Inflammation of the small intestine (enteritis) is characterized by a decrease in its functionality and structural changes in the mucous (internal) membrane. This is one of the most common pathologies of the digestive system: according to statistics, almost every person has encountered its acute manifestation, and about 25% of the entire world population suffers from a chronic form (to a greater or lesser extent).
Enteritis
The small intestine is actively involved in a number of stages of food processing. They include the absorption of nutrients immediately or after the glands secreted enzymes (enzymes) pre-catalyze the hydrolysis of complex food components, which will lead to the formation of smaller ones. When inflammation of the small intestine occurs, these functions are disrupted. That is why enteritis poses a serious danger not only to the gastrointestinal tract (GIT), but also to the entire body as a whole.
What causes intestinal colitis?
The main cause of the acute condition is various pathogenic bacteria, staphylococci or streptococci. The intestinal mucosa is sensitive and can become inflamed as a result of:
- Food poisoning.
- Allergic reaction.
- The effects of certain medications.
- Severe infectious disease.
The chronic form occurs as a result of the absence or ineffective treatment of acute colitis. Most often, chronic inflammation persists due to low immunity. The pathology can be supported by the presence in the body of other pathological foci in organs adjacent to the intestines.
Other common causes of chronic colitis:
- Worm infestation.
- Diseases of the pelvic organs in women.
- Uncontrolled use of antibiotics.
- Alcoholism.
- Chronic dysbacteriosis.
- Abuse of spices and spicy foods.
- Congenital intestinal defects.
Doctors include a monotonous diet and heavy food consumption as factors that provoke the disease.
Colitis is a common occurrence in children. The reason is that the protective barrier of the outer lining of the intestine is not yet fully formed. As a result, the organ cannot cope with various pathogenic microorganisms and an inflammatory process occurs.
In adulthood, ischemic colitis can occur. They are formed due to disruption of normal blood circulation in the mesenteric arteries (the vessel through which the intestine is attached to the peritoneum). This is a dangerous condition that requires urgent medical attention.
Instrumental studies
They also help identify acute or chronic inflammation of the small intestine. As a rule, the following studies are prescribed:
- FGDS.
- Endoscopy using a capsule.
- Colonoscopy.
- X-ray.
Endoscopic examination is very difficult. The device can only be inserted into terminal sections. The procedure itself involves taking a biopsy of the mucosa for histological analysis. It is usually possible to identify atrophic and dystrophic phenomena on the part of intestinal villi and epithelial cells.
X-ray examination, which is carried out with the introduction of a contrast agent, allows us to identify changes in the folded structure, identify segmental lesions, ulcers, and tumor formations. The state of intestinal motor function is also assessed.
Classification of the disease
Depending on which parts of the intestine are affected by the inflammation, the following are distinguished:
- typhlitis;
- transversit;
- sigmoiditis;
- pancolitis;
- proctitis
The most common form is pancolitis. It affects the entire large intestine.
Due to their occurrence, they are distinguished:
- infectious;
- medicinal or toxic;
- ischemic - typical for patients after 55-60 years;
- radiation or radiation;
- ulcerative is the most common type.
Pathology can occur with the formation of erosions, ulcers, necrosis and hemorrhages. This is how catarrhal and erosive ulcerative colitis manifests itself.
Inflammation of the mesentery of the small intestine
This disease deserves special attention. The mesentery is a kind of ligament that secures the abdominal organs. It is also responsible for transmitting nerve impulses through NS receptors, supporting the immune system and providing oxygen and nutrients.
Very rarely, the mesentery becomes inflamed on its own. This usually occurs against the background of peritonitis. It is almost impossible to recognize the pathology, since the clinical picture is varied. The most common and characteristic symptom is pain in the navel area, manifesting itself in varying intensities.
Unobvious symptoms include enlarged mesenteric lymph nodes, hyperemia and swelling of the inflamed area. Then foci of granulation tissue begin to develop, which later become scars.
Main signs of colitis
Symptoms vary depending on the type of disease. Acute colitis is characterized by an abrupt onset. A person complains of the following symptoms:
- diarrhea;
- widespread abdominal pain;
- vomiting;
- flatulence;
- cutting or burning pain in the rectal area;
- feverish condition.
