Simple contact dermatitis
Simple contact dermatitis is more common than allergic dermatitis. The cause of its occurrence is the toxic effect of irritating substances, leading to the destruction of the epidermis (the outer layer of the skin) and inflammation of the skin. A person encounters most irritating substances on a daily basis - at home or at work. Some of them are weak irritants that cause dermatitis only if there is regular contact with the skin (detergents, cleaners, solvents). Others are caustic substances that can cause dermatitis after single contact (bleach, strong acids, alkalis). No one is immune from simple contact dermatitis.
Who is at risk?
Most often, manifestations of dry dermatitis are observed in the following groups of people:
- in children suffering from atopic dermatitis;
- in older people;
- for allergy sufferers;
- in people who have dry skin from birth.
Advice! With exacerbation of dermatitis, the quality of life is greatly reduced. Most often, dry dermatitis appears on the hands, and seborrhea affects the scalp and face.
Treatment
The goals of treatment by a dermatovenerologist include restoration of the epidermis and its further protection from irritants. For chronic simple contact dermatitis, it is often sufficient to minimize contact with soap and water, use emollients (creams or ointments), and use gloves if the hands are affected. At the acute stage of the disease, it is sometimes necessary to apply glucocorticoid ointments under the bandages. Oral glucocorticoids help suppress acute inflammation, but are not used in the treatment of chronic simple contact dermatitis. It makes no sense to prescribe these drugs if contact with the irritating substance has not been eliminated.
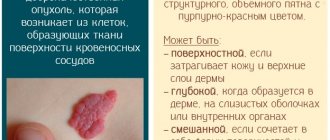
What is this disease?
Dermatitis is a group of skin diseases that arise due to the irritating effects of various environmental factors. Read more about the types of dermatitis in this article.
Dry dermatitis is one of the varieties of this disease, which manifests itself in the form of inflammation in response to physical factors (namely low air temperature). People with dry skin, elderly patients, and those with a tendency to develop allergic diseases are most susceptible to this disease.
Complaints
At the site of contact, severe itching first occurs, and then an itchy rash. Since contact with the allergen and the onset of the disease can be separated in time by two weeks, it is often not possible to determine the date of contact. Chronic allergic contact dermatitis lasts for months or years.
The affected areas may experience redness, swelling, rash, and weeping. The location and location of the rash depends on the cause of the disease. Thus, an allergen contained in decorative cosmetics will damage the face, a nickel ring will damage one of the fingers, and rubber slippers will damage the feet.
Atopic dermatitis, or neurodermatitis
To characterize skin lesions in the form of papular-vesicular rashes, hyperemia, infiltration, dryness, peeling, lichenification, the terms “atopic dermatitis” and “neurodermatitis” are more often used. According to the clinical course, atopic dermatitis is divided into limited and diffuse. For limited atopic dermatitis, the typical localization area is the back of the head, back of the neck, elbow and popliteal folds, forearms, and inner thighs. With limited atopic dermatitis, there are one or two, less often several, lesions. The disease is accompanied by dry rashes; weeping is not typical.
Diffuse atopic dermatitis differs from limited atopic dermatitis in a more widespread process. Sometimes the process takes on a generalized character. Along with vaguely limited brownish-red areas of infiltrated and lichenified skin, which can cover large surfaces, individual flat shiny nodules and multiple excoriations are noted. The skin of patients with diffuse atopic dermatitis is dry. Some patients experience vesiculation and oozing. At the same time, the clinical picture of the disease is dominated by, along with infiltration and lichenification, swelling of the skin, papules, vesicles, erosions and erythema of an acute inflammatory nature. Patients are bothered by incessant itching. Temporary hyperpigmentation of the skin remains in areas of resolved rashes. In diffuse atopic dermatitis, a chronically relapsing course is observed with frequent and prolonged exacerbations. Very often, patients with atopic dermatitis experience respiratory manifestations of atopy: bronchial asthma, rhinoconjunctivitis.
