Pulmonary tuberculosis is an infectious lung disease that is transmitted by airborne droplets and is characterized by an inflammatory process.
The disease occurs due to the tuberculosis bacillus, it penetrates from the patient through coughing, sneezing, and dialogue. According to generally accepted data, there are about 2 billion infected people in the world. During the year, out of 100 thousand people who become ill with tuberculosis, approximately 18 people die.
Symptoms of tuberculosis are the first manifestations of a dangerous disease that a person can detect at home. Once symptoms are identified, treatment should be started immediately so as not to aggravate the clinical picture. In general, they can be different and depend on the type of development of the disease.
What it is?
In simple words, tuberculosis is an infectious disease of bacterial etiology.
The disease has not only a medical, but also a social aspect: the most sensitive to the causative agent of tuberculosis are people with a low level of immunity, an unbalanced diet, living in conditions of non-compliance with sanitary and hygienic standards, and poor social and living conditions. The development of the disease is influenced by the level of a person’s quality of life. However, the risk group for tuberculosis consists of all segments of the population, regardless of age and gender.
The high frequency of deaths (up to 3 million people per year) and the prevalence of the disease are due not only to social reasons, but also to the long period of latent course of the disease, when symptoms of tuberculosis do not appear. This time is the most favorable for therapy, and to determine the likelihood of infection, an assessment of the body’s reaction to the Mantoux test is used.
Heat
A reliable criterion for tuberculosis is a slightly elevated temperature that does not subside for a long time, which is not explained by any objective factors. In the evening, the fever can rise to 38 °C and be accompanied by chills. The patient experiences increased sweating, but with the help of this natural reaction the body still fails to reduce the temperature to the physiological norm. Febrile temperature (more than 39 °C) occurs in the last stages, in the presence of powerful sources of inflammation in the lungs.
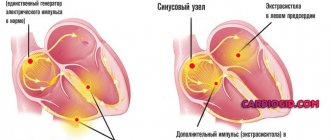
Pathogen
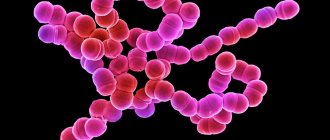
The causative agent of the pathology is the tuberculosis bacillus. A distinctive feature of the bacterium is its shell, which protects the microbe from changing environmental conditions and the effects of medications.
The tuberculosis bacillus develops very slowly, so diagnosing the disease can be difficult. Microorganisms are usually transmitted through the air: when a patient coughs, sneezes or talks. When drops containing components of the tuberculosis bacillus dry, even smaller particles are formed that remain in the air for a long time and do not settle down under gravity. From the air, the pathogen penetrates the mucous membranes of the human nasopharynx and into the respiratory tract.
The likelihood of infection depends on the duration of contact with the patient and the form of pathology from which he suffers. So, when communicating with a person suffering from pulmonary tuberculosis, the risk of contracting the disease increases many times over.
When bacteria enter the lungs, they do not always cause tuberculosis. The risk of developing pathology depends on the state of a person’s immune system, as well as on his individual sensitivity to a particular type of microorganism. The likelihood of infection is also influenced by a person’s age: the largest number of cases of the disease occur in the age group of 25–35 years.
Tuberculosis actively develops in people suffering from infectious and chronic pathologies:
- HIV;
- renal failure;
- diabetes mellitus;
- oncological diseases.
The risk category for tuberculosis infection includes children under 5 years of age, people living in poor living conditions, and the elderly.
Koch stick
Causes
The main reason is infection with Mycobacterium tuberculosis, which can occur in most cases by airborne droplets from a patient with an open form of tuberculosis. In this case, a huge amount of bacteria is released into the environment, and the danger for people nearby is increased.
However, infection is also possible in other ways:
- Contact – through the conjunctiva of the eye;
- Alimentary – through the digestive tract;
- Intrauterine – from mother to child (through the placenta or during childbirth).
Penetrating into the body, the mycobacterium is attacked by cells of the immune system and in most cases is successfully destroyed. However, the weak level of defenses cannot cope with the infection, and it invades the body. This explains the misconception that tuberculosis is a disease of the lower strata of society and underdeveloped countries.
- Unfavorable environmental and social living conditions;
- Presence of chronic somatic diseases;
- Presence of bad habits (smoking, alcoholism, drug addiction);
- Monotonous diet and lack of vitamins;
- Persistent psychological disorders (stress, depression, etc.).
The main cause of the development of the disease is considered to be the Koch microbacterium, which, after entering the human body, may not manifest itself for a long time. Activation of the bacterium occurs when the human immune system does not have enough resources to destroy the pathogen.
