Duodenal ulcers often begin gradually with sucking pain in the pit of the stomach, an increased feeling of hunger in the morning, and mild nausea.
But just as often, these signals that the body gives are not taken seriously. The person simply does not realize the scale of the impending problem. After all, persistent pain syndrome, as well as dangerous complications of this disease, develop much later.
If there is the slightest doubt about the presence of the disease, you should immediately contact a therapist or gastroenterologist with complaints, so as not to end up with a surgeon or, God forbid, a pathologist.
To help you navigate the variety of manifestations of duodenal ulcer, this article collects and highlights the main issues related to this disease.
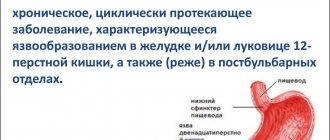
What is an ulcer?
The wall of the duodenum, which is called duodenum in Latin, consists of mucous, submucosal and muscular layers. An ulcer is a wall defect, the bottom of which is located in the muscle layer, that is, the mucosa and submucosa are destroyed.
In the duodenum, the ulcer is most often located in the initial section (bulb or bulb), since here are the most favorable conditions for the reflux of acidic gastric contents and a wonderful place for the proliferation of bacteria that provoke peptic ulcer disease. Sometimes not one ulcer of the duodenal bulb is formed, but several at once. More often these are paired, opposite each other, “kissing” ulcers.
Peptic ulcer disease is the repeated formation of ulcerative defects in the wall of the duodenum, occurring with periods of exacerbation (the presence of an ulcer) and remission (the absence of an open defect in the intestinal wall). Since the ulcer heals with the formation of a scar, even in remission, scar defects remain on the mucous membrane. If exacerbations are frequent and a lot of scars are formed, they can deform or narrow the intestinal lumen.
About ten percent of the world's population suffers from duodenal ulcers. These are predominantly young and middle-aged people.
Diet recipes
During different periods of the disease, the cooking technology differs. If mucous soups are recommended for severe inflammation (they are used in Diets 1A and 1B ), then pureed soups are the basis of Table No. 1 and are recommended during the recovery period.
Mucus soups are the most gentle and are strained decoctions of cereals (without the cereals themselves), which are salted and butter is added (sometimes seasoned with an egg-milk mixture). When preparing pureed soups, all ingredients are pureed, the soup is salted and oil is added while it is warm. Cereal milk soups are prepared in the same way (the ratio of water and milk is 1:1, the cereal is pureed). Below are the recipes for the first table dishes.
First meal
Milk soup with turkey meat and croutons
Boiled turkey meat is passed through a meat grinder and further pureed to a puree. The broth (oatmeal or rice) is mixed with puree, salted to taste and boiled. After cooling to 80°C, season with milk and cream (1:1). Additionally, you can add a beaten egg and bring to a boil.
Pumpkin and cauliflower soup
Place the vegetables in a saucepan, add a small amount of water and boil. When warm, rub together with the broth. Prepare a white sauce based on milk, flour and eggs. White sauce is added to the vegetable puree, salted, diluted with milk or vegetable broth to the desired consistency and brought to a boil. You can add a piece of butter to the finished soup.
Second courses
Fish pudding with green peas
The fish fillets are boiled and wiped. Add butter, egg yolks, mix well and salt. Add whipped whites to the prepared fish mixture in several additions, stirring gently. The mass is poured into a mold and steamed.
Beef soufflé
The boiled beef is minced several times. Milk sauce, butter, egg yolks and salt are added to the finished meat puree. Beaten egg whites are added to the resulting mass. Place in a mold and steam.
Dessert
Apple and carrot pudding
Sliced carrots are simmered in a saucepan with a small amount of water. After 10-15 minutes, add chopped apples and simmer until everything is ready. The mass is rubbed, milk and semolina are added, and boiled for 1-2 minutes. Separately beaten yolks and whites are added to the cooled mass. Place in a mold and bake in a slow cooker or oven without forming a rough crust.
Why does she appear?
There is no single view on the occurrence and development of duodenal ulcers. There are several equivalent theories of the occurrence of ulcers.
- On the one hand, several years ago there was a very popular assumption that peptic ulcer disease is the result of the colonization of the stomach and intestines by a microbe such as Helicobacter pylori. The microbe infects cells that secrete mucus. During development, it quickly colonizes the stomach and duodenum, stimulating the release of gastrin and releasing cytokines (substances that damage cells). Later it turned out that not all types of this microorganism living in humans cause disease. Therefore, blaming everything on infection is still wrong.
