1–2 inhalations). Prevention of bronchospasm attacks associated with exposure to an allergen or caused by physical activity: the recommended dose is 100–200 mcg (1–2 inhalations) 10–15 minutes before exposure to the provoking factor. Long-term maintenance therapy: the recommended dose is 200 mcg (2 inhalations) 4 times a day. Ventolin® can be administered through the Babyhaler spacer. Instructions for using the inhaler Checking the inhaler: before using the inhaler for the first time or if the inhaler has not been used for a week or longer, remove the cap from the mouthpiece by lightly squeezing the cap on the sides, shake the inhaler well and press the aerosol valve to release 1 inhalation dose per air to make sure the inhaler is working properly. Using the inhaler 1. Remove the cap from the mouthpiece by lightly squeezing the cap from the sides. 2. Inspect the mouthpiece inside and out to make sure it is clean. 3. Shake the inhaler well. 4. Hold the inhaler between your index finger and thumb in a vertical position, bottom up, with your thumb resting on the base under the mouthpiece. 5. Exhale slowly, deeply, wrapping your lips around the mouthpiece without squeezing it with your teeth. 6. Inhaling as deeply as possible through your mouth, simultaneously press the top of the inhaler to release 1 inhalation dose of salbutamol. 7. Hold your breath for a few seconds, remove the mouthpiece from your mouth, then exhale slowly. 8. To receive the second dose, hold the inhaler in an upright position, wait about 30 seconds and then repeat steps 3–7. 9. Close the mouthpiece tightly with the protective cap. Attention! When following steps 5, 6 and 7, you should not rush. You should begin inhaling as slowly as possible, just before pressing the inhaler valve. It is recommended to practice in front of a mirror the first few times. If a “fog” is visible coming from the top of the inhaler or from the corners of the mouth, then you should start over from step 3. If the doctor has given other instructions for using the inhaler, then you should strictly follow them. You should contact your doctor if you have difficulty using your inhaler. Cleaning the inhaler: the inhaler must be cleaned at least once a week. 1. Remove the metal can from the plastic case and remove the mouthpiece cover. 2. Rinse the plastic case and mouthpiece cover thoroughly under running warm water. 3. Dry the plastic case and mouthpiece cover completely, both outside and inside. Avoid overheating. 4. Place the metal can into the plastic case and put on the mouthpiece cap. The metal canister should not be immersed in water. Symptoms: more frequent - hypokalemia, decreased blood pressure, tachycardia, muscle tremors, nausea, vomiting; less frequent - agitation, hyperglycemia, respiratory alkalosis, hypoxemia, headache; rare - hallucinations, convulsions, tachyarrhythmia, ventricular flutter, dilatation of peripheral vessels. Treatment: the best antidotes are cardioselective β-blockers. However, beta-adrenergic blockers should be used with caution in patients with a history of bronchospasm attacks. The use of large doses of salbutamol can cause hypokalemia, therefore, if an overdose is suspected, the level of potassium in the blood serum should be monitored. Hypersensitivity to any component of the drug; management of preterm birth; threatened abortion; children under 2 years of age. With caution: tachyarrhythmia, myocarditis, heart defects, aortic stenosis, ischemic heart disease, severe chronic heart failure, arterial hypertension, thyrotoxicosis, pheochromocytoma, decompensated diabetes mellitus, glaucoma, seizures, renal or hepatic failure, simultaneous use of non-selective beta-blockers, pregnancy, period lactation.
Possible product names
- Ventolin aeros. d/inhal. doses 100 mcg/dose 200 doses.
- VENTOLIN AEROSOL 100 MCG 200 DOSES
- VENTOLIN 100MCG/DOSE 200DOSE AEROSOL
- VENTOLIN AEROS. 0.1 MG/DOSE 200 DOSE X1
- VENTOLIN AIR. D/ING. DOSER. 100MCG/DOSE 200 DOSES No. 1 (02.09)
- NB.Ventolin Air. d/ing. 200doses M (R)
- (Ventolin) Ventolin aerosol. d/inhal. doses 100 mcg/dose 200 doses.
Instructions for use of Ventolin (Method and dosage)
The instructions for use of Ventolin warn that the medicine must be used correctly, regardless of the form of release, otherwise the treatment process may go wrong.
In addition, the drug must be taken only after consultation with a doctor.
The instructions for Ventolin for inhalation in the form of an aerosol indicate that to use the drug it is necessary to use a nebulizer with a mask and an endotracheal tube .