The peculiarity of an infectious disease is that if the immune system does not destroy it immediately, the pathogen lives for many years. The incubation period for a closed form lasts several years.
A patient with active secretion of mycobacteria and a severe cough can infect more than a dozen people over the course of a year.
Signs of tuberculosis appear equally often in people of different ages, both in newborns and elderly patients. The main sources of infection spread, as a rule, are sick people, as well as meat and milk from animals that are sick with tuberculosis. Tuberculosis is most often transmitted by airborne droplets.
The risk of getting sick depends significantly on the age of the infected person. Among those infected, the incidence of tuberculosis is highest in adolescence and young adulthood. In women, most cases of the disease occur between the ages of 25 and 34 years; at this age, women get sick more often than men.
Factors contributing to the development of the disease:
- Frequent visits to public places, transport, medical institutions,
- Decreased immunity
- ARVI,
- Emotional stress
- Avitaminosis,
- Cachexia,
- Overwork,
- Diabetes,
- Hereditary predisposition
- Long-term treatment with hormones, cytostatics and other immunosuppressants,
- Smoking.
- Tuberculosis is transmitted from person to person by airborne droplets, that is, you can become infected even without direct contact with the patient, but simply by being in the same room with him.
- In some cases, infection occurs through food and other objects that are contaminated with Koch bacilli.
- If tuberculosis pathogens enter the body with food, then tuberculosis in children and adults affects the gastrointestinal tract, and not the lungs, as happens when inhaling contaminated air.
Most often, only people with reduced immunity have a real risk of contracting tuberculosis.
- Young children.
- HIV-infected.
- People who are undernourished and experience frequent hypothermia.
- People living in damp, poorly heated and ventilated areas.
In addition, the risk of infection increases many times over with close and prolonged contact with patients with active forms of tuberculosis.
Risk factors
The people most often affected by tuberculosis are:
- have been in contact with an infected person for a long time;
- having chronic diseases of the respiratory system;
- those suffering from stomach or duodenal ulcers, diabetes mellitus;
- taking glucocorticoid medications for a long time (hormones strongly suppress the immune system);
- infected with the HIV virus;
- alcohol abusers, those in prison, those taking narcotic drugs;
- employees of medical institutions where patients with tuberculosis are treated;
- previously had non-pulmonary/pulmonary tuberculosis.
Psychosomatics of infection
Tuberculosis is one of the most dangerous diseases of humanity. Not very good statistics forced us to pay attention to the psychosomatics of this disease. Despite all kinds of examinations and preventive measures, the incidence rate decreased by only 5-10 percent. Psychologists and psychotherapists have come to the conclusion that negative emotions and constant stress provoke the development of tuberculosis. People do not want to perceive the realities of the world, they do not allow themselves to breathe deeply and enjoy life.
Forms and stages of the disease
Scientists have now identified many different forms of tuberculosis. This infection is primarily classified by the manifestation of its symptoms.
In this regard, there are two types of illness:
- Open form. In this case, a sick person releases a pathogenic bacterium into the environment, which can infect others. Most often this occurs when coughing or expectoration. This form is designated as BC+ or TB+. This mark indicates that infectious agents were detected in the sputum smear.
- Closed form. With this disease, pathogenic microbes can exist in the human body, but they do not enter the environment. This means that the patient is not contagious. In this case, the marking is BK- or TB-.
There are also such forms of the disease as primary and secondary. They are set depending on whether the person is experiencing the disease for the first time or has had a relapse.
In addition, it is worth noting that there are dozens of types of tuberculosis diseases that can be caused by the bacterium Mycobacterium tuberculosis complex. Among them, it is necessary to highlight disseminated pulmonary tuberculosis, miliary pulmonary tuberculosis, focal pulmonary tuberculosis, infiltrative pulmonary tuberculosis, caseous pneumonia, pulmonary tuberculoma, cavernous pulmonary tuberculosis, fibrous-cavernous pulmonary tuberculosis, cirrhotic pulmonary tuberculosis and tuberculous pleurisy. All these diseases have certain characteristics, diagnostic methods, and treatment methods.
Other examination methods in the hospital
Testing for tuberculosis also includes other measures, including:
- fluoroscopy;
- radiography;
- tomography;
- fluorography.
Fluoroscopy is an inexpensive examination method that is used most often than others. It can also be called primary, since usually the first signs of the disease are detected during routine fluoroscopic examinations. Using special equipment, a specialist takes a photo. If there is a pathology, it immediately becomes noticeable in the image. Usually this is a projection of a dark-colored lesion against the background of a lighter lung. It is recommended to conduct such a study at least once a year. This is necessary for everyone, even if the epidemiological situation is satisfactory.
