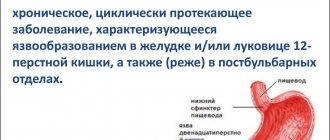
What is a perforated gastric ulcer?
A perforated stomach ulcer belongs to the category of severe, life-threatening diseases. A perforation occurs in the wall of the organ and the contents flow directly into the abdominal cavity. As a result, peritonitis develops, which requires immediate surgical intervention.
Currently, in Russia, perforated ulcers have been diagnosed in almost 3 million people. Relapses occur in 6% of patients. Men are more often affected by the disease. The hormone estrogen produced by the female body has a restraining effect on the activity of the secretory glands of the gastric mucosa.
Content:
Prevention
Necessary measures to prevent ulcer perforation:
- maintaining a proper diet;
- correctly selected diet;
- maintaining a healthy lifestyle;
- quitting smoking, alcohol;
- constant examination by a gastroenterologist.
List of references: https://ru.wikipedia.org/wiki/Perforated_ulcer https://www.mgzt.ru/content/probodnaya-yazva-stereotipy-kotorye-nam-meshayut-0 https://www.10gkb.by /informatsiya/stati/probodnaya-yazva-zheludka-i-12-perstnoj-kishki https://www.aptekar76.ru/bolezni/detail/Probodnaya_yazva_zheludka_i_dvenadcatiperstnoj_kishki/ https://www.mediasphera.ru/issues/khirurgiya-zhurnal- im-ni-pirogova/2015/11/downloads/ru/440023-12072015115 Valdanova M.E., Zhdanova A.V. Perforated ulcer of the stomach and duodenum in patients of the older age group // Smolensk Medical Almanac. 2021. No. 1. https://medi.ru/klinicheskie-rekomendatsii/probodnaya-yazva-u-vzroslykh_14206/ Notes from the author of the article, based on personal experience. This material is purely subjective and is not a guide to action. Only a qualified specialist can determine an accurate diagnosis and prescribe treatment.
Last modified: 03/18/2020
Causes of perforated stomach ulcer
People suffering from chronic peptic ulcer disease, as well as those who have suffered an acute form of the disease, are at risk of developing a perforation defect.
Perforation can be initiated by:
- Inflammation that occurs around the main focus of mucosal damage;
- Overeating (the stomach cannot cope with a large amount of food);
- Increased acidity of gastric juice (leads to an aggressive environment);
- Excessive consumption of foods seasoned with spices and alcohol;
- Sudden physical exertion;
Modern research indicates that the causative agent of peptic ulcer disease is the bacterium Helicobacter pylori (which has initially aggressive strains). Almost 50% of all humanity is infected with it. But contamination is not the only cause of peptic ulcer disease. Any violation of the body’s protective functions activates the pathogenic influence of microorganisms.
Factors that increase the risk of peptic ulcer disease:
- Suppressed immune system;
- Impaired quality or duration of sleep, night shift work;
- Prolonged stress;
- Taking certain medications. Long-term treatment with non-steroidal anti-inflammatory drugs (including aspirin) is not allowed; even short-term anticoagulants (warfarin, heparin), corticosteroids (prednisolone), and some chemotherapy drugs can have a pathogenic effect;
- Smoking (has an indirect effect on increasing the content of hydrochloric acid and disrupting microcirculation in the mucous membranes);
- Excessive alcohol consumption (leads to direct damage to the mucous membranes);
- Violation of food intake and nutritional quality. Too low or high temperature of food, foods with high fat content, smoked foods, etc., dry food unnecessarily load the stomach and provoke the occurrence of diseases;
- Hereditary factors;
- The presence of other pathologies of the gastrointestinal tract (for example, gastritis);
Symptoms
At different stages of a perforated duodenal ulcer, symptoms may vary. The first phase is characterized by the leakage of duodenal contents into the peritoneum, which is accompanied by severe pain. Depending on the flow strength and the size of the perforation, the period can last 3-6 hours. The pain can radiate to the pelvic area. If the patient has recently eaten, vomiting with particles of bile and blood may occur. Additionally, there is a decrease in pulse and blood pressure, general pallor and tone of the abdominal muscles.