Ventolin Nebula, which is sold in the form of an inhaler solution, is used without dilution. The duration of inhalation is about 10 minutes. The medicine can be diluted with a sterile sodium chloride solution (0.9%). It must be used in well-ventilated rooms, as some of the drug enters the environment.
The instructions for Ventolin Nebula for inhalation recommend a dose of 2.5 mg. If necessary, it can be increased to a maximum of 5 mg. Frequency of use – 3-4 times a day. For adult patients, if necessary, in a hospital setting, the dosage is increased to 40 mg per day.
The inhalation aerosol is designed for approximately 200 uses. It can be used by adult patients and children over 2 years of age after being prescribed by a specialist. For long-term maintenance therapy, adults are usually prescribed 200 mcg up to 4 times a day. To prevent bronchospasms in childhood, 100-200 mcg (1-2 inhalations) is used.
The syrup is prescribed to adult patients, 2 ml 3-4 times a day. If necessary, the dosage can be increased to 4 ml.
Release form
Ventolin is available in the following forms:
- Tablets – 20, 50 and 100 pcs. in 1 package, 1 tab. contain 2 and 4 mg of salbutamol.
- Syrup 150 ml in a bottle - 2 mg in 1 ml.
- Double-layer tablets 0.008 g, 20 or 50 pcs. packaged.
- Ventolin for inhalation:
— Ventolin nebula (metered-dose aerosol in plastic ampoules) — 200 doses in 1 bottle. 2.5 ml per nebula. — Metered aerosol without freons (chlorofluorocarbons that destroy the ozone layer) — 200 doses in 1 bottle. 100 mcg of salbutamol in 1 dose.
- Syrup for internal use – 2 mg in 2 ml, in a 50 ml bottle.
Overdose
When using the drug in doses above the norm, hypokalemia , tachycardia , nausea, decreased blood pressure, muscle tremors , vomiting, agitation, respiratory alkalosis , headache , hyperglycemia , hypoxemia . In rare cases, hallucinations , tachyarrhythmia , dilatation of peripheral vessels, convulsions, and ventricular flutter .
Cardioselective beta-blockers are used for treatment , but with caution if there is a history of bronchospasm attacks.
Overdose of Ventolin™ nebula, symptoms and treatment
The most common signs and symptoms of Ventolin Nebula overdose are transient changes pharmacologically induced by β-adrenergic agonists (eg, tachycardia, tremor, headache). As a result of an overdose of salbutamol, severe hypokalemia may occur, so the level of potassium in the blood plasma should be checked. Treatment consists of discontinuing salbutamol and administering appropriate symptomatic therapy, such as cardioselective beta-blockers to treat patients with cardiac abnormalities (eg, tachycardia, palpitations). Drugs of the β-adrenergic blocker group should be prescribed with caution to patients with a history of bronchospasm.
Interaction
Ventolin for inhalation is not recommended for use in conjunction with non-selective beta-adrenergic blockers . In patients with thyrotoxicosis, this drug also increases the effect of nervous system stimulants and tachycardia .
If you combine an aerosol and an inhalation solution with xanthines tachyarrhythmia increases . The risk of severe ventricular arrhythmia with Levodopa and inhalational anesthetic . In combination with anticholinergic drugs, intraocular pressure may increase. When prescribed with diuretics and corticosteroids, the hypokalemic effect .
Reviews on forums
Marina, Moscow: “My son often has bronchitis, we are constantly prescribed Ventolin and Pulmicort. You need to breathe separately. The break should be 2 hours. Both drugs are diluted with saline in equal proportions. The child is 5 years old.”
Inna, Tver: “My daughter was prescribed Pulmicort and Ventolin at the same time for obstructive bronchitis. I immediately poured these medications into the nebulizer cup and added saline solution. Helps much faster. Separately, Pulmicort made the cough worse.”
Anastasia, St. Petersburg: “The pediatrician prescribed us medications separately, and the pulminologist prescribed them together. I don’t know which of them knows more. We were treated together. There were no side effects. These medications act differently, so I think it’s possible to breathe at one time.”
It is impossible to answer the question of which medication is better. Ventolin is a bronchodilator that eliminates spasms, coughing, and improves lung function. Pulmicort is a hormonal drug with pronounced antiallergic, anti-edematous, and anti-inflammatory properties. Additionally, it facilitates the removal of mucus from the respiratory system. Recovery occurs faster when they are used together as part of complex therapy. In some cases, inhalation with Pulmicort is done in the morning, Ventolin in the evening.