- An earlier assumption was an imbalance between the ability of the mucous membrane to defend itself and aggressive factors in the form of gastric acid and pepsin, which enter the intestine when the function of the obturator muscle of the gastric outlet is insufficient. It was also believed that the intestine was scratched by rough food. Today, these assumptions have been supplemented by the fact that a decrease in protective prostaglandins has been found in the mucous membrane of patients with peptic ulcer disease.
- A relationship has been found between the incidence of ulcers and blood type. Carriers of the first group with a Rh-positive factor are at greater risk.
- Soviet physiology was of the opinion that ulcers develop in people with excessive irritation of the cerebral cortex against the background of chronic stress or nervous experiences, when the release of gastric juice and inflammatory mediators (gastrin) is stimulated through the autonomic nervous system.
- Another interesting conclusion is associated with gastrin: prolonged exposure to the sun stimulates the release of this hormone and, accordingly, provokes an exacerbation of peptic ulcer disease or worsens its course.
- Taking medications such as corticosteroids and non-steroidal anti-inflammatory drugs can provoke ulcerations of the intestinal mucosa.
- Alcohol and nicotine worsen the condition of the mucous membrane, change the nature of the secretion of hydrochloric acid and pepsin by the stomach, affect the level of gastrin and somatostatin, and also reduce the protective properties of the mucus. Alcohol directly damages mucosal cells.
Fully or partially limited products
- Products that increase secretion (broths, pickled vegetables, smoked and fried foods, alcoholic drinks, strong coffee and tea, carbonated drinks, spicy dishes, high-acid dairy products, sour fruits).
- Shchi, okroshka and borscht are excluded from the first courses.
- It is envisaged to exclude vegetables with coarse fiber (radish, turnip, cabbage, rutabaga, beans, peas), fruits with peel, and mushrooms, as a difficult-to-digest product. It is not allowed to consume sorrel, fresh dill, parsley and onions, as well as spinach due to the high content of organic acids and irritating essential oils.
- Products with connective tissue (skin, cartilage, veins).
- Irritating foods and dishes (cranberries, citrus juices and sour fruits, tomatoes, onions, peppers, garlic, ginger, chocolate, horseradish, mustard, meat sauces, tomato sauce, pepper).
- Pickled and pickled vegetables, canned vegetables - these products cause an increase in secretion.
- For a long time, difficult-to-digest cereals are excluded: millet, pearl barley, barley and corn.
- Legumes, fresh bread, kvass, yeast baked goods, which increase gas formation.
- Prohibited: fatty pork, animal fats, fatty fish, duck, lamb, goose, canned meat, canned fish and smoked meats.
- Fried and hard-boiled eggs, as they are difficult to digest and absorb.
- Any fresh bread, butter and puff pastry.
- Dried fruits and ice cream.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| sauerkraut | 1,8 | 0,1 | 4,4 | 19 |
| green onion | 1,3 | 0,0 | 4,6 | 19 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| canned cucumbers | 2,8 | 0,0 | 1,3 | 16 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| turnip | 1,5 | 0,1 | 6,2 | 30 |
| canned tomatoes | 1,1 | 0,1 | 3,5 | 20 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
Cereals and porridges | ||||
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
Confectionery | ||||
| candies | 4,3 | 19,8 | 67,5 | 453 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Cakes | ||||
| cake | 4,4 | 23,4 | 45,2 | 407 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| ginger | 1,8 | 0,8 | 15,8 | 80 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| ground black pepper | 10,4 | 3,3 | 38,7 | 251 |
| chilli | 2,0 | 0,2 | 9,5 | 40 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| ham | 22,6 | 20,9 | 0,0 | 279 |
Sausages | ||||
| dry-cured sausage | 24,1 | 38,3 | 1,0 | 455 |
| sausages | 10,1 | 31,6 | 1,9 | 332 |
| sausages | 12,3 | 25,3 | 0,0 | 277 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Non-alcoholic drinks | ||||
| bread kvass | 0,2 | 0,0 | 5,2 | 27 |
| * data is per 100 g of product | ||||
What are the symptoms of a duodenal ulcer?
The symptoms of stomach and duodenal ulcers are very close to each other. These are: pain, heartburn, nausea, vomiting, appetite disorders.
