- Home /
- Branches /
- Rheumatology /
- Hemorrhagic vasculitis
- At the Yauza Clinical Hospital, laboratory (coagulogram, increased levels of the enzyme antistreptolysin-O, IgA) and instrumental (biopsy) research methods are used to diagnose hemorrhagic vasculitis (Henoch-Schönlein disease, purpura).
- Based on the results of the examination, as well as taking into account the clinical picture of the disease, the rheumatologist will develop an individual treatment regimen for the patient, if necessary, using innovative methods of extracorporeal hemocorrection.
- 140 cases per 1 million population - incidence rate of hemorrhagic vasculitis
- More than 60% of cases of hepatitis in adults are accompanied by involvement of the joints, 50% of the kidneys, and 65% of the digestive tract.
- In 95% of cases, timely treatment of Henoch-Schenelein disease contributes to the patient’s complete recovery
sign up for a consultation
General information
Hemorrhagic vasculitis in adults and children (synonyms - Henoch-Schönlein disease, allergic purpura, capillary toxicosis, Henoch hemorrhagic purpura) refers to systemic diseases affecting predominantly the microvasculature of the skin, gastrointestinal tract, joints, and kidneys.
The most affected part of the vascular bed includes small-caliber vessels - post-capillary venules, capillaries and arterioles with the deposition of immune complexes. The ICD-10 code for hemorrhagic vasculitis is D69.0. In 2012, the nomenclature of vasculitis was revised and Henoch-Schönlein purpura received the name IgA vasculitis, that is, vasculitis with deposition of IgA-dominant immune complexes in the vessel wall, affecting small vessels. The disease occurs in all age groups in adults, but the peak incidence occurs in children (3-8 and 7-11 years), averaging 13-18 cases/100 thousand population. Children under 3 years of age rarely get sick, which is obviously due to low immunological reactivity and the sensitization of their body has not yet taken place. The higher incidence of school-age children is due to an increase in the level of sensitization in this age period and the intensity of allergic reactions. As you get older, the incidence decreases, and after 60 years it is extremely rare. The male gender predominates in the morbidity structure (2:1). In the winter and spring periods, the incidence is higher, which is explained by a decrease in the body's reactivity during this period, an increased incidence of ARVI and intensive contacts in children's organized groups.
The specificity of the disease is the variety of clinical manifestations (skin rashes, abdominal pain, articular syndrome, kidney damage, etc.), which often at the onset of the disease leads to a visit to doctors of various specializations (local pediatrician, dermatologist, nephrologist, surgeon, neurologist), untimely diagnosis and delay of adequate treatment, thereby contributing to the development of complications and worsening prognosis.
Signs of the disease
Let's consider the stages and first symptoms of hemorrhagic vasculitis. With the skin type, first of all, starting from the lower leg to the foot, rashes of a reddish hue appear, then they can become more active up to the gluteal region; when pressed, the spots do not disappear, unlike a common allergic reaction.
Read here: Dermatofibroma - what it is, why it appears and how it is treated with modern methods. Tips and recommendations from doctors for removing formations (100 photos + video)
With a mild course of the disease, the temperature does not rise, the rash covers small areas of the skin. The disease can manifest itself more aggressively, at first you will feel unwell, have a headache, have an upset stomach and the temperature will rise to 38C, and a rash will cover a large area of the body.
Severe vasculitis is expressed by the symptoms described above, to which may be added a disorder of the heart muscle, kidney damage, severe pain in the joints, and even the possible appearance of vomit with blood.
Pathogenesis
The mechanism of development of hemorrhagic vasculitis (HV) is based on a generalized immunocomplex necrotizing lesion of the blood vessels of the microvasculature of the skin and internal organs with the formation/deposition of granular IgA deposits (antigen-antibody complexes) in the vascular wall and activation of the complement system. As a consequence, a protein membrane attack complex is formed, which underlies the osmotic lysis of endothelial cells.