Colitis stool usually contains blood or mucus. Due to frequent vomiting, symptoms of dehydration occur: weakness, hypotension, pale skin, thirst.
Chronic inflammation has a sluggish course. Manifestations are mild. Periods of exacerbation and calm are characteristic. The following signs may indicate the presence of inflammation in the large intestine:
- bowel dysfunction;
- aching pain, mainly in the side and lower abdomen;
- characterized by increased discomfort after eating or during active movements;
- constant bloating;
- belching;
- unpleasant taste in the mouth;
- heartburn.
A distinctive feature is that thermal procedures (heating pad, bath, mud procedures) lead to an increase in the intensity of pain. 80% of patients with this diagnosis experience a decrease in appetite.
Medicines
Insufficiency of digestive enzymes is corrected with drugs such as Festal, Pancitrate and Pancreatin. Absorption is stimulated with medications containing nitrates. Protective drugs successfully restore the functionality of cell membranes.
As part of the treatment of diphtheritic inflammation of the small intestine (or any other), Loperamide is often prescribed, which suppresses excessive propulsive motility.
For patients with diarrhea, astringents, antiseptics, adsorbent and enveloping medications are indicated. Herbal medicine is often used for these purposes (decoctions of sage, chamomile, bird cherry, St. John's wort, alder cones, blueberries).
And to correct dysbiosis, eubiotics and probiotics are prescribed. Intravenous administration of amino acid solutions may be indicated. But this is if absorption is pronounced and is accompanied by severe protein deficiency.
Sometimes diverticula and polyps develop against the background of enteritis. If such neoplasms make themselves known, then surgical removal is prescribed.
What complications can there be?
Without appropriate and timely treatment, inflammation of the mucous membrane can lead to functional disorders. The most common are:
- the appearance of a scar, which leads to a narrowing of the lumen of the large intestine;
- internal bleeding;
- tissue necrosis, which leads to the development of peritonitis;
- non-traumatic perforation or rupture of the intestine;
- acute obstruction due to the formation of adhesions.
These conditions pose a threat to human life. It is important to consult a doctor at the first manifestations of the disease.
Causes
Inflammation of the small intestinal mucosa may have different causes. In general, the reasons can be identified in the following list:
- Nutritional features. At risk are people who are unable to eat normal food, as well as lovers of fried, smoked and fatty foods. Lack of a diet leads to malfunctions of the entire gastrointestinal tract. According to statistics, this is the most common reason. It occurs in 75-80% of cases.
- Helminthiasis. Due to Giardia and Ascaris, inflammation of the small intestine also often develops.
- Infectious lesion. If a person has consumed an expired or low-quality product, then the likelihood of becoming infected with Shigella or Salmonella increases significantly.
- Dysbacteriosis. If there are already problems with the large intestine, then there is a high chance of them spreading to the small intestine.
- Autoimmune diseases. Enteritis arising for this reason is rare. Such cases are difficult to treat. The most common autoimmune disease is Crohn's disease. It can cause not only inflammation of the small intestine - the entire gastrointestinal tract is at risk. And the cause of autoimmune diseases is any failure of the body's defense system.
- Allergy. As a rule, enteritis occurs in children for this reason. But it also occurs in adults, although less frequently.
- Genetic features. Surely many people know that the specifics of the digestive system are determined by heredity. Therefore, if one or more parents had an enzymatic deficiency, then the child will receive the same characteristics and a “bouquet” of possible problems. Among them is a predisposition to colitis, enteritis, etc.
- Heat intolerance. It is important to mention such a concept as “summer diarrhea”. This name hides hyperactivity of the small intestine, which makes itself felt in extreme heat (not all people tolerate it well).
In addition to the above, the cause of inflammation of the small intestine can be a recent operation or injury.
Diagnosis of pathology
Only a gastroenterologist can make the correct diagnosis. For this purpose, it is mandatory to order a scatological examination. It includes chemical, microscopic and bacteriological examination of stool in the laboratory. The Gregersen reaction test is also performed. This test aims to detect blood in the stool.
The doctor also recommends the following instrumental studies:
- X-ray of the abdominal cavity.