Analogs
Level 4 ATX code matches:
Onbrez Breezhaler
Formoterol Easyhaler
Fenoterol
Berotek
Foradil
Analogs of Ventolin, as well as Ventolin Nebula and Ventolin Easy Breathing in pharmacies can usually be obtained as follows:
- Ventilor;
- Nebutamol;
- Salamol Steri-Neb;
- Salamol-Eco;
- Salamol-Eco Easy Breathing;
- Salbutamol;
- Salbutamol-Inteli;
- Salbutamol-Neo.
They all have different prices. In many cases, analogues cost less than Ventolin itself.
Ventolin or Salbutamol - which is better?
Aerosol Salbutamol and Ventolin are synonyms, therefore, in all pharmacological properties they are equal, which means that one of them cannot be the best.
However, in practice, the patient very often develops his own preference. Due to a combination of factors (season, nutrition, absence of exacerbation of concomitant diseases), one of the analogues helps quickly. In this case, the positive connection is reinforced in the brain, creating the impression of benefits. For some, Ventolin is more effective, while others believe that, for example, only Salbutamol Teva works.
For children
Inhalations for children can be used to relieve bronchospasm attacks at a dosage of 100-200 mcg (1-2 inhalations). Maintenance therapy with Ventolin – up to 200 mcg 4 times a day (2 inhalations). For prevention, 100-200 mcg is used 10-50 minutes before the provoking factor (1-2 inhalations).
For children, Babyhaler or Volumatic spacers are used.
The clinical effectiveness of this drug in children under 18 months using a nebulizer has not been studied.
Indications for use
Ventolin is used for bronchospasm
Attacks of bronchospasm experienced by patients with bronchial asthma are the main indication for the use of Ventolin. The drug is often used in complex long-term therapy to support patients with bronchial asthma.
Ventolin is also used for other chronic pathologies that are characterized by reversible obstruction of the respiratory tract: emphysema, chronic bronchitis, etc.
Pediatricians often prescribe Ventolin inhalations for laryngitis and its complication – false croup. But here the opinions of doctors differ. Many experts believe that in this condition it is not advisable to use bronchodilators, since they are ineffective in case of inflammation of the larynx.
Parents often wonder whether Ventolin can be used for their child. Experts prescribe it to children from two years of age. Until this age, it is advisable to use Ventolin only when absolutely necessary and for a short course.
Ventolin price, where to buy
The price of Ventolin for inhalation in dosages of 100 mcg is about 150 rubles. In the form of a solution, this product is more expensive.
The price of Ventolin Nebula is on average 300 rubles. Ventolin Easy Breathing costs approximately 150 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
- Online pharmacies in KazakhstanKazakhstan
ZdravCity
- Ventolin aerosol for in.
dosage 100mcg/dose 200 dosesGlaxo Wellcome Production RUB 153 order
Pharmacy Dialogue
- Ventolin (aerial 100mcg 200doses)Glaxo-Wellcome
138 RUR order
- Ventolin Nebula solution for inhalation 2.5 mg/2.5 ml No. 20GlaxoSmithKline
RUB 262 order
show more
Pharmacy24
- Ventolin Evohaler 100 mcg 200 doses aerosol Glaxo Wellcome Production, France
72 UAH order
PaniPharmacy
- Ventolin liquid Ventolin Nebula d/ing solution. 2.5mg amp. 2.5ml No. 40 Germany, Aspen Bad Oldesloe
392 UAH. order
- Ventolin evohaler aerosol Ventolin evohaler aer. 100mcg/dose 200 doses Spain, Glaxo Wellcome
72 UAH order
show more
Ventolin during pregnancy
The drug is prescribed during pregnancy and breastfeeding in the most extreme cases. The medication should be used with caution, as hyperglycemia and/or tachycardia sometimes occurs in mother and child. No special studies have been conducted on the effect of the drug on the fetus, but doctors have recorded deviations in the embryonic development of the baby in mothers who used this medicine while carrying a child. Officially, Ventolin’s connection with these pathologies has not been established.
Contraindications
According to the instructions for use, Ventolin has a number of contraindications. The drug is not prescribed for the following conditions:
- threatened abortion;
- management of preterm birth;
- hypersensitivity to any of the components of the drug.
There are diseases for which the medicine should be used with caution. Relative contraindications include:
- diabetes;
- severe heart failure;
- ischemia;
- heart defects;
- thyrotoxicosis;
- myocarditis;
- tachyarrhythmia;
- arterial hypertension;
- glaucoma.