This type of research is prescribed to clarify the general condition and nature of the current process. A doctor may prescribe tomography if it is necessary to localize lesions, study the nature of deep decay, determine the boundaries of the lesion, and the total volume of the affected area.
Fluorography is prescribed for mass testing during medical examinations. This method is used as a warning; it allows you to identify any latent lung diseases, not only tuberculosis, but also various inflammatory processes and tumors. It is during medical examinations that the first conclusions about the suspected presence of tuberculosis are usually made, and the doctor prescribes more detailed studies.
https://youtube.com/watch?v=gi4WvmVw1o4
Testing for tuberculosis is very important. It is with the help of numerous methods, including such simple ones as fluorography, that one can identify the first signs of this formidable disease and determine the complexity of its course. The doctor can prescribe treatment only based on the results of the examination, otherwise the measures used may not be effective.
The first symptoms of tuberculosis
Pulmonary tuberculosis can occur for a long time without visible symptoms and be discovered accidentally during fluorography or on a chest x-ray. The fact of contamination of the body with tuberculous mycobacteria and the formation of specific immunological hyperreactivity can also be detected by performing tuberculin tests.
In the initial stage of tuberculosis development, the symptoms are quite difficult to differentiate from ordinary acute respiratory infections or chronic fatigue syndrome. But if we consider the first signs of tuberculosis in adults in more detail, it will be possible to identify them in advance.
In cases where tuberculosis manifests itself clinically, usually the very first symptoms are nonspecific manifestations of intoxication: weakness, pallor, increased fatigue, lethargy, apathy, low-grade fever (about 37 ° C, rarely above 38 °), sweating, especially disturbing the patient at night, weight loss Often generalized or limited to any group of lymph nodes, lymphadenopathy is detected - an increase in the size of the lymph nodes. Sometimes it is possible to identify a specific lesion of the lymph nodes - “cold” inflammation.
1) Increased body temperature
The most important first sign of tuberculosis is considered to be elevated body temperature, which does not return to normal within a month. Moreover, its appearance cannot be explained by any objective reasons - there are no inflammatory processes occurring in the body, there are no signs of a cold or flu. In the morning, the body temperature of a patient with tuberculosis is within the normal range, but in the evening it invariably rises to 38.5 degrees and is always accompanied by chills.
Please note: in the initial stages of tuberculosis development, body temperature never reaches febrile levels (39 degrees and above), but this is typical for the later stages of the disease.
2) Cough
A patient with tuberculosis coughs constantly, but at the very beginning of the disease the cough will be dry and paroxysmal, from the outside it looks like a nervous reaction. As the pathology progresses, the cough becomes wet; after coughing up sputum, the patient experiences relief for a short time.
Please note: if a person has had a dry cough for 20 days or more, and there are no other symptoms of cold/bronchitis, then this is a reason to immediately contact a phthisiatrician to clarify the diagnosis.
3) Shortness of breath and wheezing
Shortness of breath appears at the slightest physical exertion, a person behaves like a fish out of water - he is catastrophically short of air.
Wheezing of various types occurs. They can be dry or wet, it all depends on the damage to the lung tissue and the individual characteristics of the patient. Only a doctor can determine this diagnosis based on listening and additional symptoms.
4) Change in the patient’s appearance
The disease in question makes the patient’s face haggard, his skin acquires a pale tint, but on the cheeks, on the contrary, an unnatural blush “burns.” A patient with tuberculosis is rapidly losing weight, despite the fact that his appetite remains normal and his diet has not undergone any adjustments.
At the very beginning of the development of tuberculosis, changes in appearance are not very noticeable, and as the pathology progresses, a diagnosis can presumably be made based on the patient’s appearance.
5) Chest pain
This symptom is more typical for the later stages of tuberculosis, when it has already taken a chronic form. But at the beginning of the development of the disease, mild pain may be present only during moments of deep inspiration, and the pain will be localized under the ribs.
Physical examination
During an external examination of a person with an early stage of tuberculosis, any pathological defects are often not detected at all.
However, after contact with a patient, it is extremely necessary for an adult to be tested for tuberculosis, since it is impossible to detect the disease at home. A physical examination carried out in a clinic or at home can determine even at an early stage that adults have developed pulmonary tuberculosis. Therefore, the medical examination is carried out very carefully. The doctor evaluates the anatomical development of the patient’s body, the color of the skin and the condition of the mucous membranes. It checks whether the right and left sides of the chest are symmetrical. If tuberculosis is suspected, the fingers of the upper and lower extremities are also examined. A symptom of the disease is a change in the shape of the terminal phalanges, which resemble drumsticks. Another sign is deformation of the shape of the nails, which look like watch glasses.