| Along with atopic dermatitis, or neurodermatitis, which is well known to dermatologists, there is severe, generalized atopic dermatitis, which occurs with constant symptoms of eczematization and pyoderma. It is characterized by a combination with atopic diseases of the respiratory tract in the form of allergic rhinosinusitis, conjunctivitis and atopic bronchial asthma. The severe course of the disease often leads to disability. Treatment of these patients seems extremely difficult, due to common drug intolerance |
One of the features of the course of atopic dermatitis is a purulent skin infection, manifested in the form of pyoderma, which is characterized by small pustular rashes that are superficial. Typical for these patients is herpes simplex, which can be localized on the skin of the face, arms, buttocks, and mucous membranes and is capable of migrating to new areas. The predisposition of patients with atopic dermatitis to staphyloderma and herpes infection is considered a clinical sign of immune deficiency. Conjunctivitis in atopic dermatitis is sometimes seasonal and is a manifestation of hay fever, although in most cases it occurs year-round. When cultured from the conjunctiva, Staphylococcus aureus is often identified.
Thus, we can distinguish a syndrome that is characterized by a combination of severe generalized atopic dermatitis with alternating widespread eczematization and pyoderma and respiratory manifestations of atopy. In this case, there is an extremely high level of IgE, sensitization to almost all atopic allergens. The combination of allergic IgE-mediated reactions and immunodeficiency, clinically manifested in recurrent pyoderma, herpes infection and confirmed by the results of an immunological study, is one of the pathogenetic mechanisms for the development of this syndrome. The particular severity of the disease, the young age of the patients, and the ineffectiveness of traditional methods of therapy made it possible to isolate this disease and call it severe atopic syndrome (Yu. A. Poroshina, E. S. Fedenko, V. D. Prokopenko, 1985).
Unfortunately, traditional methods of therapy are not effective enough in the treatment of severe atopic syndrome. Glucocorticosteroids, which have a pronounced anti-inflammatory and antiallergic effect, often lead to steroid dependence and cause a number of severe complications in the form of exacerbations of foci of infection and pyoderma. Exacerbation of pyoderma causes the need for antibacterial therapy, which, as a rule, aggravates atopic dermatitis or is complicated due to the patient's drug intolerance. Due to the ineffectiveness of traditional therapy, the Institute of Immunology of the Ministry of Health of the Russian Federation has developed and carries out methods of extracorporeal immunopharmacotherapy (EIPT, plasmacytopheresis with diuciferon, prednisone and other drugs).
For the period 1995–1997 In the Clinic of Neurosis, 2686 patients were examined who consulted an allergist regarding various itchy skin rashes. Of these, 612 were diagnosed with atopic dermatitis (205 men and 405 women aged 16 to 35 years, average age 22–25 years).
Limited atopic dermatitis was observed in 319 patients, widespread atopic dermatitis in 205, and severe atopic syndrome was detected in 88. The diagnosis was made on the basis of clinical, allergological and immunological examination.
All patients underwent general clinical examination, including functional, laboratory instrumental examination, consultations with specialists (ENT, gastroenterologist, ophthalmologist, etc.).
In addition to a carefully collected allergological, pharmacological and food history according to a specially developed scheme, an allergological examination was carried out with standard domestic sets of household, pollen, epidermal and food allergens and included skin tests - prick or scarification (in patients with severe skin lesions in the forearms, tests were performed on back), provocative nasal and conjunctival tests, as well as the test of inhibition of natural emigration of leukocytes (TTEEL) in vivo according to Ado A.D. with medications.
The immunological examination included the determination of general and specific IgE in the blood serum and the study of indicators of primary immune status: the number of leukocytes, lymphocytes, T- and B-lymphocytes, T-helpers and T-suppressors, immunoglobulins of class A, M, G, as well as neutrophil phagocytosis .
Clinically, skin manifestations were characterized by the presence of papular-vesicular rashes, in some places with hemorrhagic crusts on the surface, severe dryness, widespread erythema, and lichenification. Foci of bright hyperemia, swelling and exudation were noted in the elbow bends and popliteal areas. Subjectively, I was bothered by a painful itch. In 28 out of 88 patients with severe atopic syndrome, pyoderma was observed - superficial pustules with purulent discharge. Pyoderma was widespread in 9 patients, limited in 19, and was combined with furunculosis in 5 patients. 82 people suffered from recurrent herpes simplex.