Also, when the complement system is activated, chemotactic factors are actively released. affecting polymorphonuclear leukocytes, which in turn secrete lysosomal enzymes that aggravate damage to the vascular wall. As a result of damage to the structure of the vascular endothelium, collagen fibers are exposed, which promotes the adhesion of platelets to the surface of the endothelium and the initiation of the blood clotting mechanism. Subsequently, fibrin deposits form in the vessels, blood rheology worsens, aggregation of erythrocytes and platelets , and intravascular disseminated blood coagulation develops.
Against the background of increased vascular permeability and the development of thrombosis with subsequent depletion of the anticoagulant (antithrombin-III) link and thrombocytopenia of consumption, ruptures of blood vessels of the microvasculature of the skin and internal organs occur, which lead to the development of clinical symptoms of hemorrhagic syndrome. The pathogenesis of hemorrhagic vasculitis is schematically presented in the figure below.
Pathogenesis of hemorrhagic vasculitis
Forms
Hemolytic anemia can be divided into congenital and acquired.
- Congenital - increased breakdown of erythrocytes (red blood cells) is associated with their genetic defect: erythrocyte membranopathy - increased breakdown is associated with a genetically determined defect in their membrane;
- enzymopathies (enzymopathies) - increased breakdown of red blood cells is associated with a deficiency in the activity of erythrocyte enzymes, most often glucose-6-phosphate dehydrogenase (G-6-PD);
- hemoglobinopathies are anemia associated with a genetically determined change or disturbance in the structure of the hemoglobin protein (iron-containing protein of red blood cells, which carries out the function of cell respiration).
- red blood cell membrane defect (a rare disease characterized by the breakdown of red blood cells mainly during sleep);
Classification
There is no single generally accepted classification of HS. The most commonly used clinical classification of the disease is based on one or another clinical syndrome. Accordingly, cutaneous, articular, renal, abdominal and mixed forms are distinguished.
According to severity they are distinguished:
- mild: few rashes; general condition is satisfactory; arthralgia ;
- moderate: profuse rashes, general condition of moderate severity, arthritis , arthralgia , microhematuria , periodic abdominal pain, slight proteinuria ;
- severe: profuse confluent rashes, severe general condition, angioedema , gross hematuria , persistent abdominal pain, nephrotic syndrome , gastrointestinal bleeding , acute renal failure .
According to the nature of the course: acute form (1-2 months), protracted (up to 6 months), chronic with frequent relapses.
Causes of hemorrhagic vasculitis
The causes of hemorrhagic vasculitis in adults have not yet been fully elucidated, however, in most cases, hemorrhagic vasculitis is of an infectious-allergic nature. Among the leading factors contributing to the development of the disease are:
- Infectious factor. Statistics show that in 60-80% of cases, hepatitis B is preceded by an upper respiratory tract infection. At the same time, the range of infectious agents is quite wide: Yersinia , streptococci , mycoplasmas , legionella , hepatitis viruses, respiratory syncytial virus , adenoviruses , Epstein-Barr , cytomegalovirus and others.
- The presence of foci of chronic infection ( tonsillitis , caries , adenoiditis , sinusitis , etc.).
- Taking medications (sulfonamide drugs, penicillin , ampicillin , erythromycin , antiarrhythmic and other drugs).
- Ingestion of potentially allergenic foods (chocolate, eggs, citrus fruits, dairy products, fish, strawberries, wild strawberries, etc.).
- Vaccination/serum administration.
- Insect bites.
- Excessive insolation/hypothermia.
There is also evidence of a genetic predisposition to hepatitis B, which is caused by deficiency of complement C7, as well as the presence of antigens A1, A2, A10, C3HLA Bw35, B8. Thus, in conditions of sensitization of the body, any etiologically significant factor listed above can be decisive in the development of hemorrhagic vasculitis. However, in a significant number of cases, the causes of capillary toxicosis cannot be determined.
Traditional methods of therapy
Treatment of hemorrhagic vasculitis at home with folk remedies is possible only on the recommendation and under the systematic supervision of the attending physician. During treatment the following can be used:
- Collections of herbs and fruits high in vitamin K: a mixture of yarrow with nettle, shepherd's purse, as well as the use of rose hips and black currants.