"Drumsticks"
Timely early detection of pulmonary tuberculosis in adults is carried out using palpation. Doctors determine the level of moisture in the skin, its elasticity, and the presence of a layer of subcutaneous fat. In people with chronic tuberculosis, a decrease in the volume of the muscles of the shoulder and chest is determined.
Another method of physical examination for tuberculosis is auscultation of the lungs. It should be remembered that tuberculosis sometimes does not lead to changes in the characteristics of the respiratory function and is not manifested by the appearance of additional noise in the lungs.
Using percussion, rather severe lesions of lung tissue are diagnosed in infiltrative or cirrhotic forms of tuberculosis
Percussion is important for determining conditions requiring emergency care: spontaneous accumulation of air in the pleural cavity, acute exudative inflammation of the pleural layers, collapse of the lung lobe
The presence of a boxed or shortened lung sound makes it possible to find out that the airiness of the lung tissue is changed and, possibly, symptoms of tuberculosis are present. This is indispensable for quickly assessing the clinical picture of the disease and promptly performing the required examinations.
Symptoms of extrapulmonary forms of tuberculosis
Koch's bacillus can affect not only lung tissue, but also multiply and cause inflammatory processes in other organs. With such localization they speak of an extrapulmonary type of disease. A nonspecific type of tuberculosis damage to internal organs and systems is diagnosed, as a rule, by excluding other diseases and pathologies.
The clinical picture depends on the severity of the process and the location of the organ or tissue affected by the bacterium.
- Tuberculous damage to the organs of the digestive system is expressed in periodic defecation disorders, a feeling of bloating, pain in the intestinal area, signs of hemorrhagic bleeding (blood in the stool), and an increase in body temperature up to 40°C.
- When the inflammatory process is localized in the brain, the disease manifests itself in an increase in body temperature, disturbances in the functioning of the nervous system, sleep patterns, increased irritability, neurotic reactions, and enlargement of the neck and neck muscles. Characterized by pain in the back when straightening the legs, tilting the head towards the chest. The disease progresses slowly, and those at risk include preschool children, patients with diabetes, and HIV-infected people.
- Damage to the genitourinary system by tuberculosis bacteria is usually detected in the kidneys and/or pelvic organs. The clinical picture consists of painful attacks in the lower back, body hyperthermia, frequent, painful, unproductive urge to urinate, and the inclusion of blood in the urine.
- Tuberculosis damage to bone and joint tissue is manifested by pain in the affected areas and limited joint mobility. Due to the similarity of symptoms with other diseases of the musculoskeletal system, it is difficult to diagnose.
- Tuberculous lesions of the skin are expressed in the form of rashes widespread throughout the skin, merging and forming nodular formations that are dense to the touch.
Other symptoms are possible when various organs are affected. A pathogenic organism, penetrating the bloodstream, can spread throughout the body and target almost any organ, tissue or system. In this case, clinical signs of the disease are difficult to differentiate from similar inflammatory processes of a different etiology. The prognosis for treatment of extrapulmonary forms depends on the time of diagnosis, the localization of the pathological process, its stage, the degree of organ damage, and the general health of the patient.
Clinical manifestations
From the moment the infection enters the body and the disease develops, a certain period passes, it is called incubation. It can last from three to twelve months. At this time, the pathogen spreads throughout the body in the blood, but the immune system actively fights it.
This period is characterized by an asymptomatic course. Such a patient cannot yet infect another person. Diagnostics can also be negative.
To do this, you need to know what the main signs of pathology are.
The first symptoms appear only after all the resources of the immune system to fight the disease have been exhausted.
The first sign is a long period of increased body temperature to subfebrile levels. It can last three weeks or more.
The second most important symptom that may indicate the presence of a tuberculosis infection in the body is a cough, which also lasts for at least three weeks. At first it is dry, but over time it becomes moist and phlegm appears. In advanced cases - with an admixture of blood.
The most common complaint reported by patients is drenching night sweats. Pulmonary tuberculosis can be confused with the onset of ARVI, as it is characterized by the following symptoms:
- weakness;
- chills;
- dizziness;
- weight loss;
- pale skin;
- nausea;
- chest pain;
- dyspnea.
As for damage to other organs, the symptoms here are even more severe. With tuberculosis of the genital tract, women may experience intermenstrual bleeding, pain in the lower abdomen, deformation of the tubes, and in men - swelling of the scrotum.