During the second phase, a false improvement in well-being occurs, the indicators return to normal, but at the same time there is a feeling of thirst, dryness in the mouth, and the tongue changes color. At the last stage, the patient’s condition noticeably worsens, body temperature rises, the abdomen swells, and vomiting begins. On palpation, you can feel fluid in the peritoneum.
Symptoms of a perforated stomach ulcer
The typical form of the disease is accompanied by the entry of stomach contents into the free abdominal area.
There are three periods of development:
- Period of chemical peritonitis. The duration of the course is from 3 to 6 hours. Depends on the diameter of the hole and the volume of secretions from the stomach. Accompanied by acute pain in the stomach. Severe pain is possible in the peri-umbilical segment and in the right hypochondrium. Subsequently, they cover the entire abdomen. Perforation of the anterior wall of the stomach can manifest itself in pain in the area of the left side of the abdomen and left forearm. Painful sensations are characterized by the duration of manifestation. Vomiting occurs rarely. Blood pressure is reduced, but pulse is usually within normal limits. Breathing becomes shallow and rapid. The skin turns pale and sweating increases. The muscles of the front part of the abdomen are tense, and there is an accumulation of gases in the abdominal cavity.
- The period of bacterial peritonitis. It begins 6 hours after perforation. The abdominal muscles relax, breathing becomes deeper and sharp pain disappears. The person feels relieved. During this phase, there is an increase in temperature, an increase in heart rate and a further change in blood pressure. A period of increasing toxicity begins, which leads to an increase in the volume of gases and paralysis of peristalsis. The tongue becomes dry, with a gray coating on the front and side surfaces. The patient's general behavior changes. He experiences euphoria and relief, becomes uncritical of his condition, and does not want to be disturbed. If emergency medical care is not provided during the period of increased intoxication, then the person moves to the third, most severe stage of the disease.
- Period of acute intoxication. It begins, as a rule, after 12 hours from the moment of illness. The main manifestation is uncontrollable vomiting, leading to dehydration. Visually you can notice changes in the skin. They become dry. There is a sharp change in body temperature. An increase to 38°-40° is replaced by a decrease to 36.6°. The pulse reaches 120 beats per minute. Upper blood pressure drops to 100 mmHg. The general condition of the patient is characterized by lethargy, indifference, and a slow reaction to external stimuli. The abdomen becomes enlarged due to the accumulation of free gas and liquid. The process of urination is disrupted and eventually stops completely. If a person has reached this phase of the development of peritonitis, then it is almost impossible to save his life.
Description
A perforated or perforated duodenal ulcer is a serious condition with high mortality. When the duodenum is ulcerated, the stomach is often affected. This forms a passage from the organ to other parts of the gastrointestinal tract or peritoneum. Due to constant exposure to irritants of a chemical, physical and bacterial nature located in the duodenal contents. Against this background, peritonitis develops. This consequence requires a strict diet and urgent surgical intervention.
Perforation of the ulcer most often occurs in the anterior wall of the bulbous part of the duodenal process. This outcome is equally characteristic of the acute course and the acute chronic phase of the ulcerative process. The average size of wounds is 3 mm, less often - up to 100 mm.
Classification of perforated ulcers
- According to the clinical course of the disease:
- Typical form. Characterized by the leakage of stomach contents into the abdominal cavity;
- Atypical form. The contents enter the omentum or omental bursa, possibly leaking into the retroperitoneal tissue or intercommissural area;
- Perforation with bleeding into the abdominal cavity or gastrointestinal tract;
- According to the stages of development of peritonitis:
- Stage of primary pain shock;
- The stage of development of bacterial peritonitis, accompanied by contamination with microorganisms;
- The stage of the inflammatory process, accompanied by feelings of imaginary well-being;
- The stage of severe disease, accompanied by the occurrence of purulent peritonitis;
- According to pathological and anatomical characteristics:
- Perforation of a chronic ulcer (complication of peptic ulcer);
- Perforation of an acute ulcer;
- Perforation when the wall of a hollow organ is damaged by a tumor formation;
- Perforation due to parasitic diseases;
- The occurrence of a defect due to a violation of local blood circulation;
- According to the location of the outbreak:
- Gastric ulcer (anterior, posterior wall, lesser or greater curvature);
- Duodenal ulcer;
- Pyloroduodenal ulcer;
- Combined ulcer (stomach and duodenum);
Possible complications and consequences
If you do not seek medical help in a timely manner, severe purulent complications of a perforated ulcer, including generalized sepsis, may develop. Such conditions are life-threatening.
