Gastritis with reduced secretion, or hypoacid gastritis, ranks fifth in frequency among various gastric pathologies. This pathology is characterized by a decrease in the number of glandular cells and the gastric glands themselves, and the remaining cells lose their morphological and functional properties.
Causes and risk factors
The mechanism of occurrence of the pathology is not fully understood. Exogenous causes of the development of gastritis with low acidity include infection with Helicobacter pylori, taking medications that have an adverse effect on the gastric mucosa, poor nutrition, bad habits, ionizing radiation, as well as accidental or intentional ingestion of toxic, irritating substances.
With timely diagnosis, timely and correct treatment, the prognosis is usually favorable; it worsens with the development of B12-deficiency anemia.
Endogenous factors include genetic predisposition, pathologies of the pancreas and liver, gastroduodenal reflux, metabolic and endocrine diseases, sinusitis, renal failure, rheumatic diseases, and helminthic infestations.
Improper treatment of acute gastritis can lead to chronicity of the pathological process. Hyperacid gastritis, in the absence of adequate treatment, over time transforms into gastritis with low acidity.
The exogenous cause of gastritis with low acidity is infection with Helicobacter pylori
In children, gastritis with low acidity often occurs in the first years of school, which is associated with a change in diet against the background of increased physical and mental stress.
Causes of gastritis
Of greatest interest are the causes of chronic gastritis. There are external and internal factors that provoke the development of the disease. Interestingly, in some people, gastritis develops much more slowly and does not have a significant effect on the body. That is, most likely, the causes of gastritis are hidden behind many factors and their combinations.
The most significant external causes of gastritis:
- Impact on the stomach walls of Helicobacter pylori bacteria, less often other bacteria and fungi. Approximately 80% of patients diagnosed with gastritis produce acid-fast bacteria that actively penetrate the wall of the gastric mucosa, secrete specific substances that irritate the mucous membrane, stimulate local changes in the pH of the walls and their inflammation. The definitive answer to why these bacteria cause significant harm to some people and not to others is still unknown;
- Eating disorders. It has been established that poor nutrition is a common cause of gastritis. The statement is true in both cases of overeating and undereating. You should diversify your diet with plant foods rich in vitamins and plant fiber, which normalizes peristalsis. However, when the initial stages of gastritis develop, it is necessary to avoid foods containing coarse plant fiber, as well as fatty, spicy, canned and pickled foods;
- Alcohol abuse is identified as a separate cause of gastritis. Ethanol in small quantities is an important component of biochemical processes in the body, but large amounts of alcohol provoke an acid-base imbalance in the body. In addition, alcohol in large doses with regular use significantly harms other digestive organs - the liver, pancreas, and also has a detrimental effect on metabolic processes in the body;
- It has been noted that some drugs widely used in medicine as anticoagulants (antiplatelets), painkillers and anti-inflammatory drugs have serious side effects - they irritate the gastric mucosa. Gastritis is most often caused by non-hormonal anti-inflammatory drugs (aspirin, analgin) and glucocorticoid hormones (prednisolone). It is recommended to use these medications strictly according to medical prescription, in small doses, in small doses, after meals;
- Some researchers note the influence on the development of gastritis from helminthic infestations, chronic stress, and aggressive chemicals swallowed accidentally or intentionally.
The main internal (related to disturbances of homeostasis) causes of gastritis:
- Congenital human predisposition to gastrointestinal diseases;
- Duodenal reflux is a pathological release of bile from the duodenum into the stomach. Bile, entering the stomach cavity, changes the pH of the juice and irritates the mucous membrane. Initially, inflammation of the antrum of the stomach develops, and then its other parts are involved;
- Autoimmune processes, damage at the immune level to the protective properties of the cells of the gastric mucosa. As a result, cells stop functioning normally and lose their original properties. This phenomenon triggers a cascade of small reactions that change the pH of the juice, and leads to constant irritation of the stomach walls. Endogenous intoxication occurs and the resistance of the mucous membrane to the aggressive environment of gastric juice is impaired;
- Disturbances of hormonal and vitamin metabolism, reflex effects of the pathogenesis of organs adjacent to the stomach.
Forms of the disease
The main forms of chronic gastritis:
- superficial (non-atrophic);
- atrophic;
- special forms (radiation, reactive, granulomatous, eosinophilic, hypertrophic, etc.).
Depending on the etiology, gastritis can be:
- autoimmune (type A);
- bacterial (type B);
- chemical (type C);
- mixed;
- alcoholic;
- medicinal; etc.
Depending on the location of the pathological process:
- gastritis of the antrum;
- gastritis of the fundus;
- pangastritis.