- Pain
With ulcers, the duodenum is called late. They occur an hour and a half after eating. Hunger pains that occur if food has not been received for more than 4 hours are also characteristic. A type of such pain is night or early morning, similar to very acute hunger and sucking in the right hypochondrium. The nature of pain may vary from patient to patient. There are stabbing, aching, cutting, sucking or spasmodic pains of varying intensity and duration. In this case, the pain is located in the right half of the epigastric region (bulb ulcer). They can radiate to the right hypochondrium or to the back. With an ulcer located at the end of the intestine, the pain shifts more to the midline of the epigastrium or to its left half. The basis of the pain is a violation of the integrity of the intestinal wall, inflammation and accumulation of under-oxidized metabolic products.
- Heartburn
accompanies about a third of duodenal ulcers. It is due to the fact that the acidic contents of the stomach are thrown into the esophagus against the background of impaired motor activity of the stomach and intestines and inflammatory changes in the mucous membrane.
- Nausea and vomiting
eaten food or gastric contents are characteristic of high duodenal ulcers. With the development of secondary inflammation of the pancreas or gallbladder against the background of a peptic ulcer, vomiting of bile may occur.
- Appetite disorders
can manifest itself as an increase (sucking in the stomach is somewhat smoothed out by food intake) or an aversion to food and fear of it, since in the presence of an ulcer, food can provoke pain.
Symptoms
| Occurrence (how often a symptom occurs in a given disease) | |
| Bloating (flatulence, swelling, tympany, increased gas formation) | 90% |
| Acute pain in the epigastric region and a feeling of fullness and burning in the stomach | 90% |
| Heartburn | 80% |
| Constipation | 70% |
| Frequent loose stools (diarrhea, diarrhea) | 70% |
| Reducing heartburn after drinking milk | 60% |
| Vomiting of various types, including indomitable | 20% |
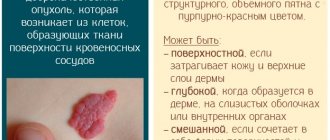
Complications of peptic ulcer
If the ulcer is not detected and treated in a timely manner, it may heal on its own. However, there is a high risk of developing a number of complications, which not only aggravate the course of the disease, but complicate treatment and worsen the prognosis for the patient. All complications are divided into:
Destructive - destroying the intestines:
- it's bleeding
- perforation - perforation
- penetration - penetration into a neighboring organ
Dysmorphic complications that change its structure:
- malignancy - the development of a malignant tumor at the site of the ulcer
- cicatricial deformation - a change in the structure of the walls and narrowing of the intestinal lumen until it is completely closed due to scars from ulcers.
Ulcers located on the anterior wall of the intestine are more likely to perforate. Ulcers of the posterior wall often penetrate the head of the pancreas.
Etiology
Varieties by reason of origin:
- due to stress factors;
- after exposure to medications;
- against the background of endocrine disorders;
- caused by diseases of internal organs.
Based on the morphology of damage, they are divided into:
- erosive damage;
- acute ulcer;
- chronic.
According to the number of damage to the mucous membrane, ulcers are divided into:
- single (from one to three damages);
- multiple (more than three).
They are classified according to the size and area of damage:
- small (less than half a centimeter);
- medium size (from half a centimeter to one centimeter);
- large (size from one to three centimeters);
- huge (more than three centimeters in diameter).
A type is acute duodenal ulcer (stress ulcer).
It is characterized by:
- first time diagnosed;
- acute onset;
- occurrence on a nervous basis.
Bleeding from the duodenum
Physical work and heavy lifting can provoke bleeding. But most often the cause is alcohol intake, if treatment with medications is not carried out or is inadequate. Therefore, up to 80% of this complication occurs in men. In this case, blood loss can be of different volumes.
When bleeding occurs, tar-colored stools or vomit with a color similar to coffee grounds appear. Minor bleeding may only result in diarrhea or pasty, dark stools. At the same time, with heavy blood loss, vomiting will be accompanied by rapidly increasing weakness, dizziness and even loss of consciousness. Bleeding is an emergency that requires calling an ambulance or going to a hospital emergency room on your own.
Risk factors for developing the disease
Develops against the background:
- poor nutrition;
- fast food abuse;
- consumption of alcoholic beverages;
- smoking;
- uncontrolled use of medications that burn the mucous membrane of the digestive system;
- hereditary factor;
- H. Pylori infection;
- chronic obstructive pulmonary disease;
- cirrhosis of the liver;
- renal failure;
- strict diets with complete absence of food for a long time;
- physical overload;
- chronic stress and depression;
- autoimmune dysfunctions.
Symptoms of a perforated duodenal ulcer
Perforation of an ulcer means not only bleeding, but also the entry into the abdominal cavity of the contents of the duodenum, where pancreatic enzymes and bile are released. These are quite aggressive substances that quickly cause irritation of the peritoneum and lead to inflammation of the abdominal cavity (peritonitis).
