Bronchial asthma is a special condition of a child’s bronchi when they are ready to react with a spasm to the ingress of a certain allergen or various types of them. Most often, the pathology is genetically determined, so it can manifest itself at different ages, even in children under one year old, but is most often registered at 2-5 years.
Bronchial asthma in children occurs with alternating periods of exacerbation and remission, and the duration of each of them will differ depending on individual characteristics, living conditions and medications taken. It cannot be infected from another person. If a child begins to cough or has wheezing after contact with a person who had similar symptoms, this indicates bronchial obstruction, which arose as a result of a collision of the bronchial wall with the virus.
The diagnosis is made after some instrumental and laboratory tests. Once established, it does not make the child disabled, but in order to maintain an adequate quality of life, it requires the imposition of many restrictions on the type of diet, region of residence, physical activity, taking medications, or the ability to acquire pets.
Unfortunately, at this stage, bronchial asthma cannot be done. With the help of drugs and regimen, it is only possible to maintain remission of the disease for a long time.
A little about the bronchi
Bronchi are cartilaginous tubes that are a continuation of the trachea. The main bronchi depart from the latter at the level of 5-6 thoracic vertebrae in the amount of 2 pieces - right and left. Then they branch into lobes, of which there are two on the right (since there are only 2 lobes in the right lung), and three on the left. Each of the lobes is divided into segmental lobes that conduct air to segments (pieces), and those, in turn, are divided into subsegmental, then interlobular and intralobular. The final stage is considered to be the respiratory bronchioles - tubes that go directly to those structures where oxygen is obtained from the air and carried directly into the blood.
The wall of the bronchi consists of three membranes:
- Internal, mucous. Underneath it is a loose submucosal layer, which contains nerve endings, lymphatic tissue, a network of lymphatic capillaries, and the terminal sections of the glands that produce bronchial mucus (if these glands die, the mucous membrane dries out and becomes inflamed).
- Medium, consisting of three types of tissue: fibrous, cartilaginous and muscle. The smaller the caliber of the bronchus, the less cartilage tissue it contains, and vice versa, the larger it is, the denser the cartilage. With a decrease in the diameter of the bronchi, the thickness of the obliquely circular muscle fibers increases.
- Adventitia, outer shell. It consists of loose connective tissue.
The mucous membrane contains many different cells. This:
| Type of cells | Function |
| Goblet | They produce mucus, which traps dust particles and microbes that enter the bronchi with air. This dust is removed with the help of ciliated cells. The distribution of goblet cells is uneven: in some areas the ratio of ciliated to goblet cells ranges from 4:1 to 7:1, while in others it is 1:1. With distance from the main bronchi, these cells become less and less |
| Ciliated | They remove mucus, which contains dust and neutralized microbial particles |
| Intermediate | These cells are elongated and are found between different types of cells |
| Basal | From them goblet and ciliated cells of the mucous membrane are formed: |
| Cells Clara | They produce enzymes that break down surfactant, that is, a substance that prevents the alveoli from collapsing. At the same time, they produce part of the surfactant. In the bronchioles they replace goblet cells |
| M cells | They capture microbial cells and report them to immune cells so that they can produce specific antibodies directed only against these microbes |
| Kulchitsky cells | Produce hormone-like substances that affect the lumen of the bronchi |
| Immune cells: plasma cells, mast cells, leukocytes and eosinophils | Normally there are few of them. They form an immunological defense against antigens and microbes entering the air |
When a child is born, the main part of his bronchial tree is already formed, but it continues to branch. The size of the bronchi develops intensively in the first year and during puberty.
In the first year, ciliated and other cells of the mucous membrane are just developing, so there is little protective mucus in the bronchi, and it is not excreted well enough. This causes easier infection of the lower respiratory tract.
The bronchial cartilage in children under one year of age is softer and more elastic, which allows them to move. The bronchial muscles are also underdeveloped, as a result the cough reflex does not work well, and small bronchi are more easily clogged with mucus when inflamed.
Danger of allergens
Substances that provoke asthma attacks are not only unpleasant, but also dangerous.
This depends on a number of reasons:
- Diversity. There are a huge number of allergens. And their number is constantly growing.
- Sudden appearance. Allergies can occur during the period of illness, when a weakened immune system is unable to fight the provocateur.