Postoperative complications of a perforated ulcer may include:
- bronchopneumonia;
- peritonitis;
- failure of the sutures with repeated release of intestinal contents into the peritoneal cavity;
- gastrointestinal bleeding;
- violation of the evacuation function of the stomach.
Patients with immunodeficiency and the elderly are more at risk of developing postoperative complications of a perforated ulcer.
Methods for diagnosing perforated ulcers
Perforation is characterized by an attack of sharp, sudden pain. If there is a history of peptic ulcer, gastritis, etc., then the task becomes easier. As a rule, a differential method is used for diagnosis.
It consists of examining the body, taking into account the presence/absence of the following pathologies:
- Acute appendicitis;
- Acute cholecystitis;
- Perforation of tumor formations;
- Hepatic colic;
- Acute pancreatitis;
- Thrombosis;
- Dissecting abdominal aortic aneurysm;
- Myocardial infarction;
- Lower lobe pneumonia;
- Pleurisy;
- Pneumothorax;
Additional research methods are:
- X-ray. The efficiency of diagnosing air filling of the abdominal cavity reaches 80%. But a similar picture can also be observed in the case of airy intestines or atony of the fallopian tubes;
- Electrogastroenterographic. Allows for a qualitative analysis of the evacuation function of the stomach and duodenum;
- Endoscopy. Used when X-ray results are negative, but perforation is suspected. Allows you to determine the presence of a peptic ulcer and the localization of the lesion. The study is carried out using air pumping, which helps determine the true clinical picture;
- Complete blood count (shows an increased level of leukocytes);
- Laparoscopy. Helps in qualitative and quantitative analysis of abdominal effusion. Has contraindications for use;
Laparoscopy is not used if the patient has:
- Obesity;
- Adhesions in the abdominal area;
- Violation of the integrity of the diaphragm;
- Pathology of blood clotting;
- The presence of large hernias on the anterior wall of the peritoneal region;
- General serious condition;
Perforation of the intestine from below, behind
Duodenal contents infect the retroperitoneal tissue. The main symptom is unexpected, sharp pain in the pit of the stomach that radiates to the back. Over time, the pain subsides. An acute inflammatory purulent process develops in the retroperitoneal tissue of the retroperitoneum. The period is characterized by the development of fever with chills. A swelling forms at the 10-12 thoracic vertebrae, which hurts on palpation. When listening to its area, you can hear a characteristic crunching sound - crepitus. X-ray shows increased gas formation in this area.
Treatment of perforated gastric ulcer
Perforated ulcers are treated surgically. Preoperative preparation consists of removing gastric contents and restoring blood pressure. Research is also carried out to select further actions.
Evaluated:
- Time elapsed since the onset of the disease;
- Nature of origin, size and localization of the ulcer;
- The severity of peritonitis and the area of its distribution;
- Age characteristics of the patient;
- Presence/absence of additional pathologies;
- Technical features of the hospital and the level of professionalism of doctors;
There are organ-preserving operations (suturing) and radical ones (resection, excision of ulcers, etc.).
Suturing the perforation is indicated in the presence of widespread peritonitis, high surgical risk (associated with the presence of concomitant pathologies or the age of the patient), and the absence of a history of ulcers in young people. The technique consists of excision of the edges of the ulcer and their subsequent stitching with two rows of sutures. With this method of solving the problem, the shape of the organ and the diameter of its lumen are preserved. At the end of the operation, temporary drains are installed. Further treatment with antiulcer drugs is prescribed.
Gastric resection is an operation that leads to the loss of a significant part of the organ. After the transfer, disability is established. Indications are the presence of chronic, large-diameter ulcers, suspicion of the presence of malignant tumors, the patient’s age less than 65 years in the absence of concomitant pathologies during the decompression period, the development of acute inflammation and purulent peritonitis, 6-12 hours after the onset of the disease.
In the absence of peritonitis, suturing of the wall of the perforated hole can be performed in combination with selective proximal vagotomy.
