Hyperglycemia is a technical term and also a symptom that refers to an increase in blood glucose levels above the upper limit of normal, which is 3.4-5.5 mmol/L (60-99 mg/dL) in the fasting state. The danger is that symptoms can often go unnoticed or ignored, sometimes they begin to appear at levels of 15-20 mmol/l, while organ damage begins already after 7 mmol/l.
You can also find other numbers. For example, according to the book “Clinical Diabetology” (1998), which is referenced by the Russian-language Wikipedia, hyperglycemia is conventionally divided into three types (glucose indicator in brackets):
- light - 6.7-8.3 mmol/l;
- moderate – 8.4-11 mmol/l;
- severe – 11-16 mmol/l.
It also indicates the state of precoma (16.5 mmol/l or more) and coma (55 mmol/l or more).
The American Diabetes Association defines hyperglycemia as a blood glucose level between 5.6 and -7 mmol/L (100-126 mg/dL), above which diabetes mellitus is usually diagnosed. Exceeding the level of 7 mmol/l for a long time can lead to damage to organ tissue.
The word “hyperglycemia” itself comes from Greek: ὑπέρ – prefix “hyper”, γλυκός glycos – “sweet wine” or “must”, αἷμα Haima – “blood”, ία, -εια -ia – suffix for abstract feminine nouns.
General information
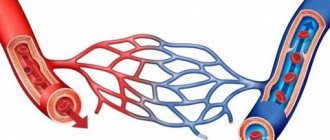
Carbohydrate metabolism largely determines the general state of metabolism . Carbohydrates take part in almost all types of metabolism: proteins (glycoproteins), nucleic acids (ribose/deoxyribose), lipids (glycolipids), nucleotides (ATP, AMP, ADP), nucleosides (adenosine), ions. Simple and complex carbohydrates are one of the main sources of energy that ensure the vital functions of the body and are an essential component of the diet. Disorders of carbohydrate metabolism are combined into several typical forms (groups) of pathology: hypo- and hyperglycemia , aglycogenoses , glycogenoses , hexoses and pentosemias .
Hyperglycemia is a clinical symptom characterized by an increase in blood glucose (in plasma) of more than 6.5 mmol/L on an empty stomach and more than 8.9 mmol/L at any time of the day). ICD-10 hyperglycemia code: R73.9 - Hyperglycemia, unspecified. Based on the glucose level (GLU), a mild state of 6.7-11.1 is distinguished. It is characterized by a significant and persistent increase in BPC to a level of 10.5-11.0 mmol/l and is combined with a disorder of the body’s vital functions. This kind of hyperglycemia is defined as hyperglycemic syndrome. The most severe manifestation is a hyperglycemic crisis (GPC > 16.5).
The subject of the article is early disorders of carbohydrate metabolism, which some authors define as “prediabetes”. Early disorders of carbohydrate metabolism usually include the state of impaired glucose tolerance (IGT) and impaired fasting glucose (IFG) or a combination of these conditions (IGT+IGN). It is generally accepted that prediabetes is accompanied by a high risk of developing type 2 diabetes, but in some cases prediabetes does not convert into type 2 diabetes and is assessed by a number of authors as an independent risk factor for the development of cardiovascular diseases. Essentially, these are borderline disorders of carbohydrate metabolism that precede the development of diabetes mellitus , i.e. hyperglycemia with glucose values insufficient for the diagnosis of diabetes.
It has been established that with IGN, liver insulin resistance and hyperproduction of glucose by the liver are more pronounced than with isolated IGT, which is confirmed by higher liver glucose production and the insulin resistance index. IGT is characterized by peripheral insulin resistance, confirmed by lower insulin . In cases of a combination of these conditions (IGT+NGN), the first phase of insulin secretion is disrupted.
According to the literature, the global prevalence of IGT in people aged 30 to 70 years is about 6.7% and continues to increase, and in the Russian Federation, about 19% of the active population have prediabetes, that is, these people are at risk of developing diabetes. Prediabetes, like T2DM, is associated with age and weight gain. Gender differences in the prevalence of early carbohydrate metabolism disorders have not been identified.