- It is impossible to reduce the body's sensitivity. This is because reacting to stimuli is a natural process.
This is why it is possible to say with certainty whether asthma is completely curable. Unfortunately, complete recovery from the disease is impossible.
Therapy comes down to combating symptoms. This process will be facilitated by eliminating allergens such as smoke, dust, and fur from the asthmatic’s environment. Buy air purifiers and humidifiers. In addition, it is necessary to ventilate the room in which the patient is located daily.
What happens with asthma
In asthma, inflammation of the bronchial wall develops: in its submucosal layer the number of immune cells increases. Basically, these are cells whose number increases during allergies: eosinophils, basophils, mast cells, T-lymphocytes. When allergens enter, they release a large amount of biologically active substances. This leads to swelling of the mucous membrane and the production of large amounts of mucus by its glands. The result is difficulty breathing, coughing, wheezing, heard when exhaling.
Substances released by eosinophils and mast cells, as well as substances synthesized by other immune cells in response to their release, trigger reactions of chronic inflammation of the bronchial wall, which leads to the appearance of scar tissue under the mucosa. Because of this, the bronchi become hyperreactive, that is, they subsequently immediately spasm in response to allergens.
Symptoms of bronchial asthma
In children, allergic and mixed forms of the disease are more often observed. At first, symptoms may be vague and resemble a cold. However, later the clinical picture becomes more characteristic. The disease manifests itself:
- paroxysmal unproductive cough (at the end of the attack a small amount of mucus is coughed up);
- whistling sounds during inhalation and exhalation;
- shortness of breath (mainly difficult to exhale);
- a feeling of chest compression.
Children with bronchial asthma have a cough with wheezing for a long time. The symptom intensifies during active games, stressful situations (during crying, fear), at night. Seizures occur soon after the baby goes to bed. After coughing, there is a feeling of lack of air. Breathing becomes more frequent, wheezing appears, chest movements become more noticeable, and it is difficult for the patient to exhale, because it is necessary to suppress strong resistance from the narrowed bronchi. After the attacks, the child is lethargic, apathetic, and drowsy.
Classification of the disease
The following forms of bronchial asthma are distinguished:
- Mostly allergic (atopic). It can take the form of:
- bronchitis (that is, with cough and sputum production);
- a combination of both asthmatic symptoms and a runny nose with the release of copious amounts of light snot;
- combinations of asthma symptoms with sneezing, nasal congestion, and discharge of light snot;
- exogenous asthma: when symptoms appear in response to contact with allergens (animal hair, plant pollen, food, household chemicals and decorative cosmetics).
- Non-allergic asthma. It occurs upon contact with protein-free substances that cannot be allergens. These are substances produced by industrial production, drugs. Non-allergic forms of asthma also occur in response to neuropsychic overload, endocrine diseases, physical activity, and exposure to any microorganism.
- Mixed asthma, when characteristic symptoms can occur in response to both some external allergen and an infectious, endocrine or neuropsychic disease.
Asthma can affect a child of any age, but it is most often found in children 2-5 years old.
Prevention of bronchial asthma
Preventive measures are relevant for children prone to allergies, as well as whose close relatives suffer from asthma. Such activities must be carried out from birth. To prevent bronchial asthma you should:
- feed the newborn with breast milk for as long as possible;
- introduce complementary foods correctly;
- avoid foods that may cause allergies (honey, chocolate, nuts);
- treat colds and infectious diseases in a timely manner and under the supervision of a pediatrician;
- minimize contact with household allergens (chemicals, dust, animal hair);
- use pillows and blankets with hypoallergenic fillings;
- refuse any interior items that accumulate dust (carpets, heavy curtains);
- regularly ventilate the house and do wet cleaning;
- create a favorable psychological environment in the family.
The most effective measures are aimed at generally strengthening the body and stimulating the immune system. These include an active lifestyle, good nutrition, daily walks in the fresh air, and hardening. SM-Doctor employs qualified pediatric pulmonologists, allergists and immunologists. Specialists will assess the child’s condition in detail, make an individual prognosis for bronchial asthma and, upon objective diagnosis of the disease, prescribe targeted treatment. Contact the best doctors who will help your child breathe deeply, grow and develop correctly!