Table 1. Respiratory manifestations of atopy in 365 patients with atopic dermatitis
| Disease | Number of patients | |
| (in abs). | % | |
| Dust allergic rhinoconjunctivitis | 83 | 23,8 |
| Dust bronchial asthma | 96 | 26 |
| Hay fever (pollen bronchial asthma and rhinoconjunctivitis) | 152 | 42 |
| Combination of dust rhinoconjunctivitis, bronchial asthma and hay fever | 34 | 9 |
| Total | 365 | 100 |
In addition to manifestations of atopic dermatitis and pyoderma, many patients (365) had respiratory manifestations of atopy, which are presented in Table 1.
The majority of patients (427) suffered from concomitant diseases of the gastrointestinal tract (chronic gastritis, peptic ulcer of the stomach and duodenum, dyskinesia of the biliary tract and colon, intestinal dysbiosis, etc.).
In 362 patients, pathology of the ENT organs was identified (chronic sinusitis, polypous ethmoiditis, chronic tonsillitis, chronic subatrophic pharyngitis).
As can be seen from Table 1, a significant number of patients (41%) with atopic dermatitis were diagnosed with hay fever. Half of the patients (49.1%) had respiratory manifestations of household allergies.
During an allergological examination of 612 people suffering from atopic dermatitis, sensitization to non-bacterial allergens was detected in 428 patients. Table 2 presents the results of an allergological examination of these patients according to skin (prick and prick), nasal and conjunctival tests, as well as the determination of specific IgE in the blood serum.
As can be seen from Table 2, the largest number of positive tests were obtained with household and pollen allergens, which, as mentioned above, is due to the presence of not only skin, but also respiratory manifestations of atopy.
Table 2. Results of allergological examination of 428 patients with atopic dermatitis
| Allergens | Number of patients with positive tests | |
| (in abs). | % | |
| Household allergens (house dust, feather pillows, library dust) | 179 | 42 |
| Grass pollen | 63 | 14 |
| Tree pollen | 37 | 8 |
| Pollen of Asteraceae and Chenopodiaceae | 52 | 12 |
| Epidermal allergens (cat, dog, rabbit, sheep, horse dander, human hair) | 42 | 10 |
| Food allergens (milk, fish, egg) | 9 | 2 |
| Combination of different groups of allergens | 46 | 11 |
| Total | 428 | 100 |
105 patients with a history of drug intolerance underwent TTEEL with drugs. In 38 people it was positive.
The clinical course of widespread atopic dermatitis and severe atopic syndrome with relapses of pyoderma and herpes in the presence of chronic foci of infection (chronic maxillary ethmoiditis, chronic tonsillitis, intestinal dysbiosis, etc.) suggested that this category of patients has a combination of allergies and immunodeficiency. An immunological examination revealed the following changes in humoral and cellular immunity: a decrease in the number of peripheral blood lymphocytes due to a decrease in T-cell populations, a decrease in neutrophil phagocytosis. There was an increase in the production of immunoglobulins of class A, M, and especially IgE. In all examined patients, a significant increase in the level of total IgE was recorded, sometimes 10–30 times compared to the level in healthy people.
Along with the term atopic dermatitis, which reflects the allergic nature of this disease, the older definition of neurodermatitis is still widely used (especially by dermatologists). This name was not given without reason, since in almost all patients the exacerbation of the skin process is caused by emotional stress factors and a traumatic situation. In turn, constant itching, which bothers the patient, causes irritability, short temper, and leads to insomnia.
Example
Patient Ch., born in 1972, was in the clinic for treatment from 02/18/93 to 04/29/93 for neurotic depression, severe asthenic-depressive syndrome.