According to expert data, the risk of developing type 2 diabetes in people with IGT is 6 times higher than in people with normal glucose tolerance, and in cases of a combination of IGT/NGN, the risk is twelve times higher. The relative risk of overall mortality in persons with IGT is 1.48 times higher than normal, while the risk of cardiovascular complications increases by 1.66 times. In the presence of IFN, the risk of developing T2DM is 4.7 times higher than in persons with normal glucose tolerance. IFN is also associated with a relatively high risk of developing cardiovascular complications.
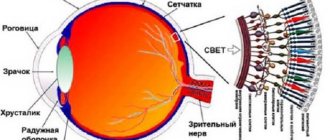
Thus, active intervention must be carried out already at the prediabetic level of glycemia (stage of NGN and IGT), thereby preventing the development of type 2 diabetes, which is accompanied by various complications in the form of visual impairment, atherosclerosis of the vessels of the heart, lower extremities and brain, nephropathy , and damage to the nervous system.
For this purpose, all individuals need regular screening, which makes it possible to identify IGT, IFN, and type 2 diabetes as early as possible and, accordingly, begin timely treatment, thereby preventing the risk of developing severe complications and potential disability of the patient in the future. For this purpose, the Postprandial Glucose test should be performed regularly, especially in persons at high risk of diabetes, which determines the blood sugar level after a meal (after 2 hours). This test allows you to identify prediabetes at an early stage, when fasting blood glucose levels are still normal. The frequency of self-monitoring of glucose levels is adjusted depending on the needs, specific circumstances and goals of the patient. The emergence of individual glucometers of various types for measuring glycemic levels makes self-monitoring relatively simple and accessible to most interested parties.
of diabetes mellitus, postprandial glucose test indicators are also used to assess the risk of complications from the cardiovascular system ( atherosclerosis , coronary artery disease) in T2DM.
Diagnostics
The examination is carried out in a clinic under the supervision of an endocrinologist or on an outpatient basis. Depends on the specific situation.
The methods are aimed at identifying possible diabetes or other similar conditions. In acute cases, the glucose level is first adjusted, and only then specialized diagnostics begin.
Sample list of events:
- Oral questioning of the patient regarding complaints. They are systematized and form a single complex. This is a necessary technique to determine the direction of further activities.
- Anamnesis collection. What could cause the change in sugar levels. Hyperlgicemia, as already mentioned, is quite likely after inflammation, strokes and other situations.
- Blood test for sugar. General analysis. Also a specific glucose load test.
- Ultrasound of the pancreas. A method for visual examination of an organ. Pancreatitis and other diseases of this structure often provoke pathologies in the future, as well as dysfunction.
- If a more accurate diagnosis is necessary, an MRI of the abdominal cavity is indicated. Targeted examination of the pancreas. Contrasting with a gadolinium-based agent is possible. This measure is needed to detect tumors.
In general, this is enough to make an accurate diagnosis.
Pathogenesis
The pathogenesis of prediabetes is caused by a qualitative/quantitative deficiency of insulin, which is based on a decrease in insulin activity in adipocytes, muscle tissue and hepatocytes, caused by a deficiency in insulin production by pancreatic β-cells and insulin resistance (decreased sensitivity of receptors to insulin). These disturbances in the post-receptor action of insulin, together with an increasing decrease in insulin production, contribute to an increase in glucose to the corresponding values of NGN (6.1–6.9 mmol/l) and/or IGT (7.8–11.0 mmol/l after OGTT with glucose) . In patients with moderate hyperglycemia, the underlying cause is a decrease in insulin sensitivity of peripheral tissues, mainly muscle tissue. And with hyperglycemia on an empty stomach, an additional negative effect may be an increase in glucose production by the liver.
First aid
A mandatory condition for correcting the condition is the person’s hospitalization in an endocrinology hospital.
The following should be taken as initial measures:
- Check your sugar level using a glucometer. This will allow you to assess the condition in general terms.
- At elevated levels (more than 8-13 units), insulin administration is required in the amount and according to the schedule prescribed by the attending physician. A special syringe or pump is used.
