Pain syndrome
The appearance of pain is typical for large cysts, as they compress the surrounding tissues, including the nerve plexuses. Small cysts do not exert such pressure, therefore, as a rule, there are no complaints of pain. This symptom is especially characteristic for the period of formation of false cysts during acute and exacerbation of chronic pancreatitis, and it is caused to a greater extent by destructive processes. Over time, the intensity of the pain decreases, it is characterized as “dull” or rather “discomfort”. A characteristic symptom is the “lucid interval” (temporary improvement and absence of pain after acute pancreatitis or injury). The most severe pain is caused by cysts located on the posterior surface of the gland and compressing the solar plexus area. Impact on this nerve plexus creates in patients a very intense, long-lasting burning pain that radiates to the back. Movement, compression by clothing, a belt, or a belt increase its intensity. The condition is somewhat alleviated when taking the knee-elbow position (“on all fours”). A pronounced increase in pain - “dagger” pain can indicate the occurrence of complications (for example, rupture of a cyst), gradual progression of pain along with an increase in body temperature and the appearance of intoxication - about its suppuration.
Dyspepsia
Other manifestations of pancreatic cysts may include dyspeptic disorders: nausea, vomiting (which may result in an attack of pain), and stool instability. As a result of the decrease in the amount of pancreatic juice entering the intestines, the digestion of food and the absorption of nutrients are disrupted. As a result, the patient loses weight, loses weight, and becomes weak.
Intestinal obstruction
Sometimes large pancreatic cysts cause compression of neighboring organs, impairing their patency. When a cyst is located in the head of the gland, obstructive jaundice may occur (yellowishness of the skin, sclera, and itchy skin appears); if the portal vein is compressed, swelling in the legs or ascites develops. Very rarely, large pancreatic cysts compress the intestinal lumen (duodenum), which interferes with the passage of food. In these cases, incomplete high intestinal obstruction may form.
general characteristics
A pancreatic cyst is a fairly common complication of pancreatitis. Such cavities are formed when organ tissue is damaged, circulatory problems and the outflow of pancreatic juice occur. As a result of such processes, in place of dead cells, a capsule is formed, bounded by walls of connective tissue cells. Most often it is filled with pancreatic juice, but its contents can be pus, blood or inflammatory exudate. The process of its formation can be long - from 6 to 12 months.
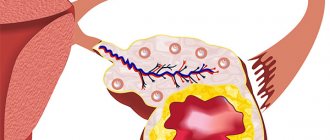
In many cases, a cyst on the pancreas forms at the site of dead parenchyma cells. When inflammation or accumulation of pancreatic juice occurs, tissues are damaged in one place. Moreover, this area is most often limited. Connective tissue grows in it. Gradually, immune cells destroy the inflammatory focus, but the cavity may remain. Such a postnecrotic cyst is filled with dead cells, inflammatory exudate, blood, but most often with pancreatic juice.
Sometimes the cyst does not cause any discomfort to the patient. But it can compress the ducts, leading to disruption of the outflow of pancreatic juice. In addition, its course may become more complicated. Sometimes fistulas appear, the cyst can fester, and bleeding occurs due to damage to the blood vessels.
A type of such pathology, in which many cavities form in the area of the gland ducts, is cystic fibrosis or cystic fibrosis. This is a congenital genetic pathology, which is characterized by thickening of pancreatic juice and blockage of the gland ducts. But cysts form not only in this organ, but also in the lungs or intestines.
A cyst is a round cavity filled with fluid that can form anywhere in the gland.
Standard classification
To understand the diameter of the affected area, its location, and also to find out whether the inflammation has affected neighboring soft tissues, modern diagnostic methods are used. They are considered a mandatory item in the plan before prescribing a surgical intervention, which allows not only to study the problem in detail, but also to use the collected information during the operation itself.
Content:
- Standard classification
- Features of each type
- When is it time to see a doctor
- Radical approach
- Success forecast
The most productive versions of diagnostics are computed tomography and magnetic resonance imaging, as well as ERCP. In the first two cases, the stage of adding a contrast agent is not mandatory, but the last type of analysis is completely based on it.
Only after receiving the visualization in hand does the attending specialist make the final decision regarding whether the operation is possible and which format will be the most effective. Most often, classic internal or external drainage is used. A little less often, experts resort to resection of part of the pancreas along with the area that threatens the entire body.