Forms of gastritis depending on the lesion
Chronic gastritis with low acidity can be in remission or exacerbation. In addition, the disease can be uncomplicated or complicated (bleeding, malignancy).
Symptoms of gastritis with low acidity
Gastritis with low acidity can be asymptomatic for a long time. In other cases, its leading manifestation is dyspeptic syndrome, which is caused by a pronounced impairment of the functional activity of the stomach. Pain in this form of the disease is associated with stretching of the stomach, and not with muscle spasm. Typically, patients complain of a dull, aching pain that appears or worsens after eating (the so-called satiety pain, in contrast to the hunger pain characteristic of gastritis with high acidity). The intensity of pain correlates with the quantity and quality of food eaten - the pain intensifies when eating hot, spicy foods. Dyskinetic disorders cause alternation of constipation and diarrhea, the development of dumping syndrome, flatulence, and bloating.
Symptoms of gastritis with low acidity
During the period of remission, the disease usually does not manifest itself in any way. During an exacerbation, there is a feeling of bitterness in the mouth, bad breath, increased salivation, belching of rotten or air, a feeling of heaviness in the epigastric region, nausea. Appetite decreases to the point of complete refusal to eat.
Gastritis with low acidity is recorded in all age groups, but is more often found in the elderly; men and women are equally susceptible to it.
Atrophy of the gastric mucosa, which develops with gastritis with low acidity, causes impaired absorption of nutrients and vitamins with the further development of protein-energy deficiency, hypovitaminosis, and anemia. The patient's blood pressure decreases, dizziness appears after eating, dry skin, brittle hair, bleeding, increased fatigue, and depression. Body weight is significantly reduced. Lactose intolerance may develop. With a long course of the disease, inflammation of the tongue and gums develops (glossitis and gingivitis).
What is gastritis?
Gastritis is an inflammation of the mucous layer of the stomach, leading to disruption of the functions of this organ. When gastritis occurs, food begins to be poorly digested, which results in loss of strength and lack of energy. Gastritis, like most diseases, can be acute or chronic. In addition, gastritis is distinguished with low, normal and high acidity of the stomach.
Currently, gastritis can already be called the disease of the century. It affects both adults and children. And according to health statistics, in Russia about 50% of the population has gastritis in some form.
Gastritis is characterized by a variety of external and internal causes that provoke the development of pathology. Clinically, it occurs in the form of inflammation (acute or chronic). Acute inflammation occurs for a short time. Damage to the mucous membranes of the stomach by concentrated acids, alkalis and other chemicals can be fatal.
A long-term (chronic) illness reduces the quality of life and manifests itself in the form of pain, as well as:
- Heaviness in the abdominal area;
- Heartburn;
- Belching;
- Vomiting;
- Diarrhea and/or constipation;
- Bloating;
- Flatulence - release of gases;
- Bad breath.
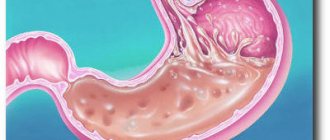
The chronic form is dangerous due to atrophy of the gastric mucosa. As a result, the stomach glands stop functioning normally. Atypical cells are formed in place of healthy cells. An imbalance in the self-healing process of cells in the gastric mucosa is one of the causes of ulcers and cancer of the gastrointestinal tract.
The stomach is the most vulnerable part of the digestive system. At least three complex digestive processes occur in it: mechanical mixing of the food coma, chemical breakdown of food and absorption of nutrients.
The most often damaged is the inner wall of the stomach - the mucous membrane, where the production of two mutually exclusive components of digestion occurs - gastric juice and protective mucus.
Digestion in the stomach is a finely tuned biochemical process in the body. This is confirmed by the normally acidic pH environment of gastric juice (its main component is hydrochloric acid), but also by the difference in acidity parameters in its different parts. High acidity (pH 1.0-1.2) is observed in the initial part of the stomach, and low acidity (pH 5.0-6.0) is observed at the junction of the stomach with the small intestine.
The paradox is that in a healthy person, the stomach not only does not digest itself, but also the gastric juice produced by the glands in different parts of the organ has different properties. At the same time, the pH environment in the esophagus is neutral, and in the duodenum (the first section of the small intestine) is alkaline.
An unpleasant, painful sensation in a person with gastritis - heartburn - is primarily the result of a violation of the acid-base balance in one of the sections of the gastrointestinal tract. In addition, deviation of the acid balance from the norm in certain parts of the stomach underlies the pathogenesis of gastritis with low or high acidity.
Severe effects on the digestive process: food or chemical poisoning, release of bile into the stomach, intestinal infections, regular intake of certain medications, carbonated drinks, alcohol and other factors negatively affect the condition of the gastric mucosa. The serious influence of microbial factors on the development of gastritis has been proven.