Reasons for the development of pathology
Increased bronchial reactivity may be due to:
- Hereditary predisposition (about 60% of children have relatives suffering from bronchial asthma). The disease may not manifest itself, but if: the child was born as a result of a difficult birth or after a difficult pregnancy;
- when he was born premature;
- If he lives in an environmentally polluted city, his chances that asthma will manifest itself in early childhood greatly increase.
- dust: industrial and domestic;
animal saliva;
Most often, asthma is triggered by a combination of several allergens.
The course of asthma is aggravated by diseases of the internal organs. The main “fault” lies with the gastrointestinal tract, where dysbacteriosis, gastritis, gastroduodenitis, constipation, and biliary dyskinesia can develop. The intestines are an excellent reservoir for toxins. In case of illness, they can remain there for a long time and gradually enter the blood.
Reasons for the appearance of a child
Speaking about the causes of bronchial asthma in a child, the following should be noted:
- All children diagnosed with asthma are allergic . And this pathology is genetic in nature. At the moment when the disease is diagnosed, there is almost always an underlying illness - atopic dermatitis or hay fever.
- Frequent colds and respiratory diseases can also be a trigger for the development of asthma. These ailments lead to changes in the structure of the bronchial tree; this occurs as a result of damage to the walls of the bronchi. In this case, allergens can easily penetrate the bronchi and create an imitation of an asthmatic condition. Very often, before the clinical picture of bronchial asthma, a child experiences frequent obstructive bronchitis.
- Bronchospasms that develop when allergens enter the body can complicate the course of the disease. Allergens can be animal hair, dust mites, plant pollen, and medications. In infants, food allergies are most often diagnosed, while in older children, it is mainly dust allergies.
- Physical overexertion is also one of the reasons for the development of bronchial asthma. In addition, psycho-emotional overload can also act as a catalyst. An unfavorable family environment can have a side effect on the development of this rather dangerous disease.
- Poor environmental conditions. Harmful emissions into the atmosphere and living in areas with busy highways provoke a deterioration in the functioning of the child’s immune system, which can give impetus to the development of asthma. Tobacco smoke is also a provoking factor.
- The so-called “aspirin” asthma is the human body’s reaction to acetylsalicylic acid. It acts as an allergen. If a child takes aspirin-based medications, the components of the active substance may release some bioactive substances that provoke bronchospasm.
- Disturbances in the functioning of the digestive system are another reason for the development of bronchial disease. The occurrence of bronchial asthma can be affected by the presence of gastritis, pancreatitis, and dysbacteriosis.
Symptoms
During bronchial asthma there are three periods:
- Remission. At the same time, the child feels absolutely or almost healthy; he has no cough, wheezing, or other symptoms. If asthma appears at an early age or has a severe course, then due to the constant lack of oxygen in the brain, the child lags behind in neuropsychic development, becomes tearful, and emotionally labile. Remission happens:
- complete: the child is not bothered by anything;
- incomplete: it is difficult to perform some actions, you less often want to play outdoor games;
- pharmacological: the disease can only be achieved by using drug therapy.
- Exacerbation. These are the time intervals during which attacks occur. Based on the duration of these intervals and the nature of their manifestation, the severity of bronchial asthma is diagnosed.
- An attack of bronchial asthma. This is the name of the condition when the main symptom occurs - difficulty in exhaling and wheezing when exhaling. This status usually occurs at night or in the evening; in children it is often preceded by special pre-attack signs.
The symptoms that can be used to suspect bronchial asthma in children are precisely the manifestations of an attack. This can begin with the appearance of pre-attack signs, which are observed from several minutes to three days. This:
- tearfulness;
- increased irritability;
- sleep disturbance;
- poor appetite;
- at first - the release of copious mucous snot, then - an obsessive dry cough, headache, after a few hours the cough intensifies and becomes a little wetter.
The attack itself begins in the evening or at night, when the following symptoms appear:
- dry cough, which may improve if the child is sat down or stood up;
- breathing becomes whistling, hoarse, inhalation is especially difficult;
- fright;
- the child is tossing about in bed;
- body temperature is normal, may rise slightly;
- the skin is pale, moist, with blue around the mouth;
- increased heart rate.