- In case of severe disease, an internal method of collecting herbs is recommended: sophora, elderberry flowers, yarrow, knotweed. The herbs are mixed in equal proportions, poured with boiling water and taken a tablespoon three times a day.
- As a supplement, you can use an alcoholic infusion of ginseng, eleutherococcus, and licorice root.
Symptoms of hemorrhagic vasculitis
Clinical symptoms of Henoch-Schönlein disease are represented by four typical clinical syndromes: skin, articular, abdominal and renal. The number of organ manifestations of the disease most often varies from 1 to 2 of all classical clinical syndromes, which can develop in various combinations and in any sequence throughout the entire period of the disease. In rare cases, damage to other organs may occur: lungs, central nervous system, heart.
The onset of breastfeeding is often preceded by a prodromal period lasting from 4 to 12 days. In most cases, within 1-4 weeks the patient suffers from a disease, more often a sore throat , acute respiratory viral infection, exacerbation of a chronic disease, or has a history of allergic exposure (taking medications, vaccinations, exacerbation of an allergic disease). Clinical symptoms of this period are not specific and often manifest as general malaise, fever, headache, and loss of appetite.
The onset of hepatitis can develop gradually, when the first symptoms of purpura appear gradually against the background of the patient’s well-being and complete health and the general condition of the patients does not significantly affect. This type of onset of the disease is typical for isolated skin lesions. However, in some cases the disease begins acutely.
Hemorrhagic purpura can begin with any syndrome, but more often the onset of the disease is manifested by cutaneous hemorrhagic syndrome, which is gradually joined by lesions of other systems and organs.
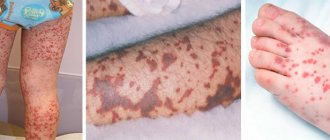
Skin syndrome (form). Skin lesions are observed in all patients with hepatitis B and are a mandatory and most important diagnostic criterion. Typical localization of skin rashes: lower extremities - mainly legs and feet. Less commonly, the rash spreads to the thighs, torso, buttocks, upper limbs, and extremely rarely to the face. Hemorrhagic rash in most cases is represented by purpura , petechiae or a polymorphic rash , less often - urticarial, erythematous-macular elements or a bullous-necrotic form. The photo below of hemorrhagic vasculitis in adults shows various forms of skin syndrome.
Forms of skin syndrome of hepatitis B: a) hemorrhagic, b) urticarial; c) papulo-ulcerative; d) necrotic-ulcerative; e) polymorphic
Cutaneous hemorrhagic syndrome has a number of specific features. The rash is symmetrical, has a small-spotted/petechial character, while the size of the rash elements is 2-5 mm, protrudes above the surface of the skin, does not disappear with pressure, is prone to recurrence and fusion, has a pronounced variegation of rash elements due to the proximity of newly formed ones to old ones, which are at various stages of reverse development, are localized predominantly on the extensor surfaces of the limbs around the joints. Quite often, the onset of the disease is accompanied by various types of allergic rash - urticaria (allergic vasculitis).
In the early period of hepatitis B, the elements of the rash have a reddish color, but in the process of evolution they quickly acquire a characteristic bluish-purple color, then turn pale and within 3-5 days, as they develop back, they acquire a yellowish-brown tint. In severe cases, with high activity of the pathological process, some of the skin elements undergo necrosis, which is caused by microthrombosis and tissue ischemia. The skin syndrome of hepatitis B is characterized by a wave-like course, most often 2-5 episodes are observed. At the same time, newly appearing rashes can be caused by errors in diet, taking medications, or violation of bed rest. In some cases, the rash is accompanied by itching, and in 30-35% of patients hemosiderosis (residual long-term pigmentation) is observed, accompanied by peeling.
A common form of manifestation of skin syndrome can be angioedemalocalized on the hands, feet and face. In boys, swelling of the scrotum occurs. The tissues in the affected areas are bluish in color and pasty.
