Along with ordinary allergic reactions to pollen, the development of a more complex allergic form is observed, which can also affect other organs of the body, often leading to serious negative consequences. This form of allergic disease is called rhinosinusitis based on exposure to allergens (one or more at the same time).
What it is
Vasomotor rhinosinusitis is a narrowing of the nasal cavity that occurs due to swelling of the tissues of the nasal turbinates.
The disease develops due to impaired vascular tone of the mucous membrane. As a result, breathing is significantly impaired.
The lateral surfaces of the nose are fixed on bone structures covered with mucous membrane - the nasal turbinates. A large number of vessels are connected to them.
With this pathology, the saturation of blood vessels is disrupted, and the nasal turbinates swell. This causes a runny nose.
The disease in some cases is defined as vasomotor-allergic rhinosinusopathy or angioedema. The disease can occur due to pathologies such as curvatures, polyps and adenoids.
Kinds
The name “rhinosinusitis” is rarely used by ENT doctors of the old, post-Soviet school. In domestic otorhinolaryngology, it is customary to divide the inflammatory process according to its localization:
- Nasal cavity – rhinitis;
- Maxillary sinus – sinusitis;
- Frontal sinus – frontal sinusitis;
- Wedge-shaped – sphenoiditis;
- Ethmoid sinus – ethmoiditis.
This division facilitates the classification of the disease according to ICD-10, structures the treatment, but does not take into account the fact that with inflammation in one sinus, one way or another, all paranasal sinuses and the nasal cavity are involved in the infectious process. Symptoms and treatment of chronic rhinosinusitis in adults depend mainly on the type of disease.
The following types of pathology can be distinguished:
- Purulent;
- Hyperplastic: cystic, polypous, cystic-polypous;
- Purulent-hyperplastic;
- Edema (with chronic or vasomotor rhinitis).
There is no single ICD-10 code for chronic rhinosinusitis. The nomenclature depends on the type of process.
Causes
The disease is based on a change in the excitability of the central and peripheral parts of the autonomic nervous system, which is why the mucous membrane reacts excessively even to normal stimuli.
The answer is a pronounced edematous-secretory reaction, which does not occur in healthy people.
Morphological changes in the epithelium lead to disruption of the activity of the ciliated epithelium and its transport function. The disease may be a manifestation of vegetative-vascular dystonia.
The following factors contribute to the development of the disease:
- ARVI;
- smoking (including passive smoking), inhalation of polluted air, strong odors;
- drinking alcohol;
- sudden changes in temperature;
- cold air;
- stressful situations;
- chronic stomach diseases;
- damage to the nose;
- anatomical disorders of the structure of the nose (curvature, etc.);
- hormonal fluctuations;
- taking certain medications;
- frequent use of nasal drops.
If the cause of the disease cannot be determined, we speak of idiopathic rhinosinusitis. Vasomotor rhinosinusitis can be combined with allergic rhinitis and other nasal diseases.
Photo: Location of the sinuses
Etiology
In most clinical situations, rhinosinusitis was preceded by an acute respiratory infection (influenza, adenovirus or parainfluenza), which was not fully treated. As a consequence, this led to disruption of mucociliary clearance and the functioning of cilia that carry the produced mucus outside the nose. The secretion stagnates, and pathogenic microorganisms begin to actively multiply in it. This is the main reason for the progression of the disease.
Causative agents of rhinosinusitis:
- bacterial agents such as Pseudomonas aeruginosa, streptococcus, staphylococcus, etc.;
- fungi from the genus Candida or Aspergillus;
- mold fungi.
Reasons for the development of the disease:
- bronchial asthma;
- decreased body reactivity;
- viral infections;
- fungal pathologies;
- pathologies of bacterial nature;
- long-term consumption of certain groups of pharmaceuticals;
- burdened heredity;
- mechanical injuries of the nose of varying severity;
- nasal polyposis in adults.
Forms
There are allergic and neurovegetative vasomotor rhinosinusitis. The disease can have a seasonal or permanent form.
Additional classification:
- reflex (reflex reaction of blood vessels to various stimuli):
- vasomotor food (symptoms occur after ingesting hot or spicy food, alcoholic drinks, allergies to certain foods are not noted);
- cold (symptoms occur when the face and limbs are overcooled, manifestations of a runny nose in the cold are excessively expressed);
- rhinosinusitis under the influence of other factors (bright sunlight, strong odors, etc.);
- medicinal (occurs while taking certain medications):
- long-term (longer than two weeks) use of nasal drops and sprays;
- taking antihypertensive drugs;
- hormonal (occurs due to hormonal imbalances):
- rhinosinusitis with reduced thyroid function (impaired hormone production due, for example, to a lack of iodine);
- rhinosinusitis due to pituitary tumor;
- idiopathic (reasons not established).
In addition, acute and chronic vasomotor rhinosinusitis are distinguished. The latter can lead to asthma. In the acute form, both sides of the nasal cavity are affected, the symptoms in this case are pronounced.