Excision of the ulcer using truncal vagotomy and pyroplasty is used in the presence of an ulcer of the pyloric part of the stomach, a combination of perforation with bleeding, and stenosis.
The absence of surgical intervention necessarily leads to death in the coming weeks after the development of the disease.
Statistics of deaths after surgery show that after 6 hours no more than 4% of patients leave, after a day - no more than 40%.
Forecast
A perforated ulcer is a life-threatening condition, resulting in death in approximately 8% of cases, even with timely diagnosis and surgical treatment. Relapses occur in less than 2% of cases. When surgical intervention is performed 12 hours after the onset of the disease and later, postoperative mortality increases to 20–40%. Treatment of a perforated ulcer at the stage of diffuse peritonitis is often delayed and does not have a positive effect.
Diet after surgery for perforated gastric ulcer
The first rule for recovery and reducing the risk of relapse is strict adherence to the doctor’s instructions. An exception to the rule “if you can’t, but really want to” doesn’t work. During the postoperative period, a strict diet is established. It can last from 3 to 6 months. The diet becomes more complex gradually.
Basic principles of the diet:
- The daily number of meals is up to 6 times, in small portions.
- All foods taken must be puree or semi-liquid.
- Food should be steamed or boiled
- Salt should be taken in limited quantities
- You should also limit your intake of simple carbohydrates (sugar, chocolate, baked goods) and liquids.
On the 2nd day after the operation, mineral water, fruit jelly, and weak, slightly sweetened tea are allowed.
After 2-3 days, the diet is replenished with rosehip decoction, pureed soups and porridges made from rice and buckwheat. Vegetable puree soups made from boiled carrots, pumpkin, zucchini, potatoes or beets. You are allowed to eat a soft-boiled egg and a steam soufflé made from pureed cottage cheese.
On the 10th day after the operation, puree from boiled carrots, pumpkin, zucchini or potatoes is introduced into the diet. Gradually introduce steamed cutlets, soufflés, purees, quenelles, meatballs or zrazy from lean meats or fish. They add cheesecakes, puddings, and cottage cheese casseroles. You can also use fresh pureed cottage cheese. In addition, whole milk and non-acidic dairy products (acidophilus, yogurt, matsoni) are introduced.
Only after a month does it become possible to consume bread products: dried bread, stale bread, crackers.
After 2 months, it is allowed to add fresh sour cream to food and consume kefir.
On the subject: Diet for stomach ulcers - what can and cannot be eaten?
Postoperative care
In the postoperative period, a special gentle diet is selected for the patient individually. The diet after surgery for duodenal ulcers should be strict and gentle.
Meals should be fractional. To avoid excessive stress, you need to eat small meals every 3 hours. The diet after a duodenal ulcer includes boiled or baked dishes.
Each dietary product must be crushed using a blender. There should be a minimum amount of salt in food. The diet after a perforated duodenal ulcer should contain foods that will not irritate the mucous membrane of the stomach and intestines.
Too hot or cold dishes, alcohol, carbonated drinks, rich broths, and coarse vegetable fiber are contraindicated.
Diagnosis of the disease
Methods used to diagnose a perforated ulcer include:
- conducting a general examination with palpation and identifying complaints;
- X-ray, which can detect air in the peritoneal area;
- General and biochemical blood test. This helps determine the presence of inflammation in the body and the level of intoxication;
- endoscopic examination. It determines the location of the perforation and the size of the damage. If there are problems with diagnosis, straightening the stomach walls with air is used;
- CT scan of the abdominal organs (almost 100% informative) helps to see free fluid and gas, thickening of the duodenal ligaments and gastric wall, and gastric ulcers;
- electrocardiogram. It is performed to determine malfunctions in the functioning of the cardiovascular system, which is necessary to know when preparing for surgery;
- esophagogastroduodenoscopy;
- Ultrasound. It helps to see the abscess, which is hidden in the intercommissural space, reveals the presence of fluid in the abdominal space;
- diagnostic laparoscopy. Laparoscopic examination is considered the most sensitive method for detecting a perforated ulcer. The disease should be differentiated from an abdominal aortic aneurysm, acute appendicitis, pancreatitis, cholecystitis, and myocardial infarction.