Short-term emergency effects on the digestive process are limited to clinical manifestations in the form of acute inflammation of the following nature:
- Catarrhal;
- Fibrinous;
- Necrotic;
- Phlegmonous.
Catarrhal gastritis is associated with poor nutrition and mild food poisoning. Fibrinous and necrotic gastritis are usually caused by poisoning with salts of heavy metals, concentrated acids and alkalis. Phlegmonous gastritis is caused by traumatic damage to the stomach wall.
Long-term exposure to a weakened body ends with the development of chronic pathogenesis, aggravated by ulcerative processes on the walls of the stomach. Gastritis can be a harbinger of oncological processes in the gastrointestinal tract.
The variety of manifestations of gastritis of the stomach in humans is confirmed by their complex classification. Detailing the clinical symptoms of gastritis is extremely necessary for gastroenterologists when prescribing treatment procedures. In our case, this is an illustration of various forms of the disease to give the reader a general idea of gastritis.
The causes of gastritis can be the microbes Helicobacter pylori and others. In some cases, specific microorganisms provoke approximately 80% of gastritis. Helicobacter is not the only cause of this disease.
Another group of gastritis is not associated with microbes, although at certain stages this connection may appear.
Non-microbial gastritis is divided into several groups:
- Alcoholic. The disease develops under the influence of regular consumption of strong alcoholic drinks (alcohol has an alkaline pH) against the background of numerous other factors associated with the general negative effect of large doses of ethyl alcohol on the body;
- NSAID-induced gastritis. NSAIDs are non-steroidal anti-inflammatory drugs that are used for many diseases as antipyretic, analgesic and antiplatelet drugs. The most well-known drugs of this pharmacological group are acetylsalicylic acid (aspirin), analgin, diclofenac, indomethacin, ketoprofen, ibuprofen, piroxicam. Uncontrolled use of NSAIDs stimulates the development of gastritis, and then its transformation into gastric ulcer.
- Post-resection. This type of gastritis develops after forced surgical removal of part of the stomach.
- Chemically caused gastritis. They develop as a result of accidental or special ingestion of chemicals that have aggressive properties against the proteins of the mucous membranes of the stomach.
- Gastritis of unknown origin.
In professional medicine, other classifications of gastritis are also used, including according to the type of distribution of pathogenesis:
- Autoimmune gastritis (type A);
- Exogenous gastritis (type B), provoked by Helicobacter pylori;
- Mixed gastritis (type A+B);
- Gastritis (type C), provoked by NSAIDs, chemical irritants or bile;
- Special forms of gastritis;
- Gastritis against the background of decreased and increased secretion of hydrochloric acid;
- Other forms of morphological and functional manifestations of gastritis.
Their differentiation involves the use of complex medical laboratory or instrumental techniques at the stage of diagnosing the disease. Therefore, a description of gastritis, which has approximately the same clinical symptoms, but differs in the underlying mechanisms of pathogenesis, is not of interest to a wide range of readers.
Let us dwell in detail on the main signs and symptoms of gastritis, which may serve as the basis for a person to contact a medical institution for help.
Features of gastritis with low acidity in children
In children, the disease manifests itself as intense abdominal pain, which is diffuse and appears after eating any food. Palpation in the epigastric region is painful. In addition, signs of gastritis with low acidity in children are nausea and vomiting that occurs several hours after eating, and intolerance to certain foods. Children become easily excitable and emotionally unstable.
In children, gastritis with low acidity is manifested by nausea and vomiting after eating certain foods
In this age group, superficial gastritis predominates; damage to the glands is possible, but the atrophic process usually does not develop.
Diagnostics
The diagnosis of gastritis with low acidity is made on the basis of complaints, medical history, as well as the results of instrumental and laboratory tests. An ultrasound of the abdominal organs is performed, as well as an endoscopic examination - esophagogastroduodenoscopy, during which pH measurements and biopsy are also performed. Measuring the acidity of gastric contents, or pH-metry, can reliably establish a decrease in the production of hydrochloric acid and pepsin.
In the general structure of gastrointestinal pathology, the share of chronic gastritis is 90%, of which gastritis with low acidity accounts for about 25%.
If it is impossible to perform gastric intubation, a laboratory determination of the content of uropepsinogen in the urine is performed. To identify the atrophic form of gastritis with low acidity, the levels of pepsinogen I and II and their relationship to each other are determined in the patient’s blood. Atrophic gastritis is determined in approximately 85% of cases of a pronounced decrease in the level of pepsinogens. Markers of autoimmune pathology (anti-parietal antibodies and antibodies to Castle factor) are determined.
pH-metry for gastritis allows you to measure the acidity of gastric contents
Detection of Helicobacter pylori in gastritis with low acidity can be carried out using polymerase chain reaction, enzyme immunoassay, urease breath test for Helicobacter, etc.