Articular form (syndrome). Involvement of joints in the pathological process is second in frequency of occurrence after skin syndrome. Quite often it occurs together with skin syndrome or appears several hours/days after it (cutaneous-articular form). Great difficulties in diagnosing hepatitis B are presented by cases in which the articular syndrome appears primarily, proceeds according to the type of migratory polyarthralgia/arthritis and precedes skin manifestations. Its development is based on impaired vascular permeability, which contributes to the development of swelling of the skin/subcutaneous fat in the area of medium/large joints, mainly the wrist and ankle; hemorrhages are less common. Small joints of the hand and foot are practically not involved in the pathological process.
Clinical changes in the joints are manifested by local hyperemia, increased volume, pain and tenderness on palpation, limitation of movements, and increased local temperature. Less commonly, painful contractures develop. Clinical symptoms develop against the background of an increase in body temperature to febrile levels and persist for 2-5 days, after which they disappear without a trace, leaving no deformities. Often articular syndrome occurs against the background of angioedema .
Abdominal syndrome . It occurs in 50-60% of patients and in a third of them it is preceded by skin syndrome, which significantly complicates diagnosis and is a common reason for surgical intervention. The main clinical sign is severe, sudden, cramping pain in the abdomen, without pronounced localization. The nature of the pain is similar to intestinal colic, more often in the navel, less often in the epigastric/right iliac region, often imitating the characteristic picture of a stomach ulcer , appendicitis , pancreatitis and even acute intestinal obstruction . The pain is often extremely intense, causing patients to take a forced position in bed, rushing about and screaming. The pain syndrome is caused by numerous hemorrhages in the intestinal wall, hemorrhages in the mesentery, hemorrhagic impregnation of the mucous membrane and intestinal wall, which can lead to the formation of areas of necrosis and bleeding. At the peak of pain, false urges with frequent bowel movements, vomiting mixed with blood, and the appearance of fresh blood in the stool are possible.
An objective examination reveals pain on palpation of the abdomen, bloating, however, signs of peritoneal irritation are usually absent. The duration of abdominal syndrome varies from several attacks over 2-3 days to 8-10 “waves” over several months. The syndrome is not constant, and the symptoms are unstable. Often, a relapse of abdominal pain is combined with another wave of skin manifestations.
Against the background of abdominal pain, patients may experience pale skin, a sunken face, a dry tongue, sunken eyes, and fever. With heavy bleeding, there is a high risk of developing acute posthemorrhagic anemia and collapse . Serious complications may include intestinal obstruction caused by the closure of its lumen with a hematoma, intestinal perforation , and peritonitis . The development of abdominal syndrome significantly aggravates the process and aggravates its course, requiring intensive therapy.
Kidney syndrome . Develops in approximately 30-50% of patients. This hepatitis syndrome always develops only after the appearance of a hemorrhagic rash, but it can join the symptom complex at different time periods of the disease. Most often, renal syndrome develops 1-2 months into the disease. There are 2 clinical variants of kidney damage:
- Transient urinary syndrome in the form of micro/macrohematuria or hematuria with moderate proteinuria in combination with other manifestations of the disease and with an undulating course.
- Schonlein-Henoch nephritis: occurs more often with a hematuric form, less often with a form of progressive glomerulonephritis and transition in 25-50% of cases to chronic glomerulonephritis, which sharply worsens the prognosis due to the presence of arterial hypertension/nephrotic syndrome and increases the risk of developing chronic renal failure. Therefore, careful monitoring of urine composition and kidney function throughout the disease is necessary.
The severity of clinical manifestations largely depends on the activity of the pathological process, according to which several degrees of severity of the course of hepatitis B are distinguished:
- Mild degree: skin rashes are not abundant, general condition is satisfactory, body temperature is subfebrile/normal, there are no signs of damage to organs/systems, ESR is up to 20 mm/hour.
- Moderate severity: the skin syndrome is clearly defined, the general condition is moderate, intoxication (weakness, headache, myalgia) and articular syndromes are pronounced, fever (hyperthermia over 38°C), abdominal/renal syndromes are moderate. In the blood - an increase in ESR to 40 mm/hour, an increase in eosinophils, leukocytes, neutrophils, dysproteinemia , hypoalbuminemia .