If acute stabbing pain in the abdomen occurs against the background of a peptic ulcer, you should immediately call an ambulance. This pain appears more often in the right half of the epigastric region and can radiate to the right shoulder or scapula. The pain is so severe that the patient takes a forced position, lying on his side or back with his legs brought to his stomach. At the same time, the skin becomes very pale. The abdominal muscles tense, the person avoids any movement.
The most dangerous period is the period of imaginary well-being, which develops a few hours after the onset of perforation. Here the pain subsides somewhat, the patient begins to move and assures that he is feeling better. During this period, patients often recklessly refuse surgery that could save their life. But, if 6-12 hours pass from the onset of perforation, and the patient does not undergo surgery, his condition will sharply worsen:
- vomiting appears
- temperature increase
- the pain will return
- bloating will appear
- pulse and heartbeat increase
- peritonitis will develop, which will need to be operated on, and the prognosis for which at this stage is already worse.
Reviews and results
This dietary food is prescribed for a long period, since it is balanced, and the diet is significantly expanded compared to Diets No. 1A and 1B . This allows you to eat a varied diet without feeling deprived. Reviews from patients indicate the positive impact of such nutrition on the gastrointestinal tract: pain, belching, heartburn , bitterness in the mouth disappear, and intestinal bloating does not bother you. For some, pain in the pancreas and bowel disorders associated with pancreatitis disappear.
- “...I have had duodenal ulcer for many years. When it was first detected, I was treated well in the hospital, after which there were no exacerbations, and if there were, they were not severe and without the formation of a “new ulcer.” It’s just that in the fall or after nervous stress, sucking pain appears in the stomach area. This is a signal that you need to drink De-nol, Lansoprozole for 2 weeks and switch to proper nutrition. In such cases, I manage without a hospital. I maintain the diet well for 3-4 weeks, and then I switch to regular food, but without spicy, smoked or fried foods. I like steamed cutlets made from different types of meat and poultry - they are not completely tasteless, since my wife adds a little grated onion and dried dill to them (this does not cause pain or other discomfort). I eat soups in water without spices or frying. These are mainly cereal soups with well-cooked or crushed cereals. I eat all the cereals, mashed potatoes, and pureed vegetable supplements. Already in the second week the stomach calms down. In a month of eating this way, I lose a little weight”;
- “... Several years ago there was a perforated ulcer, but it was not very complex, so we operated on it using the endoscopic method. I recovered quickly after this operation, but I had to follow the diet for a long time, and I also took medication for about a month. At first I ate everything pureed for a month, and then I switched to the first table that was not pureed. I adhered to it very strictly for six months, although after a month nothing bothered me, and only 3 scars reminded me of the operation. During these six months, I got used to cooking dishes in a double boiler and a slow cooker, added new recipes to the list, and the food did not seem monotonous and boring. The dietary restrictions affected my weight—I lost 5 kg. I hope to continue to adhere to a healthy diet - the perforation really scared me”;
- “...Frequent exacerbations of ulcers occur once every two years. I think this is due to smoking, irregular meals (and even dry food) and business trips. It is clear that far from home there is no opportunity to eat properly. So it turns out that I periodically end up in the hospital. There they immediately assign Table 1B, and after 2 weeks - the main table for stomach patients.”
Cicatricial stenosis of the duodenum
If exacerbations of duodenal ulcer follow one after another or the ulcerative defects are very large and deep, scars from ulcers can significantly deform or narrow the intestinal lumen. In this case, problems arise with the passage of food, and a narrowing (stenosis) of the intestine develops, which requires surgical treatment. Clinically, decompensated stenosis is manifested by vomiting, impaired passage of food and distension of the stomach. At the same time, disturbances in the content of salts and water in the body develop, which lead to lethargy, weakness, drowsiness, increased muscle tone, and a feeling of goosebumps running on the skin of the arms and legs.
Diagnostics
Today, the main and most informative method for identifying peptic ulcers is FGDS (fibrogastrodudenoscopy), in which, by inserting an endoscope (optical probe) into the stomach and duodenum, you can see the ulcer, assess its size and depth, and take the mucous membrane for examination (biopsy). or conduct a rapid urease test for the presence of Helicobacter pylori.
X-ray diagnostics, which is indispensable in clarifying complications, is of auxiliary importance.
Patients are also prescribed a clinical blood test, blood biochemistry, and a stool test for the Gregersen reaction (detection of occult blood).