Differential diagnosis is carried out with stomach cancer, pellagra (vitamin PP deficiency), sprue (impaired absorption of fats, glucose and vitamins in the gastrointestinal tract), hiatal hernia, dyskinesia of the gallbladder and biliary tract.
What is stomach acidity, acidity norm
Stomach acidity is defined as the concentration of hydrochloric acid in the gastric juice; it is measured in pH units. When a patient complains of digestive problems and stomach pain, the first thing a gastroenterologist suggests is an FGSD and an analysis of gastric juice to determine the condition of the gastric mucosa and the acidity of gastric secretions. What happens in the stomach, why is it necessary to have normal acidity in the stomach? For digestion to occur properly, enzymes are required, the main one being pepsin, which is produced and functions only in an acidic environment. However, in order for the contents of the stomach to enter the intestines for further high-quality absorption, neutralization of this acid is required. Therefore, there are 2 zones in the stomach, in one acid is formed - this is the body and bottom of the stomach, in the other it is neutralized - this is the antrum of the stomach. This is taken into account when studying the concentration of acid in gastric juice.
Everything in the body is interconnected and complex, and the slightest disturbances in the processes occurring in the stomach result in disturbances in the entire digestive process. The cells of the fundic glands that produce hydrochloric acid in the body and bottom of the stomach are called parietal, and they produce acid with the same intensity and consistency.
A change in acidity can only occur if these cells die (low acidity) or their number increases (high acidity), and also if the degree of neutralization of acid in the antal region of the stomach changes. When the cells become fewer and fewer, gradual atrophy of the fundic glands occurs, which increases the risk of developing atrophic gastritis. This is a serious diagnosis that increases the risk of developing stomach cancer, so the patient should be carefully monitored by a gastroenterologist.
Treatment of gastritis with low acidity
Treatment of gastritis with low acidity is complex and selected individually depending on the form of the disease, the severity of secretory insufficiency, the presence of concomitant diseases and complications. The objectives of treating gastritis with low acidity are:
- elimination of inflammation;
- stopping the progression of atrophic processes in the gastric mucosa;
- restoration, as far as possible, of the motor and secretory functions of the stomach.
Treatment of the disease is usually carried out on an outpatient basis, but in some cases (severe symptoms, the need for careful diagnosis) hospitalization may be required.
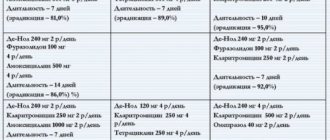
To eradicate Helicobacter pylori, antibacterial drugs are used, as well as proton pump inhibitors (in an anacid state characterized by pH ≥ 6, proton pump inhibitors are not prescribed).
Antibiotics are used to eradicate Helicobacter pylori
According to indications, gastroprotectors, enveloping and astringent drugs, agents that stimulate acid formation, and vitamin and mineral complexes are used. Replacement therapy for gastritis with low acidity consists of taking natural gastric juice and gastric enzymes.
The main treatment of chronic gastritis with low acidity can be supplemented with physiotherapy (UHF therapy, magnetic therapy, inductometry, electrophoresis with drugs, ozokerite and paraffin applications, etc.).
Diet for gastritis with low acidity
One of the main methods of treating gastritis with low acidity is diet therapy. The success of drug therapy largely depends on how well it is followed.
Fractional meals are recommended - meals at least 5-6 times a day at approximately equal intervals, in small portions. Food should be at a comfortable temperature (warm), since cold or hot food has an irritating effect on the gastric mucosa. Dishes are prepared using dietary methods (boiling, steaming, baking or stewing).
A gentle diet is the main method of treating gastritis with low acidity
The diet should include fermented milk products, cereals, lean fish and meat, vegetable and meat soups, pasta, eggs, vegetables, fruits, fruit juices, tea with lemon. Exclude smoked, fatty, fried foods, confectionery, whole milk, fresh baked goods, cabbage, grapes, carbonated drinks, alcohol.
Gastritis with low acidity develops less frequently than other clinical forms, but more often than others leads to serious complications.
Prevention
It is much easier to prevent a disease than to treat it. In order not to experience all the symptoms and consequences of hypoacid gastritis, you should adhere to the following rules:
- do not abuse alcoholic beverages;
- adhere to a healthy diet;
- avoid hot food;
- take care of personal hygiene, do not drink or eat from someone else’s dishes;
- be regularly examined by a gastroenterologist.
Such a diagnosis does not entail dangerous consequences with the necessary prevention and a healthy lifestyle. A person with this disease should adhere to these recommendations.