- It is obligatory to call an ambulance. It is better to do this from the moment the problem is discovered. To avoid causing fatal complications.
- Next, it is important to assess the general condition of the patient. If shortness of breath develops, you need to open a window or window to ensure normal ventilation of the room where the victim is located.
- The development of hyperglycemic coma is a complication of the pathological process. You can no longer do anything on your own. You need to turn your head to the side so that the person does not choke on vomit.
- Upon arrival of doctors, it is necessary to talk about the condition of the victim. First aid for hyperglycemia ends as soon as the doctors arrive. If possible, it would not be a bad idea to accompany the patient to the hospital to facilitate the registration process and provide all possible assistance to the doctors.
Without special equipment and drugs, not much can be done. Everything else falls on the shoulders of the doctors on site.
Causes
The causes of increased blood glucose vary widely, the main ones being:
- Hormonally caused hyperglycemia ( hyperthyroidism , diabetes mellitus , familial polyendocrine adenomatosis , acromegaly , pheochromocytoma , Itsenko-Cushing's disease ).
- Hyperglycemia of central origin (poisoning, brain injury with hemorrhages in the fourth ventricle of the brain, encephalitis , tumors ).
- Psychogenic disorders (stress).
- Diseases of the pancreas ( pancreatitis ), liver failure .
- Extreme prematurity of the child.
- Hyperglycemia against the background of the development of various critical conditions.
- Nutritionally-induced hyperglycemia (eating disorders - bulimia / long-term excess consumption of easily digestible carbohydrates; Prader-Willi syndrome - a predisposition against the background of obesity to the development of insulin-resistant diabetes in childhood; Sipe-Lawrence lipodystrophy - a predisposition to the development of T2DM; Urbach-Wiethe syndrome - a tendency to fasting hyperglycemia).
- Drug-induced hyperglycemia ( glucocorticosteroids , second-generation antipsychotics , stanines , thiazide diuretics , calcineurin inhibitors , etc.).
Risk factors for the development of carbohydrate metabolism disorders include:
- Presence of relationship with patients with T2DM.
- Age 40 years and older with a BMI ≥25 kg/m.
- Low (insufficient) physical activity.
- Persons with arterial hypertension , coronary artery disease.
- Polycystic ovary syndrome.
Symptoms
A feature of prediabetes is the absence of clear specific clinical symptoms characteristic of diabetes mellitus, which is primarily due to preserved energy supply to tissues and organs and slight glucosuria . In rare cases, symptoms of hyperglycemia at the stage of NGN and IGT manifest in the form of nonspecific patient complaints of increased fatigue, decreased ability to work, and worsening healing of wound defects.
Indirect signs of hyperglycemia at an early stage include:
- obesity or overweight;
- arterial hypertension;
- disorders of the cardiovascular system;
- atherogenic dyslipidemia (increased triglyceride levels and decreased cholesterol levels due to HDL (high-density lipoprotein);
- increased levels of uric acid in the blood ( hyperuricemia );
- fibrinolysis disorder .
On examination, most patients with prediabetes experience an increase in waist circumference to >94 cm in males and >80 cm in females. At the same time, fat mass is distributed predominantly on the torso with its relative decrease in the hips/buttocks area.
Hyperglycemia in children
Carbohydrates play a big role in the development and growth of a child and are an essential and significant component of food. They are involved in almost all types of metabolism: nucleic acids, proteins, lipids, nucleosides. Carbohydrates are essential for optimal functioning, especially brain function. Given the high metabolic rate in children, even minor deviations in carbohydrate metabolism cause disruption of other types of metabolism.
The causes of hyperglycemia in childhood are:
- neurogenic disorders;
- various endocrinopathies;
- liver pathology;
- psychogenic factors;
- binge eating.
In the neonatal period, hyperglycemia is more common and is found in 20-80% of premature babies weighing less than 1500 g. This condition is a prognostically unfavorable sign in this period, which can lead to death. The main cause of hyperglycemia is excessive infusion of glucose solutions during intensive care. An infectious process cannot be ruled out as the cause. Hyperglycemia often occurs in children who have suffered asphyxia and had respiratory disorders. An increase in sugar levels may be a manifestation of transient neonatal diabetes (decreased pancreatic function).