The attack may initially go away on its own within a few minutes to several days. You should not expect that the situation will resolve on its own, because this is dangerous due to a lack of oxygen in the brain and other vital organs. In this case, help is needed: optimally - inhalation of bronchodilator drugs (best of all - non-hormonal "Berodual").
After the attack has passed, the cough becomes wet, that is, bronchial mucus is coughed up. In children over 5 years old, it is clear that sputum due to asthma is viscous and glassy.
The course of the attack depending on the type of asthma
With the development of a subtype such as asthmatic bronchitis, which usually develops against the background of acute respiratory infections, the following symptoms appear:
- moist cough;
- dyspnea;
- difficulty breathing.
The difference between allergic asthma is the rapid development of an attack. If help in the form of inhaled bronchodilators is started immediately, the attack quickly subsides.
Non-allergic asthma is characterized by the gradual development of an attack. The assistance provided does not lead to an immediate effect.
Classification of attacks according to their severity
| Type of attack | Mild attack | Moderate attack | Severe attack | Status asthmaticus is a serious condition that can develop either on its own or as a result of an overdose of bronchodilators. |
| Breath | Slight difficulty breathing | Noisy, whistling, breathing involves the wings of the nose and the muscles between the ribs | Breathing is both more frequent than normal and noisy, and requires the inclusion of all muscles in the act of saturating the blood with oxygen | Frequent, noisy |
| Cough with asthma | Dry, as if in spasms | Attacks, after which thick, viscous sputum is difficult to clear | May not be | In this case, coughing and vomiting are signs of improvement |
| Speech | Not broken | Speak in separate phrases or words, with difficulty | Cannot speak, has difficulty pronouncing individual words | Impossible: all the body’s energy is spent on the act of breathing |
| General state | Worse than in health, but generally not bad | The child is capricious and restless. Pale skin, bluish lips | The child is very restless. The skin is pale bluish; cold sweat on the head, bluish lips | Very severe, may be accompanied by loss of consciousness or inappropriate behavior |
Severity depending on the course of asthma exacerbations
The treatment of asthma in a child depends on this classification. The main criteria on which it is based can be assessed by any parent. Some of them are determined by the doctor and are described in the “Diagnostics” section.
| Sign | Mild, episodic asthma | Mild asthma | Moderate asthma | Severe asthma |
| How often do choking symptoms appear? | Less than once a week, short-term | 1 time/7 days or more often, not every day | Daily | Constantly |
| Exacerbations | Lasts several hours - several days. Between exacerbations the child feels well and breathes normally | Lead to disruption of physical activity and sleep | Disturbs physical activity and sleep | Frequent, significantly limit physical activity |
| Frequency of night symptoms | 2 times a month or less | More often than 2 times a month | More than once a week | Frequent |
| Peak expiratory flow (PEF) or FEV in 1 second | More than 80% of normal | More than 80% of normal | 60-80% of normal | Less than 60% of normal |
| With daily fluctuations of less than 20% | Daily fluctuations: 20-30% | Daily fluctuations – more than 30% | Daily fluctuations – more than 30% |
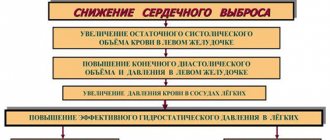
Extrapulmonary complications
The consequences of bronchial asthma are manifested not only in disruption of lung function. Many other organs and systems may also be affected.
Most often the disease affects:
- cardiovascular system;
- metabolism;
- CNS;
- Gastrointestinal tract.
Features of asthma manifestations in children of different ages
Bronchial asthma manifests itself differently in different age groups. Parents need to pay attention to the characteristics of symptoms in order to provide timely help to their child, diagnose the disease, and then achieve complete and stable remission through constant or course use of medications.
Features of the course in infants
At the age of up to 1 year, asthma is most difficult to diagnose, since its manifestations differ from the “usual”, classic ones described above:
- there is definitely a prodromal period with discharge of liquid mucus from the nose, constant sneezing, dry cough;
- the only signs determined by the doctor are swollen tonsils, isolated dry wheezing over the lungs;
- the child becomes restless and irritable;
- sleeps poorly;
- from the gastrointestinal tract there may be either constipation or diarrhea;
- breathing becomes “sobbling”, inhalations become frequent and short, exhalation becomes whistling and noisy.