Diagnostic measures
To make a diagnosis, the doctor needs to interview the patient, identify complaints that bother the patient, the circumstances under which they arose, and the duration of the symptoms. In addition, a number of instrumental and laboratory studies will be required:
- X-ray and fibrogastroscopy to assess the condition of the tissues of the stomach and intestines and detect lesions. Determination of their location and size;
- Blood test for hemoglobin level to detect internal bleeding;
- Examination of stool to determine the presence of a bleeding ulcer;
- Study of gastric juice for hydrochloric acid content to determine the possible cause of the development of the ulcerative process.
Treatment of duodenal ulcers
With timely detection of duodenal ulcer in the acute stage, treatment is reduced to the prescription of conservative therapy (prescription of tablets, less often injections or drips). The times when surgical treatment methods were used for uncomplicated peptic ulcers are a thing of the past. If the peptic ulcer is complicated, then hospitalization in a surgical hospital is mandatory, and refusal to do so can be fatal. This does not mean that any bleeding will be operated on, but timely observation is indicated for every complicated duodenal ulcer.
Previously, it was customary to carry out seasonal (spring and autumn) preventive treatment of duodenal ulcer. Currently, this practice is not supported, as it has not brought the expected results. Treatment is prescribed for the period of exacerbation of duodenal ulcer.
Prevention
Prevention of duodenal ulcer has 2 goals: preventing increased secretion of hydrochloric acid and preventing infection with Helicobacter pylori infection.
In order to prevent an increase in hydrochloric acid, it is necessary to give up alcoholic beverages and smoking, eliminate neuro-emotional stress, while eating, exclude from your diet foods that increase acidity (spicy, salty, fried). In order to prevent infection with Helicobacter pylori infection, it is necessary to use clean utensils (do not drink from a cup after someone else, do not use someone else’s spoon or fork, even with your family), since this infection is transmitted through the saliva of an infected person.
In the presence of chronic gastritis and/or duodenitis, their timely drug treatment and diet therapy.
Diet for ulcers
In case of duodenal ulcer, a 4g diet is prescribed for the period of exacerbation, which involves mechanical, chemical and temperature sparing. It is recommended to eat 5-6 meals a day in small portions. Food should be heated to a temperature of 36-37 degrees. Hot, cold and dry foods are excluded (see what you can eat with gastritis). Alcohol and smoking on an empty stomach are prohibited.
- Preference is given to boiled, pureed food. Slimy porridges, non-rich creamy soups, mashed potatoes, pasta, rice and buckwheat are desirable. Steamed fish, poultry, boiled meat in the form of soufflé or minced meat and cutlets. Watermelons and bananas are allowed as fruits.
- You will have to give up fried, spicy, rich meat and bone broths, marinades, soda, strong tea, coffee, and yeast baked goods. The greatest harm is caused by fruits and vegetables containing fiber. You will have to forget about tomatoes, cucumbers, apples, pears, cabbage, carrots, radishes and other garden delights until the ulcerative defect heals.
- It is strictly forbidden to chew gum, which stimulates gastric secretion.
- Milk in this situation becomes an ambiguous product. In some patients, whole milk can irritate the ulcer due to calcium ions, while others drink it with pleasure, as it significantly reduces heartburn.
For more details, see Diet for duodenal ulcers, list of products, menu.
Authorized Products
Diet for duodenal ulcer includes:
- Soups that are prepared with potato broth or a decoction of prefabricated vegetables. At first they add pureed vegetables and cereals (semolina, buckwheat, rolled oats, rice), and then switch to non- pureed ones. The first courses add pureed meat, an egg-milk mixture and a little butter. Milk cereal soups and noodle soups are allowed.
- Use lean dietary meat (beef, veal, young lamb, chicken, rabbit and turkey). Prepare steamed and boiled dishes (cutlets, dumplings, puree, soufflé, meatballs, zrazy). A month after an exacerbation or surgery, meat baked in the oven is allowed.
- Lean fish is steamed or baked without crust. The skin is removed, the fish can be cooked in pieces or chopped (cutlets, meatballs, meatballs, zrazy).
- Porridges are cooked in milk or water from rice, semolina, buckwheat or oatmeal; you can also use vermicelli. The porridge needs to be boiled well and kneaded a little, the buckwheat should be rubbed first. You can make puddings and casseroles from cereals with the addition of cottage cheese.
- Vegetables with low fiber content (potatoes, beets, pumpkin, zucchini, carrots, green peas, cauliflower). They are steamed and served pureed. By adding whipped whites and semolina to the puree and steaming the mixture in molds, you get a vegetable soufflé.