According to statistics, pancreatic cysts have been diagnosed much more often in recent years, and mostly young people become its victims. Researchers explain the sharp rejuvenation of patients in the gastroenterology inpatient department by the fact that young people more often began to suffer from acute and chronic pancreatitis. Moreover, their etiology varies from classic traumatic to biliary or acquired alcoholic, which over the last ten years has become a real scourge among doctors.
According to the same statistical summary, a cyst is the most common consequence of complications of chronic pancreatitis. It accounts for about 80% of clinical cases of the total.
Difficulties are added by the fact that in the medical community there is no common understanding of what formations should be classified as pancreatic cysts. Because of this, one general set of rules regarding the classification of such pathology is not provided, as well as standards of pathogenesis with the provision of care.
Some adherents insist that the cyst must have pancreatic juice inside and also be limited to the walls. Others believe that the contents may even be necrotic parenchyma or:
- blood;
- pus;
- inflammatory exudate.
The only thing both camps agree on is the principles of anomaly formation. They provide the following conditions:
- parenchymal damage;
- problematic secretion outflow;
- local failure of microcirculation.
There is a separate classification of pathologies, which is divided according to the parameters of their formation. But even they have several divisions for the convenience of establishing a specific diagnosis. Basic sorting involves dividing diseases into the following types:
- congenital;
- inflammatory;
- traumatic;
- parasitic;
- neoplastic.
The first item includes several more subitems such as dermoid and teratoid, as well as fibrocystic degeneration, adenomas, and polycystic disease.
But frequently occurring pseudocysts are a representative of a number of inflammatory categories, which also include retention variants. Separately, there is a sorting for neoplastic versions, which affects the following subtypes:
- cystadenomas;
- cavernous hemangiomas;
- cystadenocarcinoma;
- epitheliomas.
They all differ in the course of the disease, cure measures, and approaches to rehabilitation therapy.
Varieties
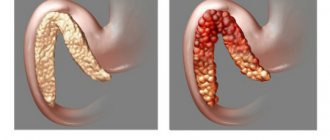
Most often, all such formations in the pancreas are divided into two groups. True cysts include cavities lined from the inside with epithelial cells. They can form due to pathologies of the gland ducts or due to abnormalities in intrauterine development. A pseudocyst is a formation that arises at the site of an inflammatory focus. Although this pathology is more common than true cysts, many scientists do not classify them as a separate group.
In addition, cysts formed during pancreatitis are classified. There are acute formations that often do not have their own walls. Their role can be played by the walls of the ducts, the gland itself, or even other organs. There is also a pathology such as cystofibrosis, in which well-formed cavities, usually round in shape, are formed. Their walls are formed of fibrous tissue. The most difficult case is when an abscess filled with pus occurs. This condition is also classified as a cyst, since it forms at the site of a festering cyst or dead tissue due to necrosis.
Such formations are also classified according to their location. Most often, a cyst forms in the head of the pancreas, since there are the most ducts here, the bile duct passes through, and there is a connection with the duodenum. A cyst of the body or tail of the pancreas may also appear.
In addition, sometimes cysts are classified according to the type of tissue and the reason for their appearance:
- traumatic appear as a result of injury or blunt trauma to the abdomen;
- parasitic are a reaction to infection by parasites, for example, echinococci;
- congenital appear during intrauterine development;
- retention occurs as a result of blockage of the ducts;
- pseudocysts form at the site of cell death.
Cysts can vary in location, size and content
Pancreas
This organ is located, as its name suggests, under the stomach. But not always, only when a person is lying down. When the subject is in an upright position, it is located behind the stomach, just above the navel. The organ is small, does not exceed 20 cm in length. The head is located in the loop of the duodenum, the tail approaches the spleen.
Since iron plays a big role in the digestion of food and the production of insulin, a person cannot do without it; it must be protected so as not to die of hunger when there is an abundance of food. So, the more a person knows about the pancreas, the better.
Digestion involves enzymes that, entering the intestine through the duct, break down proteins, fats and carbohydrates. Before entering the duodenum, the enzymes are in an inactive state. But if it happens that there is an obstacle in the way of the secretion of the gland, then the enzymes will begin to digest the body of the organ itself.