Bone tuberculosis may go undetected for years, as its manifestations are similar to other forms of arthritis, such as rheumatoid arthritis. Other types (tuberculosis of the nervous system, gastrointestinal tract) are even less common, mainly in HIV-infected people.
The most dangerous manifestation is when the pathogen spreads throughout the body, many microgranulomas occur. If you take an X-ray of such a patient, he will look as if he was sprinkled with millet.
Diagnostics
Diagnosis of tuberculosis is based on fluorography, radiography and computed tomography of affected organs and systems, microbiological examination of various biological materials, tuberculin skin test (Mantoux reaction), as well as the method of molecular genetic analysis (polymerase chain reaction), etc.
Also, the diagnosis of active tuberculosis is carried out by microscopic examination of sputum obtained by smear. Such diagnostics is one of the most popular methods, but it is far from the most unambiguous, since in the early stages of tuberculosis, as well as in its manifestations in children, such a study will give a negative result. It is more effective to use fluoroscopy or fluorography, which will give higher accuracy in the results, especially in the later stages.
Polymerase chain reaction is also used to identify the pathogen.
Ultrasound examination
Ultrasound examination of the pleura is not yet used so often, although it can show not only foci of tuberculosis, but also malignant formations. All the diagnostic capabilities of this particular method are not very common today. Experts prefer proven diagnostic methods that have proven themselves to be excellent.
Ultrasound allows you to visualize the surface of the visceral layer of the pleura, tissues of the chest and lungs, the diaphragm, and subpleural sections. Ultrasound allows you to obtain valuable information regarding the condition of the pleura, the presence of fluid, and the identification of all lesions. On the resulting image you can see whether there are breaks in the tissue structure, what the size of the lesions is.
The use of ultrasound examination allows you to expand diagnostic capabilities and obtain more accurate data on the course of the process. But not all areas can be thoroughly examined using this method. For example, ultrasound is not used in the area of the shoulder blades.
The ultrasound method makes it possible to obtain the following data:
- visualization of affected areas;
- assessing how the process is spreading;
- assessing whether the process is spreading to other areas;
- conducting diagnostics for changes in pleural tissue;
- determining the amount of fluid that is in the pleura;
- assessing all nearby tissues.
Complications
The worst complication may be death from tuberculosis. This is the case if it is not treated. There are also other consequences of the disease:
- destruction of other organs occurs, for example, liver, heart, kidneys, etc.;
- the disease can destroy joints, leading to bone tuberculosis;
- pulmonary hemorrhage may occur - one of the most dangerous complications of tuberculosis. In this case, urgent medical attention is needed.
If a person has once suffered from tuberculosis, then he is not immune from inflammation of the disease in the future. There is also no certainty that the child will not become infected from the mother and will be born completely healthy and without abnormalities. Often there is a frozen pregnancy or death of the baby during childbirth.
After recovery, a person may still experience headaches, discomfort in bones and joints, and weakness for some time. Most often this happens due to strong medications. There may also be a disturbance in the functioning of the stomach and upset stool.
Hemoptysis
This serious sign almost certainly indicates infiltrative tuberculosis. You just need to differentiate this illness from heart disease or lung cancer, since they are also characterized by hemoptysis. In tuberculosis, blood is released from the respiratory tract in a small amount immediately after an attack of wet cough with copious sputum. In some cases, blood literally flows like a fountain, which indicates a rupture of the cavity. The patient requires emergency assistance.
What to do if you have tuberculosis at home
All members of the family in which there is a patient with tuberculosis must take precautions. The infected person should be isolated in a separate room or behind a screen. The number of things he will come into contact with should be limited as much as possible. All items in the house should be disinfected and cleaned daily.
Soft toys, carpeting, curtains, and extra pillows must be removed from the room in which the patient lives. It is recommended to cover upholstered furniture with special covers, which need to be boiled from time to time. When moving around the house, the infected person must wear a mask (disposable or four-layer gauze).
Sputum examination
Doctors can tell you how to diagnose tuberculosis without Mantoux. In this case, collection and further examination of sputum for the presence of Koch's bacillus is a mandatory diagnostic procedure. To ensure that the result is not distorted, it is necessary to follow the sequence of microbiology:
- All patients receive 2 fluid samples.
- To collect sputum, disposable plastic containers with a volume of at least 50 ml must be used.
- The first portion of the secretion must be collected and donated during the initial visit to the clinic on the day of treatment. The second one is collected independently the next morning.