Concomitant diagnosis: atopic dermatitis, a common form in the acute stage (remission at discharge). Hay fever. Allergic rhinoconjunctivitis. Sensitization to tree pollen. Food allergies to nuts, apples, carrots. Chronic gastritis with reduced secretory function. Dyskinesia of the colon.
Complaints of constant itching of the skin, rashes, irritability, short temper, tearfulness, sleep disturbance, headaches, increased fatigue, decreased mood.
From the anamnesis: my grandmother suffered from eczema. My aunt has bronchial asthma. She was born as her first child, on time. According to the mother, pregnancy and childbirth proceeded without complications. From the age of five months she was bottle-fed and almost immediately developed infantile eczema. At the age of five, neurodermatitis was diagnosed. Was observed by dermatologists. There were long periods of relative well-being, when limited dermatitis remained (in the area of the elbow joints, hands). There is always improvement in summer, worsening in September-October. Since 1992, symptoms of rhinitis appeared in May. There was an exacerbation of dermatitis after eating nuts, chocolate, eggs, and citrus fruits. In August 1993, angioedema occurred after eating apples; after that, she did not eat apples. Since childhood, a sharp exacerbation of dermatitis due to stressful situations has been noted. The last deterioration was about a year against the background of a traumatic situation in the family (divorce from my husband). Skin rashes have spread, constant itching bothers me, and sleep has been disturbed because of this. I lost 7 kg in a year. I took suprastin and diphenhydramine with little effect. Local treatment prescribed by a dermatologist (the patient does not know the names of the ointments) gave only short-term improvement.
On admission: general condition was satisfactory. The skin is dry, against the background of areas of hyperemia, multiple scratches, small papular, vesicular scattered rashes, crusts. There is pronounced lichenification in the neck, elbow joints, and wrists. There is no swelling. There are no symptoms of rhinitis or conjunctivitis. The mucous membrane of the oral cavity and pharynx is not changed. There is vesicular breathing in the lungs, no wheezing. Heart sounds are clear, rhythmic, blood pressure is 110/70. Pulse 88 per minute, satisfactory properties. The abdomen is soft, painless in all parts. The liver is not enlarged. There is no dysuria. Stool is not regular, tendency to constipation. Asthenized. The mood is low. Fixed on her condition and on the traumatic situation in the family.
Results of clinical and laboratory examination: class. an. blood – HB-124, L-5.0; p.1, p.46, e.12, l.36, m.5, soe-8 mm/hour. Biochem. an. blood: total protein 80.0; urea 4.4; creatinine 89.1, cholesterol 6.1; beta lipoproteins 6.1; bilirubin total 14.8; ALT–0.25; AST-0.34; glucose 4.7; seromucoid 0.10. SRB - negative, Wasserman district negative.
An. urine – without features.
ECG: without pathology.
X-ray of the PPN - the transparency of the sinuses is not impaired.
EGDS: gastritis, duodeno-gastric reflux.
Cons. ENT: healthy.
Cons. gynecologist: healthy
Cons. gastroenterologist: chronic gastritis with reduced secretory function. Dyskinesia of the colon.
Cons. neurologist: vegetative-vascular dysfunction of the hypotonic type.
Immune status: L:5.0; Lf-36%, - 1.9; phagocytosis 74%, Tlf-61%-1.1; Vlf 5% -0.09; IgA 230, IgM 110, IgG 1400, IgG-tot. more than 1000.
Allergological examination: scratch tests are positive with allergens from birch pollen +++, alder +++, hazel +++, oak ++, ash ++, poplar +, with epidermal and household allergens – negative. Certification tests with food passive allergens - nuts (walnuts, hazelnuts, almonds, peanuts), carrots, apples (Starkin, Golden) - positive. Testing was carried out on the back.