- Severe degree: the general condition is severe, the symptoms of intoxication are very pronounced (weakness, high fever, myalgia, headache). Almost all the main syndromes are expressed - skin, articular, renal, abdominal (paroxysmal abdominal pain, vomiting mixed with blood); there may be damage to the peripheral nervous system and central nervous system. In the blood there is anemia, severe leukocytosis, neutrophilia, ESR more than 40 mm/hour.
Henoch-Schönlein purpura can also occur with the involvement of other systems (cardiovascular, gastrointestinal tract, central nervous system) and organs (liver, lungs) in the pathological process, however, such variants of the disease are much less common.
Related violations
Common purpura is the most common type of the disease, most often occurring in women over 50 years of age. In the absence of damage, skin lesions occur more often than subcutaneous hemorrhage. However, after surgery or even minor injuries, the fragility of the blood vessels leads to excessive bleeding.
Bleeding may be reduced by short-term therapy with corticosteroids or estrogen in postmenopausal women.
Scurvy , a type of purpura, results from a deficiency of vitamin C in the diet. Symptoms may include:
- General weakness.
- Anemia.
- Looseness of gums.
- A tendency to hemorrhage under the skin and in the mucous membranes that line the mouth and gastrointestinal tract.
Scurvy is rarely found in modern civilizations, except in regions remote from modern living conditions. An improved diet and availability of foods containing vitamin C can help prevent the disease.
Gardner-Diamond syndrome, or autoerythrocyte syndrome , is a rare disorder sometimes called painful bruise syndrome. It is characterized by patches of purpura, mainly in young women. The occurrence of the pathology is associated with an autoimmune disorder.
Vasculitis, or angiitis , is a vascular inflammatory disease that can occur alone or in combination with other allergic or rheumatic diseases. Inflammation of the vascular walls promotes spasm of blood vessels and can cause insufficient blood supply to certain areas of the body (ischemia), tissue death (necrosis), and/or the formation of blood clots (thrombosis). Vessels of any size or any part of the vascular system may be affected. Symptoms relate to the system involved and may include:
- Fever.
- Headache.
- Profound loss of appetite.
- Weight loss.
- Weakness.
- Abdominal pain.
- Diarrhea.
- Pain in muscles and joints.
Since there are many forms of vasculitis, there are plenty of reasons for its development. Some types may be caused by allergic reactions or hypersensitivity to certain drugs, such as penicillin, propylthiouracil, other drugs, toxins, and various inhaled irritants. Some forms may occur due to fungal infection, parasites or viral infections, while in some cases there is no obvious cause.
Cutaneous necrotizing vasculitis is a relatively common inflammatory disease of the blood vessels, affecting veins, arteries and smaller blood vessels (capillaries). This disorder usually affects the skin and can occur alone or in combination with allergic, infectious or rheumatic diseases. The symptoms are:
- Nodes on the skin.
- Small hemorrhages under the skin and/or lesions that may be red and flat (macula).
They can form in many parts of the body, especially on the back, arms, buttocks and/or legs. In some cases, severely itchy hives or ring-shaped ulcers are present. Fever, generalized discomfort (malaise) and/or muscle and joint pain may also occur. The exact cause of cutaneous necrotizing vasculitis is unknown. Some lesions may be caused by an allergic reaction or hypersensitivity to certain medications, such as sulfate or penicillin, toxins, and inhaled irritants.
Kawasaki disease is an inflammatory disease in children characterized by fever, skin rash, swollen lymph nodes (lymphadenopathy), inflammation of the arteries (polyarteritis), and inflammation of the blood vessels (vasculitis). Inflammatory changes cause destructive lesions in the blood vessels, which can lead to complications related to the liver, gallbladder and heart. Symptoms may include:
- An abnormally high body temperature that begins suddenly and lasts for about two weeks.
- Redness of the inside of the eyelids of both eyes (bilateral conjunctivitis).
- Irritability.
- Fatigue.
- Redness (inflammation) of the mouth and tongue (stomatitis).