- Pumpkin and zucchini can be eaten ungrated, as they are the most delicate vegetables. To improve the taste, chopped dill can be added to vegetable purees and soups.
- Small amounts of butter and vegetable oils are used to season ready-made dishes.
- Wheat bread (stale or dried). The diet can be expanded by introducing low-fat biscuits and dry cookies. It is not often possible to eat baked savory pies with different fillings (apples, jam, cottage cheese, meat, fish).
- Milk and cream, non-acidic yogurt and kefir are added. Non-acidic fresh cottage cheese can be eaten in its natural form or made into cheesecakes, puddings, and lazy dumplings. Mild cheese can be introduced infrequently.
- Two eggs, eaten every other day, cooked as a steam omelet or soft-boiled.
- Expanding the diet allows you to switch to an untreated table, on which you are allowed to eat a salad of boiled vegetables with meat or fish, jellied fish, herring and sturgeon caviar.
- Desserts steamed from pureed berries, purees, jelly, jelly, sambuca, compotes. Sweet berries and fruits can be consumed baked or boiled. You can eat milk jelly, non-sour jam, meringues, marshmallows, marshmallows and honey. Drinks allowed are fruit juices, rosehip infusion, weak coffee with milk, tea with milk/cream.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Fruits | ||||
| apricots | 0,9 | 0,1 | 10,8 | 41 |
| watermelon | 0,6 | 0,1 | 5,8 | 25 |
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
| nectarine | 0,9 | 0,2 | 11,8 | 48 |
| peaches | 0,9 | 0,1 | 11,3 | 46 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| strawberry | 0,8 | 0,4 | 7,5 | 41 |
| raspberries | 0,8 | 0,5 | 8,3 | 46 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| noodles | 12,0 | 3,7 | 60,1 | 322 |
Bakery products | ||||
| white bread crackers | 11,2 | 1,4 | 72,2 | 331 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| meringues | 2,6 | 20,8 | 60,5 | 440 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
| milk sauce | 2,0 | 7,1 | 5,2 | 84 |
Dairy | ||||
| milk | 3,2 | 3,6 | 4,8 | 64 |
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| cream | 2,8 | 20,0 | 3,7 | 205 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| curdled milk | 2,9 | 2,5 | 4,1 | 53 |
Cheeses and cottage cheese | ||||
| cottage cheese | 17,2 | 5,0 | 1,8 | 121 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| beef liver | 17,4 | 3,1 | 0,0 | 98 |
| boiled beef tongue | 23,9 | 15,0 | 0,0 | 231 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Fish and seafood | ||||
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| ghee | 0,2 | 99,0 | 0,0 | 892 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| coffee with milk and sugar | 0,7 | 1,0 | 11,2 | 58 |
| black tea with milk and sugar | 0,7 | 0,8 | 8,2 | 43 |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| * data is per 100 g of product | ||||
Drug treatment of duodenal ulcers
Peptic ulcer of the duodenum is currently treated with the following groups of drugs.
Medicines that reduce the production of gastric juice
The leading positions in this group are held by proton pump blockers, which slow down the secretion of hydrochloric acid:
- Products based on omeprazole - omez, gastrozole, bioprazole, demeprazole, lomac, zerocid, krismel, zolser, omegast, losek, omezol, omitox, omepar, zhelkizol, pepticum, omipix, promez, pepticum, ricek, orthanol, romsec, sopral, ultop , chelicide, cisagast, chelol.
- Medicines based on pantoprazole - controloc, sanpraz, nolpaza, peptazole.
- Lansoprazole preparations - helicol, lanzap, lansofed, lanzotope, epicure, lancid.
- Based on rabeprazole - zulbex, zolispan, pariet, ontime, hairabezol, rabeloc.
- Esomeprazole - Nexium.
H2-histamine receptor blockers have practically ceased to be used to treat peptic ulcers, as they cause withdrawal syndrome (with abrupt cessation of use, the symptoms of the disease return).
- These are ranitidine (Gistac, Rannisan), famotidine (quamatel, ulfamid, gastrsidine), cimetidine (Belomet).
Selective blockers of M-cholinergic receptors (gastrocepin, pirencipin) reduce the production of pepsin and hydrochloric acid. Used as auxiliary medications for severe pain. May cause palpitations and dry mouth.
Agents that increase the protective properties of the mucous membrane
- Sucralfate (Venter) forms a protective coating at the bottom of the ulcer.