Treatment: individual hypoallergenic diet, IV drip of Dexon 8 mg per person. r-re, two days; IV drip Dexona 4 mg. On physical solution – 3 days, total 28 mg; IV drip Ascorbic acid 5.0 per physical. solution 5 days; zaditen 1 t. x 2 times, festal 1 t. x 3 times during meals, intal 2 drops. x 3 times (dissolved in water) in 20 minutes. before meals, activated carbon 1 t. x 3 times 1.5 hours after meals; IV drip tavegil 2.0 for physical solution - 2 days, tavegil 2.0 IM at night - 5 days, retabolil 1 t. at night, local skin treatment with celestoderm ointment and Unna ointment, physiotherapy (electrosleep, ultraviolet irradiation), acupuncture, complex psychotherapy, therapeutic relaxation gymnastics, group and individual sessions with a psychologist. HBOT – 5 sessions.
As a result of the treatment, pronounced positive dynamics were noted: the skin rashes completely disappeared, lichenification remains in the area of the elbows and wrists, and there is almost no itching. Sleep returned to normal. I became calmer, more cheerful, more active. My mood has improved.
Recommendations given upon discharge:
- Observation of an allergist at the place of residence.
- Following a hypoallergenic diet with the exception of apples, nuts, honey, carrots, stone fruits, and histamine-liberating products.
- Continue taking zaditen 1 t. x 2 times, topically Unna cream.
- In May, it is advisable to travel to a different climate zone.
- Herbal medicine, penicillin drugs, nicotinic acid, B vitamins, and radiocontrast agents are not indicated.
- Avoid contact with dust and household chemicals.
- Frequent change of underwear and bed linen.
- Before surgery, premedication: IV or IM Dexon 8 mg, IM Tavegil 2.0; honey. vaccinations only for health reasons and with the same premedication.
Treatment
For rashes and weeping, lotions with aluminum acetate (Burow's liquid) help. After the affected areas of the skin have dried, glucocorticoids are prescribed for external use. In severe cases, H1 blockers (antihistamines) and oral glucocorticoids are required. For cure, it is important to identify and eliminate the allergen, but this often requires application tests. Patch tests are especially useful for those patients who come into contact with many chemicals at work.
Why does this disease occur?
As mentioned above, the main cause of this disease is exposure to cold air on the skin. However, other reasons are also important and may act as predisposing factors. These include:
- heredity (a tendency to develop dermatitis, not necessarily dry dermatitis, can be transmitted from parents to children);
- dry air (if not only the air temperature decreases, but also its humidity, the risk of developing the disease increases several times);
- stress (emotional stress plays a big role in the development of all types of dermatitis);
- various agents that cause allergic reactions: fluff, dust, cosmetics and household chemicals, fungi, food allergens (these factors can negatively affect the condition of the skin, aggravating the course of the disease);
- chronic diseases of the digestive, nervous, immune, endocrine systems.
Dermatitis (dry) is a multifactorial disease, therefore, for effective treatment and prevention it is necessary to exclude all possible causes that could cause this condition.
Forms
Dermatitis can occur in several forms:
- acute;
- subacute;
- chronic.
The acute form of dry dermatitis is accompanied by severe symptoms. It is characterized by an increase in body temperature and the occurrence of unbearable itching and burning of the skin.
The subacute form of the pathology is characterized by the formation of pustules or papules filled with clear liquid and prone to spontaneous opening.
In the chronic form of the pathological process, the severity of the clinical picture is not so bright. However, with such dermatitis, treatment is more protracted. In addition, it is impossible to completely eliminate the risk of relapse, and stopping the pathological process will be much more difficult.
Inexpensive ointments and creams for dermatitis
Below are advertised expensive medications for dermatitis, as well as their cheaper and inexpensive analogues.
| Expensive drugs | Price, rub) | Available analogues | Price, rub) |
| Lokoid | 300 | Hydrocortisone ointment> | 30 |
| Bepanten | 750 | Dexpanthenol | 150 |
| Celestoderm | 320 | Betaderm | 130 |
| Advantan | 650 | Metipred | 200 |
| Elokom | 400 | Momat | 140 |
| Skin Cap | 900 | Pyrithione zinc | 600 |
| Exoderil | 800 | Fungoterbin | 350 |
Before purchasing an analogue, you should carefully read the instructions for use and consult your doctor.
How to distinguish psoriasis from seborrheic dermatitis?