Endocrinopathies are associated with increased activity of hyperglycemic hormones: with an excess of glucagon , the formation of glucose from amino acids and intensive breakdown of glycogen , which is accompanied by an increase in blood sugar. Excess glucocorticosteroids stimulate the formation of glucose, and excess catecholamines stimulate the breakdown of glycogen. With hyperthyroidism, glycogenolysis (the breakdown of glycogen) is enhanced, glycogenesis (the formation of glycogen from glucose, the formation of glucose and its absorption in the intestine are stimulated.
Increased secretion of growth hormone enhances the breakdown of glycogen and inhibits glucose consumption. Neuro- and psychogenic disorders cause activation of the sympathoadrenal system, adrenal glands and the release of thyroid hormones. The hormones of these systems activate the breakdown of glycogen in the liver and the formation of excess glucose.
Overeating (consuming excessive amounts of simple carbohydrates over a long period of time) is considered a cause of hyperglycemia. In this case, glucose is quickly absorbed in the intestines, its level in the blood increases, and the liver is not able to convert it into glycogen in such quantities. When liver function is impaired, transient hyperglycemia always occurs after eating, which is associated with the inability of liver cells to quickly utilize glucose.
Hyperglycemia manifests itself in children as hyperglycemic syndrome and hyperglycemic coma.
Hyperglycemic syndrome includes:
- A persistent increase in sugar levels to 10.5–11.5 mmol/l.
- Detection of sugar in the urine ( glucosuria , which should not be normal).
- Severe, unquenchable thirst ( polydipsia ).
- Polyuria is excessive urination (urine output more than 3 L/day) due to increased glomerular filtration, increased urine osmolality and decreased reabsorption (reabsorption) of water in the tubules.
- Dry skin and signs of dehydration due to polyuria.
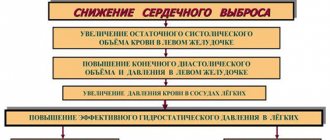
- Decreased blood pressure as a result of fluid loss and decreased cardiac output.
- Hyperglycemic (hyperosmolar) coma in children develops with diabetes mellitus due to a lack of insulin. There is an increase in sugar of 22–28 mmol/l or more. Hyperglycemia causes an increase in plasma osmolarity. An increase in osmolarity causes an increase in the permeability of the blood-brain barrier , which causes neurological symptoms. In newborns, increased osmolarity not only depresses the central nervous system and causes cerebral edema , but also causes hemorrhages inside the ventricles of the brain. In newborns with elevated levels of indirect bilirubin, its neurotoxicity increases.
Dysfunction of the central nervous system depends entirely on the level of increase in sugar:
- depression of consciousness;
- tonic-clonic seizures;
- dehydration;
- respiratory failure;
- apnea;
- disorders of the cardiovascular system;
- development of coma .
Complications and possible consequences
Hyperglycemia is a disease that always leaves consequences. They are especially dangerous for patients with diabetes. With the development of this pathology, all systems in the body are weakened, causing the consequences to become more serious. Prolonged neglect of hyperglycemia leads to the development of heart failure, stroke, thrombosis, heart attack, ischemia and other serious diseases.
Complications of hyperglycemia are as follows:
- Polyuria is kidney damage in which there is a strong outflow of urine. Because of this, the concentration of electrolytes in the body decreases, which disrupts the water-salt balance.
- Glucosuria is a phenomenon in which a certain amount of glucose enters the blood. This has a negative effect on the kidneys.
- Ketoacidosis is a phenomenon in which ketone bodies appear in the body. They enter the urine and blood.
- Ketonuria is a condition in which ketone bodies are excreted from the body through urine.
- Ketoacidotic coma is a pathological condition of the body caused by a serious jump in the level of ketone bodies in the body. It can be recognized by vomiting, abdominal pain, and increased body temperature. May lead to shortness of breath, convulsions, loss of consciousness and heart failure.