Features in children 1-6 years old
Up to 2 years of age, it may just be increased frequency and intermittency of breathing during sleep, during outdoor games, or physical education.
For children 2-6 years old this is:
- restless sleep;
- periodic coughing, which can only occur during sleep;
- a dry cough, and sometimes a feeling of chest compression, appear during physical activity or outdoor games;
- If you breathe through your mouth, a strong dry cough occurs.
For schoolchildren
Signs of asthma in children of this age are:
- cough in sleep;
- cough after exercise;
- children try to run and jump less;
- During a coughing attack, the child tries to take a sitting position, while bending and leaning forward.
Asthma in teenagers
Usually by this age the diagnosis of asthma has long been established. The child already knows what can trigger an attack and must have an inhaler with him. It often happens that by adolescence, asthma seems to go away, but in fact, the increased reactivity of the bronchi remains, “waiting in the wings.” There are often cases where a disease that had passed in a teenager returns in old age.
conclusions
Getting rid of asthma forever is not an easy task. However, there are such cases, you just have to not give up. And the main attention should be paid to increasing immune defense - the main barrier to any disease.
Bronchial asthma is a common disease that is hereditary. Once a diagnosis has been made, it remains with the person forever - this is the bitter truth. But the disease has different stages and progresses in different ways. Nobody forbids using folk remedies in parallel with traditional methods. Maybe they will bring relief.
Diagnostics
Parents of children who have:
- Almost any cold is accompanied by a cough and dry wheezing, which gives the doctor the right to diagnose “Broncho-obstructive syndrome”;
- when attacks of wheezing or dry, unproductive cough occur: a) in the warm season, during the flowering of certain plants;
- b) after physical activity;
- c) while taking certain medications (especially if they contain acetylsalicylic acid);
- d) during fear, stress, strong emotion.
The main diagnostic method is peak flowmetry. It is performed using a portable peak flow meter, which resembles a tube into which the child will need to exhale air at maximum speed. This will allow you to estimate the maximum expiratory flow rate, thanks to which you can judge the patency of the bronchi.
Peak flowmetry is carried out starting from the age of 5, when it is already possible to cooperate with the child. It is performed 2 times a day: first in a hospital setting, then at home, simultaneously recording the baby’s daily routine and medication schedule. This way you can analyze what affects the occurrence of an attack and the effectiveness of the medications taken.
Peak flowmetry is performed standing, at one selected time, before taking medications. If you need to evaluate the effectiveness of inhaled bronchodilators, measurements are taken before inhalation, and then 20 minutes after taking the medicine. The assessment is carried out according to a nomogram, which takes into account not only the obtained indicators, but also the child’s growth.
The normal peak expiratory flow rate (PEF) is 80-100%, with daily deviations less than 20%. “Precaution” - PSV 60-80%, daily fluctuations 20-30%. In this case, it is necessary to increase the dosage of those drugs that make up the “basic therapy”.
If PEF is less than 50%, and daily fluctuations are more than 30%, urgent care for bronchial asthma is needed, which should be started at home, followed by hospitalization.
Is a complete cure possible?
What is the answer to the question - is bronchial asthma treatable or not? It is impossible to completely get rid of bronchial asthma. Despite all the new drugs regularly developed by medical scientists, a panacea for this disease still cannot be developed. You can put together all the treatment methods (taking powerful medications, inhalations, heating, compresses and all kinds of folk remedies), but even this will not be able to normalize the functioning of the respiratory system affected by bronchial asthma.
However, this does not mean at all that a patient with bronchial asthma will have to see life in less bright colors and lose precious moments of life to attacks of suffocation. Properly selected means of maintaining the body in normal condition by the attending physician will allow you not to be distracted by the disease and live a full life. In medical practice, there are very rare, unique cases where a patient was able to be relieved of the symptoms of bronchial asthma for quite a long time. However, the reason for this is not special treatment methods, but the individual characteristics of the human body.
Statistics on the growth of bronchial asthma
It is worth noting that perseverance, a focus on results and the belief that treatment can restore all functions of the body are of great importance in the fight against asthma. Unfortunately, even in those rare cases when the patient managed to get rid of the symptoms of bronchial asthma for a long time, relapse of the disease always occurred. On this basis, we can make the final conclusion that one hundred percent healing is impossible. Bronchial asthma is a chronic disease, and if once it affects the human body, then you need to be prepared for the fact that it will now become a part of a person’s life.