It is important to follow the recommendations of specialists in order to make the correct fence:
- Biological fluid should be collected in the morning before meals. At night, more sputum is formed, which facilitates the process and increases the information content of the diagnostic test.
- To prevent bacteria and microorganisms from entering the liquid, it is necessary to brush your teeth before the procedure.
- Before collecting the material, you should not take antitussive medications - as a result of their influence, the outflow of mucus may be obstructed. If it is difficult to clear sputum, your doctor may prescribe mucolytics.
Microbiological diagnostics are carried out in the following ways:
- Ziehl-Neelsen microscopy;
- luminescent method;
- PCR;
- bacteriological culture.
Laboratory diagnosis of tuberculosis can detect Koch's bacillus in sputum. If bacteria are detected in at least 1 of the samples, the test result is considered positive.
How to treat tuberculosis?
Typically, treatment for tuberculosis is complex and lengthy; depending on the type and severity of the disease, it lasts up to two years and includes the following measures:
- Chemotherapy;
- Maintenance drug therapy;
- Surgical interventions (if necessary);
- Rehabilitation in sanatorium-resort institutions.
Hospitalization for tuberculosis
It is not always necessary to go to the hospital to treat tuberculosis. There are indications for hospitalization:
- Suspicion of pulmonary tuberculosis.
- Carrying out differential diagnosis of tuberculosis with other diseases that have similar symptoms.
- Treatment of newly diagnosed extrapulmonary tuberculosis (course of chemotherapy).
- Treatment of tuberculosis resistant to anti-tuberculosis drugs.
- Treatment of active forms of the disease.
- Treatment of common forms of tuberculosis.
- The need for surgical treatment of tuberculosis.
The duration of hospitalization for tuberculosis depends on the form of the disease:
- If the diagnosis confirms that the patient does not have tuberculosis, he is discharged immediately.
- If the preliminary diagnosis is confirmed, treatment takes about 3-4 months. Only after three sputum tests confirming that the patient does not secrete mycobacteria can he undergo further treatment on an outpatient or sanatorium basis.
- With multidrug-resistant tuberculosis, when the bacillus is resistant to all anti-tuberculosis drugs, the patient can spend up to one and a half years in the hospital.
Asymptomatic period
Of particular concern to phthisiatricians is the increasing number of cases of asymptomatic tuberculosis, when the pathological process is detected accidentally during fluorography or the Mantoux test. Very often, in the initial phase of the disease, there is no suspicion that a person is infected and is a spreader of the formidable infection caused by Koch's bacillus.
Often, during the infection stage, the clinical symptoms of the “tube” are completely absent or have mild severity. The absence of disease-specific syndromes can provoke an incorrect diagnosis when an entry about ARVI or pneumonia is made in the patient’s medical history.
Therefore, at the first signs of ill health, you should visit a general practitioner, since it is impossible to understand that you have tuberculosis at home.
Over time, prolonged coughing attacks occur, regular coughing, a rise in temperature to subfebrile levels, rapid fatigue, overwhelming weakness, malaise, excessive sweating, shortness of breath, causeless weight loss, poor appetite. These phenomena should alert a person and motivate him to quickly consult a doctor to compare the manifestations of the disease with the clinical symptoms indicated in the official description.
Chemotherapy
In modern phthisiatric practice, anti-tuberculosis therapy is used with the participation of several types of antibiotics.
There are currently three treatment regimens available:
- Three-component;
- Quadruple;
- Five-component.
Treatment of tuberculosis consists of two main phases:
- Intense;
- Prolonged.
The goal of the first, intensive phase is to stop the inflammatory process, prevent further tissue destruction, resorption of infiltrate and exudate, and stop the removal of tuberculous mycobacteria from the body into the environment. That is, doctors are trying to make a person stop being contagious. This takes, on average, two to six months.
Prolonged treatment of tuberculosis is aimed at complete healing of foci of inflammation, scarring of damaged tissue and restoration of strong immunity in the patient. Depending on the nature and severity of the disease, therapy can last up to two years, and in the case of multidrug-resistant tuberculosis - up to three to four years, until X-ray examination proves complete attenuation of the disease.
Surgery
So, we found out why tuberculosis appears. Diagnosing the disease in advanced cases requires surgical treatment. It involves several types of surgical intervention:
- Artificial pneumothorax or pneumoperitoneum - squeezing and securing the lung through the introduction of purified oxygen into the pleural cavity. The method is called collapse therapy. If the organ is fixed, the cavities in it grow together over time; in addition, the release of the tuberculosis pathogen stops, and the patient stops infecting people.
- Speleotomy or cavernectomy is the removal of particularly large cavities that cannot be treated conservatively.