Causes
Recently, this pathology is becoming more common. Moreover, the cause in many cases is pancreatitis. The acute form of the disease, leading to the death of parenchyma cells, leads to the formation of such a cavity in approximately 15-20% of cases. This happens 3-4 weeks after the onset of inflammation, when an area of necrosis appears in the gland tissue. But in most cases, such cavities are formed during chronic pancreatitis. More than half of patients, especially those who do not follow doctor’s recommendations, are faced with such a diagnosis.
The formation of a postnecrotic cyst can be caused by a violation of the outflow of pancreatic juice, narrowing of the sphincter of Oddi, and cholelithiasis. All these pathologies lead to the death of pancreatic cells, and in many cases a cavity forms in their place. But other reasons can also cause the development of such a process:
- abdominal trauma;
- disruption of the blood supply to the gland due to blockage of blood vessels by a blood clot;
- arterial dissection;
- disturbances in the intrauterine development of the ductal system of the gland;
- parasitic infections.
Prices for services *
| Name of service | Price |
| Consultation with a chemotherapy doctor | Price: 5,150 rubles |
| Carrying out intrathecal chemotherapy | Price: 15,450 rubles |
| MRI of the brain | Price from 8,900 rubles |
| Chemotherapy | Price from 50,000 rubles |
| Comprehensive Cancer Care and Hospice Program | Price from 9,690 rubles per day |
| Gastrointestinal tract oncology program | Price from 30,900 rubles |
| Lung oncology program | Price from 10,250 rubles |
| Urinary system oncology program | Price from 15,500 rubles |
| Oncology diagnostic program “women’s health” | Price from 15,100 rubles |
| Oncology diagnostic program "men's health" | Price from 10,150 rubles |
Download price list for services
We work around the clock
Sign up for a consultation by phone or send a request through the form
Symptoms
The formation of a cyst does not always cause discomfort to the patient. Small formations that do not compress the gland ducts or other organs can go unnoticed for a long time. Moreover, in many cases its formation occurs against the background of inflammatory processes, so pain is attributed to pancreatitis. The pain from a cyst may not be severe, manifesting itself as slight discomfort. Or it occurs spasmodically. Severe pain occurs when the cyst compresses ducts, nerve fibers, and other organs.
If the cyst grows up to 5 cm or compresses surrounding tissues, it can cause pain, nausea, and digestive upset.
In addition, the following symptoms of pancreatic cysts may be observed, which resemble an exacerbation of gastrointestinal diseases:
- nausea, sometimes vomiting;
- belching, flatulence, heartburn;
- intestinal dysfunction;
- lack of appetite;
- due to deterioration in nutrient absorption, weight loss may occur;
- decreased performance.
If the cyst grows more than 5 cm, it will certainly manifest itself as more serious disorders. Signs of this condition will depend on the location of the formation. A cyst located on the head of the gland often compresses the bile ducts. This manifests itself in the form of mechanical jaundice and severe skin itching. Compression of blood vessels can cause disruption of the blood supply to the abdominal organs and even swelling of the lower extremities. Large cysts in the tail of the pancreas sometimes interfere with the flow of urine and lead to urinary retention, and can also compress the intestines or spleen. The result of this is intestinal obstruction and other pathologies.
Diagnostics
Not everyone understands how dangerous a cyst in the pancreas is. But although it is benign, the consequences of leaving it untreated can be serious. First of all, the cyst can grow, which will lead to compression of the tissue of the gland itself or other organs. In addition, it can fester and be complicated by perforation of the walls or bleeding. Therefore, if you suspect such a pathology, you must undergo an examination.
Upon examination, the doctor may immediately suspect the presence of a pancreatic cyst due to characteristic symptoms, and if the formation is large, a protrusion of the abdomen on one side. But an instrumental examination is still prescribed. The most common method is ultrasound. Such a study allows you to confirm the presence of a cyst, estimate its size, and suspect the development of complications. If necessary, an MRI is prescribed, which can accurately determine the size of the formation, connection with the ducts, and tissue damage.
A cyst can only be detected during an instrumental examination; most often, an ultrasound is performed for this purpose.
Sometimes a CT scan or scintigraphy is also prescribed to clarify the diagnosis and detail the pathology. And at the stage of preparation for surgery, ERCP – endoscopic retrograde cholangiopancreatography – is mandatory. It is needed to obtain detailed information about the type of cyst, its connections with ducts, vessels and other tissues.