Treatment of the disease
Treatment of bronchial asthma in children begins with eliminating from the child’s life those things that can trigger an attack. Firstly, this is a hypoallergenic lifestyle, and secondly, a hypoallergenic diet.
Hypoallergenic life
To ensure that your child gets as few allergens as possible, follow these rules:
- store books in a closed cabinet;
- Do not store clothes, especially woolen ones, in the children’s room, and certainly do not spray them with moth repellents;
- do not buy soft toys for children; clean gifted items with a vacuum cleaner, after wrapping them in damp gauze;
- wash soft toys and bedding with hypoallergenic powders with the addition of acaricidal agents to kill possible house mites;
- remove pets from the house;
- if you have fish, feed them “wet” food, not dry food;
- Constantly ventilate the room, use air purifiers such as a HEPA filter, which will remove wool, dust, and fungal spores;
- the child should not be in the room during cleaning;
- the bathroom and toilet should be cleaned from mold spores with vinegar;
- The optimal covering for toilets and bathrooms is tile, not linoleum.
Recovery in older people
As for the treatment of asthma in older people, the main emphasis is on eliminating symptoms. Since in such people this disease is the result of natural aging and weakening of the body, age-related deformation of the bronchial region.
Much attention is paid to taking vitamins and strengthening the immune system. This therapy helps the body fight allergens. It is also necessary to reduce the pain of attacks. In some severe cases, antispasmodics are prescribed to completely eliminate pain.
In older people, any attack of suffocation can become critical. Therefore, you should always keep your inhaler with you.
Drug treatment
It includes 2 aspects:
- basic therapy;
- emergency medications.
This is the name of drug treatment aimed at suppressing allergic inflammation and predisposition to bronchospasm. Taking basic therapy medications lasts at least 3 months; in severe cases, they have to be used year-round.
Basic therapy can be:
- hormonal;
- non-hormonal;
- additional.
Non-hormonal therapy
This includes several groups of drugs. Let's take a closer look at them.
Mast cell membrane stabilizers
As mentioned above, the submucosa of the bronchi contains so-called mast cells. They contain granules with various substances - inflammatory mediators. When faced with an allergen, the cell membrane becomes permeable, and substances from the granules come out, triggering bronchospasm, coughing, and mucus secretion.
If you “fix” the membranes of mast cells, you can avoid swelling of the bronchial mucosa and their spasm. With the help of these drugs, the attack is not stopped, but - what is much more important - it is prevented, lengthening the intervals between the symptoms of suffocation and cough.
Unfortunately, the effect of these drugs does not occur immediately; They have a cumulative effect, so you need to take them for at least 3 months. They begin to “work” after 2-12 weeks, and their effect continues for some time after the end of the course.
Membrane stabilizers include the following drugs:
- "Tailed" in the form of an inhalation aerosol;
- "Cromogen" - aerosol for inhalation;
- “Intal” (sodium cromoglycate) and “Intal plus” – capsules with powder for inhalation;
- “Tyledmint” is an inhaler with a special device that creates a cloud of fine particles of medication in front of the mouth, which improves drug delivery to small-caliber bronchi by 1.5 times;
- "Ketotifen" is a drug in tablets.
You need to start using them 10-14 days after the start of flowering, if the attacks are caused by pollen of seasonal plants.
"Intal" is prescribed 4 times a day, "Tailed" and "Tailedmint" - twice. If a mild attack occurs while using the medication, instead of Intal you can use Intal Plus, which contains not only a membrane stabilizer, but also a bronchodilator. “Intal+” is used for a short course; after the exacerbation ends, you need to switch back to “Intal” or “Tailed”.
Use inhalers with Intal, Cromogen or Tailed as follows:
- to ensure that the substance reaches the mast cells of the bronchi, it is recommended that the child inhale bronchodilator drugs before using these inhalers;
- You should try to take as many breaths as possible from one capsule;
- you need to inhale the medicine with your head thrown back so that it is easier for the medicine to reach its destination;
- In some children, Intal may cause bronchial irritation, so at the beginning of treatment it may be necessary to use bronchodilators (Berodual, Salbutamol);
- if, despite the mast cell stabilizer being used, the child experiences frequent seizures, it is necessary to discontinue this drug and replace it with another long-acting agent;
- when asthma is combined with an allergic runny nose or food allergy, eye drops (Opticrom) or a nasal inhaler (Lomuzol) with similar drugs are additionally used.