- Valvular bronchoblocking is the installation of small valves at the mouth of the bronchi to avoid their gluing and normalize the breathing of infected people.
- Resection is the removal of an irreversibly damaged lobe of the lung.
- Lobectomy - removal of one part of an organ.
- Bilobectomy – removal of one part of both organs.
- Removal of one lobe of an organ completely – pneumonectomy, pneumonectomy.
Some traditional medicine recipes will also help in treating the described illness.
Additional drugs for treatment
Additional therapy for tuberculosis includes:
- Immunostimulants (galavit, xymedon, glutoxim) help the body fight mycobacterium tuberculosis;
- Hepatoprotectors are necessary to protect the liver from the destructive effects of antibiotics; they are prescribed with constant monitoring of the level of bilirubin in the blood;
- Sorbents (acetylcysteine and rheosorbilact) are prescribed during chemotherapy withdrawal in case of extremely severe side effects. After a short period of rest, treatment still has to be resumed;
- B vitamins, glutamic acid and ATP are needed to prevent peripheral neuropathy and other undesirable effects from the central nervous system;
- Methyluracil, aloe vera, glunate, FiBS are prescribed during the treatment of tuberculosis to accelerate the processes of cellular regeneration;
- Glucocorticoids are a last resort because they have a strong immunosuppressive effect. But sometimes they are still prescribed for a short period of time in order to suppress the too violent manifestations of the inflammatory process in extensive and severe tuberculosis.
Healing jam
Such a healing composition will undoubtedly help in treating the first signs and symptoms of tuberculosis. Take a liter of unsalted rendered lard, honey and agave juice. Add to this mixture a spoonful of beeswax and pure rosin, which can be purchased at the pharmacy. Add 1.5 packs of cocoa, 250 ml of vodka and sublimate to the edge of the knife.
Preparation:
- Place the pork fat, honey and beeswax on gas in one pan.
- As soon as everything dissolves, pour in the agave.
- Boil and gradually add everything else.
- Vodka at the end.
- When everything is mixed, cover with a lid and place in the oven for an hour. The end result will be jam.
You need to take a tablespoon 3-5 times a day; you can spread it on bread and eat it with tea. This jam cleanses the lungs well, and improvement will occur after the first day of use. Also, such a remedy would be appropriate if wheezing appeared after starting treatment for tuberculosis. After all, all its components quickly fight the disease, and the cough will gradually begin to recede.
Diet
Nutrition for tuberculosis should be aimed at strengthening the immune system.
- The patient should consume from 120 to 150 g of pure protein per day. It is needed for the production of antibodies. Sources of protein: fish, seafood, dairy products, lean poultry and fish, liver of cattle and fish.
- The amount of fat the patient needs is from 50 to 80 g per day. They are necessary to restore cell membranes that have been damaged by mycobacteria. To avoid a shortage of fats, you need to eat butter and vegetable oils, fish oil, lard, and animal fats in small quantities.
- Carbohydrates for tuberculosis should correspond to the age norm - about 400 g per day. They can be obtained from cereals and vegetables. Eating more than 80 g of confectionery products per day is not recommended.
- Mineral salts normalize metabolism and improve the functioning of the endocrine system, thereby increasing the body's defenses. Their sources can be: tomatoes, figs, cauliflower, herbs, cheeses, cottage cheese.
Cough
A person suffering from pulmonary tuberculosis coughs almost regularly, but at the beginning of the disease the cough is dry, paroxysmal and similar to a nervous reaction. And then, if the granulomas grow into caverns and exudate accumulates in the lungs, intense sputum production occurs. The cough becomes wet, and after clearing the throat the person feels relief for some time. It is impossible to say exactly when a cough appears during tuberculosis, since everything depends on the human body and its immune system.
Prevention
Due to the fact that infection occurs quite easily, doctors have drawn up certain rules to prevent the pathogen from entering the human body. They are as follows:
- You should not stay in the same room for a long time with a person suffering from tuberculosis.
- It is worth getting vaccinated periodically at the prescribed time in the form of BCG. First of all, this concerns children. The vaccine is also given to adults under 30 years of age if their Mantoux test gives a positive result.
- It is necessary to do fluorography once a year. This applies to both children and adults.
In order to detect tuberculosis in the early stages, all adults must undergo a fluorographic examination in a clinic at least once a year (depending on profession, health status and membership in various “risk groups”). Also, if there is a sharp change in the Mantoux reaction compared to the previous one (the so-called “turn”), the phthisiatrician may suggest preventive chemotherapy with several drugs, usually in combination with hepatoprotectors and B vitamins.