Diet
Diet 5th table
- Efficacy: therapeutic effect after 14 days
- Duration: from 3 months or more
- Cost of products: 1200 - 1350 rubles per week
It is the most important component of the treatment process both during conservative therapy and after surgical intervention. The main one is Table No. 5 (pancreatic) for the entire period of treatment and No. 5, which is prescribed if necessary for up to 1 year. Most patients with this pathology (forum “pancreatic diseases”) believe that it is dietary nutrition that helps minimize the risk of complications.
Treatment
Treatment of pancreatic cysts is only possible through surgery. But there is not always a need for surgery. After all, if the cyst is small, does not grow and does not compress the tissue, it does not cause any discomfort. In this case, the patient only needs to follow a diet and undergo regular examinations by a doctor so as not to miss possible complications.
Emergency medical care is required when the patient experiences severe pain in the abdomen, loses consciousness, has uncontrollable vomiting of blood, and heart palpitations. It is necessary to take him to a medical facility, preferably to the surgery department, since most likely he will need surgery. After all, such symptoms appear when a cyst ruptures, ducts are blocked, or bleeding occurs.
When choosing a method of surgical treatment, the doctor always focuses on individual characteristics. Large cysts, especially if they enlarge or threaten to compress the ducts, must be removed. Most often this is done together with part of the gland itself. The volume of tissue removed depends not only on the size of the cyst, but also on the condition of the parenchyma. To prevent relapse, the damaged part of the gland can be removed. But such radical operations are rarely done, since serious complications are possible after this.
If the cyst cavity is small and is not complicated by other pathologies, drainage may be recommended. The wall of the formation is pierced and its contents are sucked out. There are several types of drainage. If the cyst does not affect the pancreatic ducts, puncture is performed through the skin. A drainage is installed through which the contents of the cyst flow out. Sometimes laparoscopic intervention or transgastric drainage is also performed.
Symptoms of insulinoma
Among the conservative methods of treating cysts, symptomatic therapy is used. Typically, pancreatic function in this pathology is reduced, so it is recommended to constantly take enzyme preparations. This could be Pancreatin, Panzinorm, Creon, Festal. Patients who adhere to certain dietary restrictions and take enzyme preparations prescribed by a doctor feel well and can avoid complications of the pathology.
But sometimes other medications are also required. These can be antispasmodics or analgesics for severe pain, carminatives for flatulence, and antiemetics. For a parasitic cyst, a course of anthelmintic drugs is required. Sometimes it is possible to relieve symptoms with folk remedies. Most often, herbal teas based on calendula decoction are recommended. It is useful to add celandine, yarrow, chicory, currant leaves and lingonberry to them.
Nutrition
Regardless of the chosen treatment method, a patient who has been diagnosed with this condition needs to switch to a dietary diet. Food should be taken in small portions, quite often - up to 6-7 times a day. This will take the load off the pancreas. Be sure to exclude foods that stimulate the production of pancreatic juice. These are mainly strong broths, spices, fatty foods, marinades and pickles. But it is also not recommended to consume foods that have a pronounced taste.
Following a special diet will help avoid complications and help the patient feel good
Prohibited foods include alcoholic beverages, coffee, soda, sweets, smoked foods and pickles. It is undesirable to eat legumes, cabbage, radishes, radishes, garlic, and mushrooms, as these products cause increased gas formation. To reduce the load on the gland, food should be taken pureed. It is forbidden to fry it; it is better to steam it, boil it or stew it.
A diet for pancreatic cysts involves consuming the following foods:
- lean meat and fish;
- skim milk, kefir, fermented baked milk, natural yogurt;
- rice, buckwheat, oatmeal;
- boiled eggs;
- dried white bread, crackers, biscuits;
- boiled or baked vegetables;
- fresh herbs;
- fruits in small quantities, but not sour;
- dried fruit compote, rose hip decoction, weak green tea.
Complications
The prognosis for a pancreatic cyst depends on the cause of the pathology, the location of the cavity and the timeliness of treatment. Almost half of the cases of the disease are accompanied by complications. Fistulas appear, perforation, bleeding or suppuration may occur. In this case, infection of the abdominal cavity is possible - peritonitis. Sometimes this benign formation can develop into a malignant tumor.
The question of the need for surgery to remove a cyst is decided individually
Even with timely treatment, the pathology can still have serious consequences. If its causes are not eliminated, the cyst may form again. Therefore, it is very important to take measures to prevent this condition. To do this, you need to eat right, give up alcohol and smoking, and if any signs of disruption of the gastrointestinal tract appear, carry out treatment in a timely manner.