Such drugs are not discontinued abruptly, they are “removed” gradually, under the control of peak flow measurements.
The advantages of these drugs are:
- relief of asthma attacks;
- ease of use;
- safe;
- no addiction;
- It is optimal to use it in a child with bronchial asthma due to a viral infection instead of the usual interferons or other agents.
Antihistamines
The purpose of these drugs is to disable the receptors to which the main internal allergenic substance, histamine, binds.
First generation drugs include: Suprastin, Diphenhydramine, Diazolin, Tavegil, taken 2-3 times a day. They cause drowsiness and act for a short time. Now they will be used only during the relief of an attack, in the form of intramuscular injections.
To prevent suffocation, second- and third-generation histamine receptor blockers are currently prescribed. These are Fexafenadine (Telfast), Erius, Cetrin, Ebastine. The same drugs are also used during exacerbations of asthma. They are used for another month after this.
Leukotriene receptor antagonists
Preparations with the active substance zafirlukast (Akolat) or montelukast (Singulair) are available in tablets. They are especially effective in the case of exercise asthma and aspirin-induced asthma. These drugs are also effective if there is a need to use inhaled hormonal drugs: leukotriene receptor antagonists help avoid increasing the dose of hormones.
Specific immunotherapy
This is the name of the treatment when the allergens that cause an asthma attack are introduced into the child’s body in microdoses, with a gradual increase in the dose.
SIT has been used since 5 years. Treatment begins during the period of remission. It is most effective when asthma is combined with allergic rhinitis or when you are allergic to one substance.
Hormonal basic therapy
It is prescribed for frequent exacerbations of the disease, when without the use of these drugs the development of status asthmaticus is possible. This therapy is more effective than any other in suppressing swelling, the release of histamine and other substances contained in mast cells. Thereby:
- peak flow measurements increase;
- daytime and even nighttime asthmatic attacks go away;
- the use of bronchodilators is not required;
- the chance of needing emergency care is reduced.
A huge disadvantage of hormonal therapy is that it is addictive and often requires increasing the dose. In addition, it can cause the development of fungal stomatitis.
The most commonly prescribed drugs are: Becotide, Seretide, Symbicort.
Alternative Therapies
Other types of treatment are also used in the treatment of asthma: physiotherapy, treatment with herbs, essential oils, and homeopathic medicines.
Phytotherapy
This type of treatment can be used after consultation with the attending physician and only during the non-attack period, under the control of PSV. The following recipes are used:
- Take 3 parts of nettle leaves, 2 parts of coltsfoot leaves, 5 parts of wild rosemary herb, mix. Remove 4 tablespoons from the mixture, add a liter of cold water, and leave to brew overnight. In the morning, boil over low heat for 7-10 minutes, cool, and strain. Give 1-2 times a day; dosages are listed below.
- Mix 10 tsp. coltsfoot leaves, 12 tsp. wild rosemary herb, 4 tsp. licorice roots and elecampane rhizomes, 6 tsp. nettle leaves. Mix all the herbs, add 4 tbsp. into an enamel bowl, add a liter of water at room temperature, leave for 8 hours. Next, put the infusion on low heat, let it boil and simmer for 10 minutes. After cooling and straining, you can consume 1-2 times a day.
- Take equal parts powder of licorice root, knotweed, nettle and calendula, mix. Next you need 3 tbsp. the mixture, which is poured with 0.5 liters of boiling water, is placed in a water bath, where the infusion is kept in boiling water for another 15 minutes, after which it is filtered and cooled.
Dosages:
- infants - 1 tbsp. l. appointment;
- children 1-3 years old - 2 tbsp per dose. l.;
- from 3 to 10 years – 3 tbsp;
- 10-12 year olds – 50 ml;
- over 12 years old, like adults - half a glass.