Diseases are often confused. Although both diseases share common features, they also have many differences. Common characteristics include a chronic type of disease and an undulating course, the presence of rashes, itching, and peeling of the skin. What is the difference between psoriasis and dermatitis?
- Prerequisites for development. If psoriasis appears under the influence of autoimmune, endocrine, and genetic disorders, then seborrheic dermatitis is caused by increased activity of the sebaceous glands and yeast-like fungi.
- Symptoms. Despite the fact that in both cases the skin is covered with scales, their structure and appearance are different. When oily yellow crusts appear, we are talking about seborrheic dermatitis, and when dry gray, white or silvery scales form, psoriasis can be diagnosed.
- Localization. Psoriasis can affect almost all areas of the skin, and seborrheic dermatitis is localized mainly on the scalp, neck and face.
If you experience skin rashes that could be a sign of both dermatitis and psoriasis, be sure to consult a dermatologist. Usually, a qualified doctor can determine what it is by the external manifestations of the disease. If mixed symptoms occur, the dermatologist will write a referral for additional examinations.
Prevention
Specific prevention has not been developed. To reduce the likelihood of this disease occurring, you need to protect your skin from cold air, use moisturizers, follow a hypoallergenic diet, avoid stressful situations, and also constantly monitor your health. To improve the condition of the skin, it is recommended to drink vitamins A, group B, C, E.
Dry dermatitis is an unpleasant disease, but curable. If you consult a doctor in time and make efforts to cure, you can forget about the unpleasant symptoms of this disease forever!
Alarming symptoms and diagnosis
The skin is the largest human organ, which is exposed to the maximum number of external influences. Is “something strange” that appears on the skin always atopic dermatitis? Certainly not.
Characteristic signs of AD:
- itching of varying intensity;
- dry skin + peeling + redness;
- rashes: spots and blisters in the primary lesion; scales, crusts, erosions, cracks, thickening and hardening of the skin (lichenification), skin discoloration (hypopigmentation) - with relapses;
- localization – AD most often affects certain areas of the skin.
Atopic dermatitis can be localized on any part of the face, trunk and limbs. In the absence of timely diagnosis and adequate treatment, the disease can affect a large surface of the skin. The progression of atopic dermatitis significantly increases the risk of developing bronchial asthma, respiratory allergies and other diseases.
Which specialist should I contact if I have alarming symptoms? Dermatologist/dermatovenerologist + allergist. A preliminary diagnosis can be made based on examination, medical history, and family history. To confirm the diagnosis, as a rule, the following is prescribed:
- general blood analysis;
- biochemical blood test, including determination of the concentration of immunoglobulins E in the blood;
- analysis for allergen-specific antibodies;
- additional studies - as indicated.
Red dermatitis, also known as lichen planus
This is a chronic itchy skin disease, which is accompanied by the appearance of pink-red-violet rashes, merging into large plaques, up to 10 cm in size, with the formation of garlands and rings.
Locations: the lateral part of the body, the inner surface of the arms in places of flexion, mucous membranes of the mouth and genitals.
There are several forms of damage to the skin and mucous membranes. Manifestations of the disease are very diverse: papules, spots, erosions, blisters, etc.
Complications
If left untreated, dermatitis can become more complicated:
- skin hyperpigmentation;
- the formation of scars at the site of the rash;
- development of dyschromia;
- atrophy of skin tissue;
- the addition of a secondary bacterial infection.
The danger of the pathology also lies in the fact that some of the above anomalies can be combined with each other, which leads to the need for long-term treatment and a significant decrease in a person’s quality of life.