Varieties
Types of rhinosinusitis
Clinicians use a classification based on etiology, course, severity, and localization of inflammation.
By etiology:
- mixed;
- viral;
- bacterial;
- fungal.
By localization of inflammation:
- unilateral;
- double-sided
With the flow:
- spicy;
- chronic;
- recurrent.
According to the severity of the pathology:
- light form;
- medium-heavy;
- heavy.
Symptoms
A typical sign of any form of this pathology is weakness and decreased performance.
Headaches and sleep disorders may occur, and appetite decreases.
Symptoms:
- decreased sense of smell;
- stuffiness and runny nose, worsening under certain circumstances;
- labored breathing;
- constant sneezing;
- nasal voice;
- mucous and watery discharge from the nose.
Impaired breathing is associated with difficult ventilation of the lungs, which leads to slower blood flow in the brain and cardiovascular system.
Classification
Clinicians use several classifications of chronic rhinosinusitis, which are based on the localization of the pathological process, its prevalence, and the type of inflammation. Classification according to the type of causative agent of the pathological process is also important.
By localization:
- chronic ethmoidal rhinosinusitis or ethmoiditis - the ethmoid sinuses become inflamed;
- chronic maxillary rhinosinusitis - the inflammatory process affects the maxillary sinuses;
- frontal sinusitis - the mucous membrane of the frontal sinuses becomes inflamed;
- sphenoiditis - the sphenoid sinuses are affected.
By prevalence:
- chronic hemisinusitis. In this case, all sinuses located on one side of the face are affected;
- chronic sinusroethmoiditis. The inflammatory process covers the ethmoid and maxillary sinuses;
- chronic pansinusitis. The inflammatory process affects all sinuses at once;
- chronic polysinusitis. Its progression is indicated if inflammation is observed in several sinuses at once, localized on different sides of the nose.
Structure of the sinuses and air circulation
By type of inflammatory process:
- chronic catarrhal rhinosinusitis;
- chronic purulent rhinosinusitis. Characterized by the presence of periods of exacerbation with the release of purulent exudate;
- chronic polypous rhinosinusitis. A characteristic feature is the growth of outgrowths (polyps) in the sinuses;
- chronic cystic rhinosinusitis. Cystic formations form in the sinuses, inside which exudate accumulates.
Depending on the pathogen:
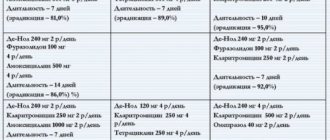
- bacterial rhinosinusitis. Progresses due to the pathogenic activity of bacterial agents. Treatment of this form of pathology is carried out using antibacterial drugs;
- fungal rhinosinusitis. The pathology begins to progress due to the pathogenic activity of fungal microorganisms. It is worth noting that with this type, a mycetoma is formed in the sinus - a specific dense fungal body. In this case, the treatment plan must include antifungal pharmaceuticals.
Chronic allergic rhinosinusitis deserves special mention. It is seasonal and completely independent of the activity of microbial agents. The main reason for its progression is exposure to various allergens (fungal spores, pollen, wool, etc.) on the body. A characteristic feature of allergic rhinosinusitis is that, together with inflammation of the sinus mucosa, rashes appear on the skin and the eyes turn red.
Diagnostics
The diagnosis of vasomotor rhinosinusitis is made after excluding other chronic nasal diseases.
The doctor collects anamnesis: asks about complaints (periodic congestion, discharge, whether symptoms are related to the weather, certain foods, etc.).
The following is a general inspection:
- signs of VSD are revealed:
- blue skin on the hands;
- coldness of the hands and tip of the nose;
- increased sweating;
- low temperature;
- decrease in heart rate;
- low pressure;
- fatigue and drowsiness;
- examination of the nasal cavity:
- enlargement of the nasal concha;
- swelling of the mucous membrane;
- bluish tint of the mucous membrane;
- Allergen samples are taken.
The diagnosis can be confirmed using a blood test.
The detection of eosinophils in the blood and nasal mucus indicates an allergic form of the disease, which is often combined with bronchopulmonary pathologies.
Read what eczema on the legs is. Is nummular eczema dangerous? The answer is in the article.
Diagnostic measures
Diagnostics includes the following activities:
- Rhinoscopy - examination of the nose with a rhinoscope: hyperemia and swelling are detected; discharge occurs during exacerbations. The area of the anastomosis contains pus.
- Examination of the nasal cavity with an endoscope allows you to examine the farthest corners of the nose and identify abnormalities.
- X-ray of the facial part of the skull in 2 projections. The inflammation appears as a darkened area in the affected sinus. With different degrees of inflammation, the darkening will be different. The ethmoidal and sphenoidal sinuses are poorly identified by x-ray.
- CT is today the main method in diagnosing rhinosinusitis. Not performed during exacerbations. The images are taken layer by layer; they reveal the extent of the process and anatomical features.