- Sodium carbenoxolone (Ventroxol, Biogastron, Kaved-s) accelerates the restoration of the epithelium of the mucous membrane.
- Colloidal bismuth subcitrate (de-nol) forms a film on the ulcer.
- Synthetic prostaglandins (enprostil) stimulate mucus production and cell restoration.
Other drugs
- Medicines that calm the central nervous system. Tranquilizers (seduxen, elenium, tazepam), antidepressants (amitriptyline), sedatives (tenoten, valerian preparations, see sedatives).
- Blockers of central dopamine receptors (metoclopramide, raglan, cerucal) normalize intestinal motor activity.
The course of treatment for ulcers can take from two to six weeks, depending on the size of the defect and the general condition of the body.
It should be noted that a competent doctor who can monitor the treatment process and evaluate its results should prescribe treatment for duodenal ulcers, select medications and dosage regimens.
Menu (Power Mode)
As indicated, nutrition for duodenal ulcers depends on the stage of the process. The longest diet during the period of recovery and remission, therefore the menu of Table No. 1 .
The physiologically complete composition of the diet (90-100 g of proteins, 100 g of fats and 420 g of carbohydrates) allows you to adhere to it constantly. In general, this is a healthy diet with sufficient vitamin and mineral composition, moderately sparing the gastrointestinal tract. Depending on the patient’s condition and the time that has passed since the exacerbation, dishes can be pureed or not pureed. This question should be clarified by the doctor.
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Treatment of duodenal ulcers with antibiotics
Antibiotic therapy for peptic ulcers has appeared since the undoubted participation of Helicobacter pylori microorganisms in the development of the disease was proven. In the early stages of the use of antibiotics, it was believed that the war should be waged until a victorious end, that is, the complete disappearance of the microbe, which was confirmed by culture, a urease test during FGDS, or a blood test for antibodies to the bacterium. Later it turned out that not all types of Helicobacter cause disease, that it is unrealistic to destroy all Helicobacter, since when it dies in the stomach and duodenum, it moves to the lower intestines, causing severe dysbiosis and inflammation.
Re-infection is also possible when using someone else's or shared utensils and the same FGDS, which therefore must be performed only according to strict indications.
However, today it is advisable to carry out one or two courses of therapy with antibacterial drugs (amoxicillin, clarithromycin or tetracycline) for proven Helicobacter infection. If after one course of antibiotics the bacteria are not killed, then this drug is not worth repeating. A different treatment regimen is selected.
Increased length of hospitalization
If the patient does not seek medical help in a timely manner or has concomitant diseases, the length of stay in the hospital may be increased.
The main reasons for unsuccessful treatment of exacerbation of duodenal ulcer:
- reflux disease with a healed ulcer not recognized in time;
- immunity of some strains of Helicobacter pylori to antibiotic therapy (usually metronidazole);
- failure to comply with the patient's dietary instructions;
- lack of patient discipline;
- repeated infection;
- parallel treatment for other indications with non-steroidal anti-inflammatory drugs;
- the occurrence of a duodenal ulcer with a different etiology (without Helicobacter pylori infection).
Ulcer treatment regimen
First line Helicobacter pylori eradication scheme:
- Double dose proton pump inhibitor twice daily (eg 40 mg omeprazole or esomeprazole twice).
- Clarithromycin 500 mg twice daily or Josamycin 1000 mg twice daily.
- Amoxicillin 1000 mg 2 times a day.
- De-nol 240 mg twice a day.
Scheme of the second row (in the absence of FGD dynamics of ulcer size)
- Proton pump inhibitor in double dose 2 times a day (same as scheme 1)
- De-nol 240 mg twice a day.
- Metronidazole 500 mg three times a day.
- Tetracycline 500 mg 4 times a day.
Before starting therapy, Helicobacter pylori is detected using an immunological blood test (antibodies to the pathogen). Control – detection of Helicobacter antigens in feces. The urease breath test is not very informative.
The duration of eradication therapy is from 10 to 14 days. If treatment is ineffective with sequential regimens 1 and 2, Helicobacter pylori is typed and its sensitivity to drugs is determined.
Today, regimens with levofloxacin can only be used in regions of the Russian Federation where Helicobacter remains sensitive to this drug.
If duodenal ulcer is not associated with Helicobacter pylori infection, then treatment is carried out with medications that reduce the production of gastric juice. After 7-14 days of combination therapy, treatment is prescribed for another five weeks.