Consumer Reviews
Prikhodko.Angelina (vseotzyvy.ru)
“After giving birth and breastfeeding, apparently something changed in my body - if before everything was ok with my hair and scalp, now it’s just a disaster - it itches terribly, my hair has become dry, the ends are split, I don’t have time to cut them. I tried folk remedies - all kinds of masks, and store-bought ones - all to no avail, until I came across La-Cri shampoo for dry and sensitive scalp. At first I liked the composition - it does not contain sulfates, hormones, which are harmful to the skin and body, but contains panthenol, bisabolol, violet and licorice extracts, keratin. And the shampoo did not disappoint even after use - after the first wash, the skin stopped itching and flaking. I’m used to washing my hair every day, with this shampoo it’s possible, but it’ll only be better. I’ve been using it for the second month, despite the sun, the skin on my scalp has completely forgotten what itching is, my hair has stopped falling out and while I’m in no hurry to go to the hairdresser for a trim, the ends of my hair are not split, although two months have definitely passed since the last haircut. This shampoo is also good because it can be used by children as young as 3 years old, and soon I will be able to wash my daughter’s hair with it too.”
Elena (wildberries.ru)
“The shampoo is good. Thick. The smell is pleasant. Well moisturizes the scalp. Hair shines after washing. It suited me. I will buy more products from this series. Well packaged.”
Sources:
- Andropova T. V., Gudina M. V., Odintsova I. N., Hygiene of children and adolescents, Siberian State Medical University Publishing House, 2021.
- Cohen Bernard A. Pediatric dermatology, MEDpress-inform, 2015.
- Sukolin Gennady Ivanovich, Illustrated clinical dermatology. Brief alphabetical reference book, Lux Print publishing house, 2010.
- Kildiyarova Rita Rafgatovna, Pediatrician for every day. Guide for doctors, GEOTAR-Media, 2021.
Photos of dermatitis
Localization of lesions in dry dermatitis
The most vulnerable areas of the skin are those with the fewest sebaceous glands, as well as parts of the body that are most often in contact with cold air. Symptoms of the disease are often localized in the following areas of the body:
- feet;
- palms;
- knees;
- elbows.
These are the most typical places for manifestations of the disease to occur, but other areas of the skin may also be affected. Sometimes the lesion occurs on the head, stomach, or back. You can read about dry facial dermatitis in this article.
Antipruritic ointments
Dermatitis is always accompanied by itching. It can be of varying degrees of severity. With intense itching, patients become nervous, lose peace and sleep. Stress only worsens the course of dermatitis. Therefore, in such situations, it is important to alleviate the condition of patients with the help of antipruritic drugs.
For this purpose, external antihistamines (Fenistil gel for dermatitis) and calcineurin inhibitors (Protopic, Elidel) are used. These drugs stop inflammation and have an anesthetic effect, thereby reducing skin itching. A menthol-based ointment for dermatitis on the skin (Boromenthol, Menovazan) has a similar effect. It cools and soothes inflamed skin, reduces the sensitivity of receptors, as a result of which the affected area stops itching for some time.
As mentioned above, hormonal antipruritic ointment for dermatitis has a faster and more effective effect. But it is still better to start treatment with non-hormonal ointments due to the low risk of side effects and a small list of contraindications.
Treatment of seborrheic skin lesions
The main ointment for seborrheic dermatitis is antifungal: Ketoconazole, Nizoral, Sebozol, Nizorex, Mycozoral.
It is recommended to treat the affected skin with keratoregulating agents (for example, Mustela Stelaker). In special cases, Sulsena paste and hydrocortisone ointment are added, but preference in the treatment of this type of dermatitis is given to physiotherapeutic methods.
Remedies for atopic dermatitis
Therapy for atopic dermatitis begins with the use of non-hormonal agents. These are Gistan, Fenistil, Eplan, Radevit. If the severity of clinical manifestations does not decrease within several days, the therapeutic regimen is adjusted.
It is replenished with hormonal agents:
- Cutivate;
- Akriderm;
- Momatom;
- Beloderm;
- Celestodermos.
Cheap ointments for dermatitis (Prednisolone, Hydrocortisone) are effective only for minor rashes. Papules, vesicles, blisters can usually be eliminated with expensive means, for example, Cutivate.
After the rash disappears, patients are prescribed products with dexpanthenol to accelerate skin regeneration. If the course of the pathology is complicated by infection, the use of drugs with a combined composition is recommended - Akriderm GK, Triderm.