Some adults and approximately 10% of children who do not receive preventive treatment during the transition period develop a condition called tuberculosis intoxication.
Sowing
This test involves collecting sputum from the oral cavity to identify tuberculosis pathogens in it. This technique is considered one of the most accurate and effective. The main problem with this technique is that it takes a long time to get results.
The thing is that individual microorganisms take a long time to grow – up to 3 months. In view of this feature, samples for analysis are kept in a sterile thermostat for the entire duration of the study.
Preparing for analysis
To obtain accurate data, you need to follow some recommendations when collecting material:
- Sputum collection is collected in a sterile container. It can be taken from the laboratory.
- Before collecting the material, it is necessary to thoroughly clean the oral cavity.
- Expectoration is best done in the morning on an empty stomach. This period is considered the most favorable for collecting material, since at this time the maximum amount of sputum is released.
- The analysis must be delivered to the laboratory no later than a couple of hours after collecting the material.
If the collection is carried out correctly, the sputum will be mucopurulent or mucous in nature. The volume of material for research should be about 5 ml.
Carrying out analysis
When biomaterial enters the laboratory, it is initially checked visually. If the disease is severe, blood will be present in the sputum. But this is not yet an indicator for making a diagnosis of tuberculosis. Blood in the sputum may be present in both lobar pneumonia and a tumor in the respiratory system.
If the patient has tuberculosis, pathogenic microorganisms will be found in the sputum.
You can analyze sputum using two methods:
- Bacterioscopic. This method has been used for more than a decade. Thanks to it, it is possible to identify red blood cells, lung tissue fibers, Kurshman spirilla and other substances. In the sputum of an infected patient, in addition to pathogenic microflora, dark fragments are also observed - small particles of disintegrating foci.
- Biological. This method involves the use of the following procedures: settling the mixture, shaking, removing the protein, and only after that the contents of the tube are taken for inoculation.
Decoding the results
After the sample is stained, it is examined under a microscope and the number of bacteria is counted. If in the field of view their number does not exceed the number 3, then the disease is considered unconfirmed, and the result is written on the form - not detected.
If 4-9 bacteria are found in the laboratory technician’s field of view, then the result is not positive enough.
But further, if there are 10 or more organisms in the field of view, then the laboratory assistant sets the indicator +1. If there are more than 2 dozen of them, then +2, but if their number already significantly exceeds 30, then this is already a contagious form.
Forecast for life
With early detection of Koch's bacillus in the body, careful diagnosis and strict compliance by the patient with the instructions of the attending physician, the prognosis for recovery from tuberculosis is very positive.
The unfavorable outcome of the disease in most cases is due to the advanced form of the disease, as well as the frivolous attitude of patients towards it.
However, remember, even if doctors gave up on a patient, there is a lot of evidence when such a person turned to God in prayer and received a complete recovery, even with such deadly diseases as cancer.
Pneumonia: symptoms in adults, treatment and prevention Bronchitis in adults: how to treat, what symptoms, list of antibiotics Serous meningitis - symptoms and treatment Cardiac asthma - symptoms and treatment in adults
Signs
At the initial stage, tuberculosis is very difficult to distinguish from a common disease or fatigue syndrome. At the same time, it is difficult to accurately answer the question of how long it will take for the first signs of tuberculosis to appear, since it depends on many of the factors already listed above. A person regularly feels weak and drowsy. He doesn’t feel like eating, his mental state is depressed, and the slightest stress causes a strong emotional reaction.
In the evenings, the infected person feels a slight chill, his night sleep is usually restless, accompanied by sweating. The body temperature stubbornly remains at the subfebrile level - 37.1-37.2 ° C, and a dry paroxysmal cough occurs, which is especially annoying at night and in the morning.
It is important to know how long it takes for tuberculosis symptoms to appear. The first of them can occur after the incubation period, which is particularly long for this disease. It can last up to 3 years, and the infected person will not even suspect the presence of Koch’s bacillus in his blood.
Diaskintest
Modern method for detecting Koch's bacillus. It is a skin allergy test on a par with Mantoux, but more specific. The dose of the administered substance contains antigens of virulent tuberculosis bacilli, due to which this diagnostic test is used to assess the activity of the disease.
It should be noted that Diaskintest cannot be used instead of the Mantoux test, since its main feature is that it detects only dangerous strains of mycobacteria.
It is recommended that an alternative detection method be used if the child or adult has recently received a vaccine. In most cases, the Mantoux test may show a false positive result, but the substance administered during Diaskintest will not react to vaccination.