- In case of exacerbation of inflammation, a puncture (puncture) of the maxillary sinus is performed for diagnostic purposes; if it is purulent, the sinus is washed with antiseptics and local antibiotics are injected into it.
- Ultrasound - as an alternative to x-rays;
- When pumping out exudate without a puncture (YAMIK procedure), it is sown on a nutrient medium to determine the type of pathogen and its sensitivity to various antibiotics.
Treatment of vasomotor rhinosinusitis
Therapy is aimed at strengthening the vessels of the mucous membrane and normalizing blood circulation. During treatment, it is necessary to correct the impaired function of the mucous membrane.
Therapeutic measures include:
- identification and elimination of provoking factors (for example, exclusion of a number of products, alcohol, tobacco smoke, etc.);
- treatment of gastrointestinal diseases (chronic gastritis, GERD);
- moderate physical activity (light jogging and walking) – helps improve the functioning of the autonomic nervous system);
- taking a contrast shower;
- use of medications:
- antiallergic nasal sprays;
- corticosteroid sprays;
- drops and sprays that help reduce secretions (contain ipratropium bromide);
- vasoconstrictor drops and sprays (short-term use);
- rinsing the nasal cavity with saline solutions and special compounds;
- acupuncture;
- hardening (baths for feet and hands with a gradual decrease in temperature);
- physiotherapeutic procedures (ultrasound, magnetic field, electrophoresis, etc.).
In Russia, nasal blockades with hydrocortisone and other hormonal drugs are traditionally used.
Substances are injected into the tissue of the nasal cavity, resulting in the formation of a depot of hormonal medication that has an anti-inflammatory and decongestant effect.
This is a common technique, but it can cause complications.
If conservative treatment does not give the desired result, minimally invasive intervention is performed on the choroid plexuses of the nasal cavity.
Surgical correction of anatomical abnormalities (eg, curvatures) may also be indicated.
Prevention
Preventive measures include:
- minimizing and eliminating contacts with provoking factors (excluding certain foods, alcohol, smoking, etc.);
- correction of nasal anomalies (deviated septum, etc.);
- treatment of gastrointestinal diseases;
- regular exercise, daily walks;
- refusal or reduction in the use of vasoconstrictor drops;
- timely contact a specialist for any manifestations of the disease.
List of sources
- Selkova E.P., Radtsig E.Yu., Bugaychuk O.V., Malygina L.V., Lapitskaya A.S., Gudova N.A., Grenkova T.A. Respiratory viruses in the etiology of rhinosinusitis and acute purulent otitis media in children. Epidemiology and Infectious Diseases. 2015, no. 3, p. 21-23.
- Karpova E. P., Vagina E. E. The role of nasal decongestants in the complex treatment of acute rhinosinusitis in children // Medical Council. 2013, no. 1, p. 46–48.
- Lopatin A. S., Svistushkin A. M. Acute rhinosinusitis: etiology, pathogenesis, diagnosis and principles of treatment. Clinical recommendations. M., 2009. 25 p.
- Ryazantsev S.V., Kocherovets V.I. Etiopathogenetic therapy of diseases of the upper respiratory tract and ear. Guidelines. St. Petersburg, 2008. 120 p.
- Kryukov A.I., Studeny M.E., Artemyev M.E., Chumakov P.L., Rynkov D.L., Gorin D.S. Treatment of patients with rhinosinusitis: possibilities of conservative and surgical treatment. Medical advice. 2012;11: 52-56.
Forecast
The following options for the development of the disease are possible:
- cure with effective therapy or elimination of the cause that caused the exacerbation of the disease is the most expected outcome;
- transition to the chronic stage, periodic repetition of attacks;
- complications of vasomotor rhinosinusitis.
Complications may be as follows:
- swelling of the mucous membrane can cause acute rhinosinusitis (inflammation of the paranasal sinuses);
- breathing problems and, as a result, sleep disturbances, decreased performance and concentration, headaches, fatigue;
- breathing problems during sleep – increases the risk of developing sleep apnea with respiratory arrest and oxygen deprivation;
- prolonged use of vasoconstrictor drops can lead to drug dependence and the development of drug-induced rhinitis, which is difficult to treat;
- chronic hypertrophied rhinosinusitis is an irreversible proliferation of tissue in the nasal cavity.
Polypous rhinosinusitis
Formation of polyps in rhinosinusitis
The progression of polypous rhinosinusitis is more common in people whose body reactivity is significantly reduced. It is also worth noting the fact that in the course of various studies, scientists have found that the risk of developing pathology is higher in patients who have a reduced concentration of immunoglobulin G.
The mechanism of development of polypous rhinosinusitis is as follows:
- under the influence of viral agents, allergens and aggressive chemicals. substances, the mucous membrane swells;
- Gradually, the epithelial tissues thicken, and specific growths - polyps - form on them.
In this case, there is only one treatment - surgery. But it is worth immediately noting that most often surgical intervention causes an exacerbation of the disease and can provoke attacks of suffocation. But it is still necessary to carry out it in order to make nasal breathing easier for the patient.