Homeopathy
As an auxiliary therapy, you can use drugs prepared directly by a homeopathic doctor. Some homeopaths recommend eliminating sensitivity to allergens with new generation drugs from the Italian laboratory Guna. This is, for example, Allergy Plex 31 - Fur (ALLERGOPLEX 31 - Animal fur) or Allergy Plex 29 - Pollens and dust (ALLERGOPLEX 29 - Pollen and dust).
These drugs are prescribed after consultation with an allergist and identification of the substances that cause an attack in the child. They are selected together with the doctor of this laboratory.
Physiotherapy
To prevent exacerbations of asthma in children, the following physiotherapeutic methods are used:
- breathing exercises (for example, according to the Buteyko method or Strelnikova gymnastics);
- acupuncture;
- treatment with mountain air, including in sanatoriums located in the highlands: in Kislovodsk, on the southern coast of Crimea, in the Elbrus region;
- massage is simply a manual intervention and with the addition of essential oils to which the child is not allergic (for example, thyme, lavender, tea tree).
In addition to using various therapeutic interventions, parents should not neglect visiting asthma schools, where parents and children are thoroughly trained in the rules of behavior during an attack, methods of its timely recognition and prevention, and alternative methods of self-help during an attack. Psychologists work with sick children in asthma schools.
Why you shouldn’t delay treatment
It is easier to prevent a disease than to deal with its consequences and complications. Due to their young age and underdeveloped body, in children the disease develops faster and is more severe than in adults. It often develops in newborns and children who do not yet know how to speak, and therefore are not able to explain what and where they hurt. This greatly complicates diagnosis and treatment.
Therefore, a lot depends on the parents - they must carefully monitor all the symptoms and do not hesitate to consult a doctor or call an ambulance. Considering the dangerous complications bronchial asthma causes, any delay or poor-quality treatment can seriously damage the health or life of the child.
Help during a seizure
Emergency care for asthma in a child is as follows:
- Place your child in a sitting position.
- Provide fresh air.
- Call an ambulance.
- Try to calm the child down.
- Free the child from constrictive clothing.
- Inhale bronchodilators. It is optimal if it is “Berodual” in the form of an inhalation solution, which will be inhaled using a compressor inhaler (nebulizer) in an age-specific dosage. You can use both “Berodual” in the form of a ready-made inhaler, and “Ventolin” (“Salbutamol”) in the form of a solution or inhaler. "Berodual" is preferable, it causes less tachycardia.
- If you don’t have an inhaler at hand, you can give Euphyllin in tablets so that the dose is 3 mg/kg per dose.
It is very important not to overdose on a bronchodilator, otherwise you can cause status asthmaticus, a life-threatening complication that requires mandatory hospitalization. The number of inhalations is no more than 5 times a day. During 1 administration, the inhaler head can be pressed 3-4 times. It is optimal to use a spacer into which 1-2 injections of the drug are injected. If you don’t have a ready-made spacer, you can make one by cutting off 2 plastic bottles. Next, throw away their lower parts and place the upper parts next to each other so that the neck faces outward on each side. In this case, the child takes 1 neck in his mouth, and the inhaler is inserted into the second.
From a spacer, homemade or industrially produced, you need to inhale a bronchodilator drug for at least 5 minutes.
For drugs produced in the form of powder inhalers, devices called “turbuhaler” and “diskhaler” are used. If asthma attacks are frequent, it is worth purchasing an “easy breathing” system for your child. This is a device connected to a spacer, which makes it possible to synchronize the child’s breathing and the flow of the drug into the bronchi. This way, you won’t have to wait until the baby is about to take a breath to inject the drug, and most of the medicine will not remain in the pharynx, but will enter the bronchial tree.
Inhalers as part of therapy
Doctors, explaining whether asthma can be treated or not, claim that it is impossible to do without the use of inhalers.
After all, they have advantages that make them simply irreplaceable:
- Neutralization of suffocation in asthmatics of all ages occurs in 5 seconds.
- The uniformity of the spray eliminates the possibility of an allergic reaction inside the oropharynx. This is dictated by the rapid penetration of the drug into the respiratory tract and lungs. This ensures uniform spraying.
- Suitable for use by children.
Inhalers are considered one of the most effective means of relieving asthma symptoms. But you should pay attention to the composition of the drugs. Some components can cause bronchial spasms with prolonged use.