- Intestinal endoscopy (colonoscopy).
- Irrigoscopy - x-ray with the introduction of contrast into the colon. Allows you to accurately detect the inflammatory process and the boundaries of its spread.
It is imperative to exclude diseases such as polyposis and intestinal cancer. A warning sign is blood during and after bowel movements. This condition requires a comprehensive and thorough study. Consultation with doctors of related specialties is recommended.
Analyzes
Well, above we briefly talked about the features of inflammation of the small intestine. Treatment will be discussed a little later, but for now we need to pay attention to the specifics of diagnosis.
First of all, the gastroenterologist collects the patient’s medical history, conducts an initial examination, and palpates the abdomen. Tests are required. And here's what they are:
- General blood analysis. Helps detect signs of inflammation. They are indicated by a high level of leukocytes and ESR.
- Stool analysis. With its help, enzymatic deficiency is determined, and the completeness of the digestive function is assessed. It is also possible to detect infectious lesions. Typically, fat, starch, and muscle fibers are found in the biomaterial.
- Biochemistry of blood. Allows you to identify signs of malabsorption syndrome.
How to treat intestinal colitis
During the period of exacerbation, as well as in severe cases of acute colitis, a person must be hospitalized. Treatment on an outpatient basis is carried out only after acute symptoms have resolved and there are no complications.
Therapy is aimed not only at combating inflammation, but also at reducing the sensitivity of the intestinal mucosa. At the first stage, doctors’ efforts are concentrated on eliminating signs of dehydration and normalizing the functioning of all parts of the intestines.
In chronic cases, an important treatment method is to follow a special therapeutic diet.
Diet therapy
Nutrition is adjusted at any stage of the disease. In the acute phase, it is necessary to help the intestines, so all heavy, difficult-to-digest foods are excluded from the diet. The list of prohibited products includes:
- smoked meats;
- sugar, sweets;
- meat, including broths;
- legumes;
- salt, vinegar;
- vegetables fruits;
- all products that are aimed at improving intestinal motility.
The amount of salt per day should not exceed 8-10 grams. Dishes should be served stewed, boiled or pureed. Steaming is allowed, without adding fat. Meals should be frequent, small portions. There are no restrictions on water intake.
During the period of exacerbation, the gastrointestinal tract should be spared as much as possible. To do this, you must strictly follow all the recommendations of your doctor. On average, a special diet is prescribed for 3-5 days. This is enough to relieve acute symptoms.
Conservative treatment
If therapeutic nutrition is ineffective, as well as when concomitant gastrointestinal diseases are detected, a course of antibacterial drugs is necessary.
The dose and duration of the course are selected by the doctor individually. The purpose of antibiotics is to reduce the number of pathogenic microorganisms. When dysbiosis increases, the microflora is restored with the help of probiotics and prebiotics.
If agreed with a doctor, medicinal herbal infusions can be used as an additional treatment. They help control inflammation, reduce pain and manage diarrhea.
If worms and protozoa are detected in the tests, a course of antiparasitic therapy is recommended. Sometimes it is advisable to use sorbents and intestinal antiseptics.
The inflammatory process in the lower intestines is well controlled with local anti-inflammatory treatment. For this purpose, anal suppositories and microenemas are prescribed. They help not only regulate intestinal motor function, but also have a local analgesic and bactericidal effect.
If the patient complains of constipation, laxatives, suppositories or enemas are indicated. To improve local immune forces, vitamins and immunostimulating drugs can be prescribed.
Surgical method of treatment
Surgery is recommended only in exceptional cases when there is a risk to human life. These include all complications of colitis - the development of peritonitis, intestinal rupture, internal bleeding.
Relative indications for surgical treatment may be partial intestinal obstruction or lack of positive dynamics during drug therapy.
Surgery is often performed for advanced ulcerative colitis. To do this, a coloproctectomy is performed - radical removal of the colon.
Treatment
Treatment of intestinal inflammation should only be comprehensive: taking medications (including taking antibiotics), following a diet. Herbs for intestinal inflammation can be used, but only in consultation with the attending physician.
The issue of hospitalization is decided on an individual basis. If there is no risk of developing serious complications, therapy can be carried out at home. An integrated approach to therapy makes it possible to ease intestinal function in adults and children.