Important
- We should not forget that a stomach ulcer affects the functioning of the entire body, and therefore it is better to prevent this disease than to then adapt to it all your life, easing the pain with medications.
- Attacks can be prevented by following a diet and proper nutrition, giving up alcohol and cigarettes. You should visit a doctor at least once a year. For preventive purposes, patients are prescribed antiulcer medications in courses in spring and summer. It is at this time that the disease makes itself felt with the most striking manifestation of symptoms.
- It is also necessary to remember for patients suffering from peptic ulcer disease about annual endoscopic monitoring, which must be completed even in the absence of pain after the ulcer has healed. The need for such control is associated with the high probability of malignancy of gastric ulcers.
Author of the article: Tryapitsyn Alexander Valerievich (gastroenterologist, candidate of medical sciences)
Alternative treatment for duodenal ulcers
Complete or partial distrust of traditional medicine most likely does not bode well for an ulcer sufferer. There are drugs for the treatment of ulcers, the effect of which has been proven in serious random studies in humans. Also, the effect of drugs is checked by everyday medical practice. Schemes are being refined and side effects of drugs are being identified. At the same time, no one canceled the alternative possibility of being treated with folk remedies.
Freshly squeezed potato juice is considered one of the most effective traditional medicine for stomach and duodenal ulcers. It tastes rather unpleasant, but you can get used to it quite easily. It is better to use the Morning Rose or American varieties, but any unspoiled potato tuber will do. Preparing juice is quite labor-intensive, given that you only need to drink it fresh and 3 times a day, but you can get the hang of it if you want. The raw potato tuber is peeled, grated and squeezed through several layers of gauze. The juice should be drunk immediately, otherwise it turns black and loses its medicinal properties. The first 3 days only take a tablespoon before meals 30 minutes, preferably 3 times a day, then 3 days 2 tablespoons, gradually increasing to half a glass per dose and so on for 21-28 days. This requires adherence to a diet. After 2-3 weeks the course can be repeated. This really helps!
You can resort to traditional medicine, use treatment with sea buckthorn or olive oil (1 dessert spoon on an empty stomach for 3 months), honey, propolis, herbs (calendula, plantain, St. John's wort), after going on a duodenum-friendly diet and taking twice a day 20 mg omeprazole daily.
Author:
Postnova Maria Borisovna general practitioner
Folk remedies
Traditional medicine has several recipes that significantly alleviate the patient’s condition even during periods of exacerbation of duodenal ulcer. But it is important to understand that they are not a panacea and cannot guarantee that the pathology will be put into remission or full recovery.
Important: before using any traditional medicine, you should consult your doctor.
Traditional medicine used in the treatment of duodenal ulcers:
- Honey. You can simply eat it every day in its pure form - the benefits will already be provided. But it is better to mix honey and olive oil in equal proportions (for example, 500 ml each) and store in the refrigerator. Half an hour before meals you need to eat a tablespoon of medicine - there will be 5-6 such doses per day. The duration of treatment is 14 days, then a break is taken for 10 days and the course can be repeated.
- Plantain seeds. They need to be brewed in boiling water (10 g of plantain seeds per 100 ml of water), left to steep for half an hour. You need to take the product one tablespoon an hour before meals - there can be a maximum of 3 such doses per day.
- Propolis. You need to take 150 g of this product, grind it as much as possible and pour in 1 kg of melted butter. Mix everything thoroughly until the propolis is completely dissolved (if necessary, you can do this in a water bath) and take 1 teaspoon an hour before meals three times a day. The duration of treatment is 30 days, then you need to take a break for 3 weeks. The medicine is stored in the refrigerator.
- Herbal collection. It is very useful for duodenal ulcers to drink herbal infusions. For example, you can make the following: licorice root + chamomile + common knotweed + fennel seeds. All components are taken in equal proportions, and then a tablespoon of the mixture is poured with boiling water (250 ml) and infused for 20 minutes. Dosage regimen: 200 ml of prepared decoction in the morning and evening. Duration of treatment is 20 days;
- dandelion root + elecampane root + shepherd's purse + chicory - all taken in equal quantities. Take a tablespoon of the mixture and add 400 ml of cold water and leave for an hour. Then take the resulting product and boil for 10 minutes. After straining, it should be consumed before each meal, 2 tablespoons, at least 3 times a day;
- creeping wheatgrass + dandelion root + buckthorn bark - everything is taken in equal quantities. Then a tablespoon of the mixture is poured into a glass of boiling water and left for 8 hours. You should take ½ glass at night, and to improve the taste of the infusion, you can add honey or sugar to it.