Diet
Diet 9th table
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1400 - 1500 rubles per week
Diet for insulin resistance
- Efficacy: therapeutic effect after a month
- Timing: constantly
- Cost of products: 1500-1600 rubles. in Week
Basic principles of nutrition for patients with hyperglycemia include:
- Reducing total calories to 1500 kcal per day.
- Exclusion of simple carbohydrates (sugar, sweets, baked goods, sweet desserts, confectionery, ice cream, jam, condensed milk, sweet drinks).
- Limiting fat intake due to its high calorie content.
- Increasing the amount of protein, as well as fiber up to 30 g/day due to vegetables with a low glycemic index.
The glycemic index reflects the rate at which carbohydrates are broken down into sugar and released into the bloodstream. Products with a high index sharply increase blood sugar levels, and their predominance in the diet will be accompanied by constant hyperglycemia. Patients' diets should be dominated by foods containing fiber, which is digested slowly and does not cause sudden spikes in blood sugar. These can be green vegetables, lettuce, all types of cabbage, unsweetened fruits, legumes, and whole grains.
Vegetables with a high index are excluded or sharply limited: potatoes, carrots, beets, tomatoes. More detailed recommendations can be found in the articles Diet for high blood sugar , Diet 9th table and Diet for insulin resistance .
Prevention
- Healthy eating.
- Weight loss and constant weight control.
- Increasing physical activity.
- Identification of high-risk groups (presence of abdominal obesity, heredity of diabetes mellitus, lipid metabolism disorders, high blood pressure, presence of fatty liver, polycystic ovary syndrome) and control of sugar levels in this group.
- Identification of patients with impaired glucose tolerance, fasting glycemia or HbA1C from 5.7-6.4%.
- It is especially important for these patients to follow a diet and increase physical activity.
- Periodic examination by a doctor (once every six months) and decision on the issue of taking metformin if non-drug treatment is ineffective.
Folk remedies
Following all the doctor’s recommendations, you can additionally turn to traditional medicine. Some medicinal plants contain insulin-like alkaloids and can lower glucose concentrations:
- Leave a spoonful of crushed dandelion root in 1 tbsp for 30 minutes. boiling water and drink 50 ml 4 times a day. A salad of dandelion leaves and greens is very healthy. Pre-soak the leaves in water. Season the salad with sour cream or butter.
- Boil the Jerusalem artichoke tubers for 15 minutes and drink the broth warm.
- Boil a glass of oat grains for 60 minutes in a liter of boiling water, cool and drink without restrictions.
- Infuse 10 laurel leaves in 250 ml of boiling water for 24 hours. Drink 50 ml warm before meals for 7 days.
- Fresh blueberries effectively reduce sugar. You can also use its leaves. Brew the leaves with boiling water, leave for two hours and drink 250 ml three times a day for six months.
Effective remedies can be decoctions of burdock roots, bean pods, juniper and eucalyptus. But before using any product, you should consult your doctor.
List of sources
- Demidova T.Yu., Galieva OP Prevention and management of prediabetic disorders of carbohydrate metabolism in patients with metabolic syndrome. “Obesity and Metabolism”, No. 4 (13), 2007; P.19-P.24.
- Nedogoda S.V., Barykina I.N., Salasyuk A.S., Smirnova V.O., Popova E.A. Prediabetes: main causes, symptoms, prevention and treatment//Medicine Bulletin No. 2 (70). 2021. Volume 12.
- Current issues of endocrinology in therapeutic practice: hands. for doctors / Ed. M. N. Kalinkina, L. V. Shpak. - Tver: Factor and K, 2014. - 698 p.
- Pasyeshvili T.M., Koryak V.V. A patient with hyperglycemia at a family doctor’s appointment / Eastern European Journal of Internal and Family Medicine. — 2021.— No. 2.— p. 35-39.
- P.F. Litvitsky, L.D. Maltseva Disorders of carbohydrate metabolism in children: hypoglycemia, hyperglycemia, glycogenosis, aglycogenosis, hexosemia / Issues of modern pediatrics. — 2021.- VOLUME 16/ No. 5 p. 362-368.