The doctor may prescribe the following medications:
- antibiotics;
- non-steroidal anti-inflammatory;
- probiotics;
- enterosorbents;
- adsorbents;
- aminosalicylates.
Treatment with antibiotics is prescribed when the development of the pathological process is infectious. The drug regimen is determined on an individual basis.
Treatment of intestinal inflammation with folk remedies is possible, but this must be discussed with your doctor. The following herbs can be used:
- flax seeds;
- oak root
It is important to understand that any medicine for intestinal inflammation should be prescribed only by your doctor. This is especially true for antibiotics.
However, antibiotics and other drugs will not give the desired therapeutic effect if the diet for intestinal inflammation is not followed. The list of prohibited and permitted products is determined by a gastroenterologist. Nutrition for intestinal inflammation implies the following general recommendations:
- exclusion of spicy, fatty, salty, pickled, preserved foods;
- products that cause fermentation and increased flatulence are excluded;
- meals should be divided, 5–6 times a day, with a time interval of 2–3 hours;
- correct drinking regime;
- food should be warm, liquid, slimy consistency.
Provided that all the doctor’s recommendations are followed correctly and in a timely manner, treatment even at home gives positive results.
Intestinal colitis: prognosis and prevention
If you seek medical help in a timely manner and follow the prescribed diet and treatment, the prognosis is favorable. After the acute period is over, performance is fully restored and well-being improves.
But to increase the duration of the remission period, a person with colitis needs to eat properly throughout his life. Long fasting or strict diets are excluded. You should forget about snacks on the run, fast food, as well as fatty, spicy and smoked foods.
It is also necessary to treat all gastrointestinal diseases in a timely manner. It is important for women to visit a gynecologist annually to identify inflammatory diseases in the pelvic organs at the initial stage.
It is recommended to undergo sanatorium-resort treatment in health institutions that specialize in gastrointestinal pathologies.
Boost your immunity and eliminate bad habits. Try to avoid prolonged stress. If you suspect you have colitis, treatment should only be prescribed by a gastroenterologist after a thorough examination.
Forecast
If enteritis has a mild or moderate form, then with proper treatment prescribed by a doctor, it goes away in a few days.
When the disease is advanced, things are somewhat more complicated. The severe form often leads to complications, including necrosis, bleeding, severe dehydration, and perforation.
A chronic disease, which occurs with alternating exacerbations and remissions, slowly progresses. Enteritis worsens, inflammation spreads throughout the gastrointestinal tract, and signs of malabsorption intensify. If proper measures are not taken, death is quite possible. The cause will be severe disturbances of internal homeostasis, as well as exhaustion.
Enteritis also often entails the addition of infections.
In mild and severe forms, performance is maintained. But people certainly experience difficulties. Physical exertion and emotional stress cause him discomfort.
Structure
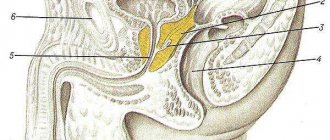
The small intestine is a very long (2 to 5 m) hollow tube. It starts from the stomach and ends in the ileocecal angle, at the point of its connection with the cecum. Anatomically, the small intestine is conventionally divided into three sections:
1. Duodenum. It is located in the back of the abdominal cavity and is shaped like the letter “C”;
2. Jejunum. Located in the middle part of the abdominal cavity. Its loops lie very freely, covered with peritoneum on all sides. This intestine got its name because when autopsying corpses, pathologists almost always find it empty;
3. Ileum - located in the lower part of the abdominal cavity. It differs from other parts of the small intestine in having thicker walls, better blood supply and a larger diameter.
Lymphatic vessels
The lymphatic vessels of the small intestine begin in the villi of the mucous membrane; upon leaving the wall of the small intestine they enter the mesentery. In the mesenteric area, they form transport vessels that are capable of contracting and pumping lymph. The vessels contain a white liquid similar to milk. That's why they are called milky. At the root of the mesentery are the central lymph nodes.
Some lymphatic vessels may empty into the thoracic stream, bypassing the lymph nodes. This explains the possibility of rapid spread of toxins and microbes through the lymphatic route.