- Chapped lips.
- Swelling of the lymph nodes in the neck (cervical adenopathy).
- Skin rash.
The exact cause of Kawasaki disease is not fully known. This may be due to two previously unknown strains of staphylococcus and streptococcus bacteria and/or a possible immunological abnormality.
Immune thrombocytopenia is a rare platelet disorder characterized by unexplained low levels of platelets in the circulating blood. Symptoms may include:
- Nosebleeds.
- Small red or purple spots on the skin that represent hemorrhages under the skin (petechiae) and/or bleeding from the rectum and/or urinary tract.
- Anemia can contribute to weakness and fatigue.
- Other people with this disorder have episodes of high fever and an abnormally enlarged spleen.
No specific cause for the development of immune thrombocytopenia is known. Existing data support an immunological basis, as most patients have antiplatelet antibodies that can be identified.
Idiopathic thrombocytopenic purpura (ITP) is a rare blood disorder characterized by abnormally low levels of circulating platelets in the blood, abnormal destruction of red blood cells, kidney dysfunction, and nervous system disorders. Symptoms of this disorder, which begin suddenly, may include:
- Fever
- Headache.
- Purpura spots on the skin and mucous membranes.
- Joint pain (arthralgia).
- Partial loss of sensation in the arms or legs (paresis).
- Change in mental state.
- Cramps.
The exact cause of ITP is unknown. This may be due to an infectious agent or an autoimmune reaction.
Tests and diagnostics
The diagnosis of hepatitis B is made by identifying specific clinical syndromes, first of all, the presence at the time of examination/history of skin hemorrhagic bilateral rashes and establishing a connection between the onset of breastfeeding and infectious diseases, an allergic history, and changes in diet. There are no specific laboratory tests. Laboratory research:
- OAC - thrombocytosis and nonspecific changes common to any inflammatory process, accelerated ESR, leukocytosis.
- OAM—hematuria/proteinuria.
- Biochemical blood test - blood for CRP, liver tests, creatinine, urea.
- Coagulogram - hypercoagulation is noted, accompanied by a decrease in the activity of antithrombin III and plasmin, and a decrease in chlorides.
- Immunogram - an increase in the concentration of IgA in the blood serum.
- Fecal occult blood test (positive for gastrointestinal bleeding).
In confirming the clinical diagnosis, a leading role is played by a skin biopsy and an immunohistochemical study to reveal the fixation of IgA-containing immune complexes in the vascular wall. If necessary, an ultrasound of the kidneys and abdominal organs and an ECG are prescribed.
Differential diagnosis is necessary with vasculitis in autoimmune diseases ( rheumatoid arthritis , Crohn's disease , systemic lupus erythematosus , ulcerative colitis ), vasculitis of infectious etiology, infections (hepatitis B and C, infectious subacute endocarditis , tuberculosis ), drug allergies and malignant neoplasms.
How to prevent exacerbations?
After discharge from the hospital, the patient should not forget about his illness at home. Of course, by that time he will already know everything about the nature of the disease, prevention of exacerbations, behavior in everyday life, nutrition and daily routine. Having immersed himself in a homely atmosphere, the patient will not take any medications without a doctor’s prescription, will not attack foods that can provoke a relapse (allergens), but will eat well and will take quiet, easy walks in the fresh air every evening.
In addition, the following are contraindicated for a person:
- Excessive anxiety, mental stress;
- Vaccinations (possible only for health reasons);
- Hard physical labor (children are exempt from physical education lessons);
- Hypothermia;
- Administration of immunoglobulins (antistaphylococcal, antitetanus, etc.).
Due to the fact that hemorrhagic vasculitis is predominantly a childhood disease, special recommendations are provided for children (or parents?):
- Every six months the child visits the attending physician (in the absence of exacerbations);
- Clinical observation for at least 5 years if the kidneys remain healthy, but if they are damaged, control may be lifelong;
- Children are completely exempt from physical education for a year, then move to the preparatory group;
- A mandatory visit to the dentist and otolaryngologist is required 3 times a year;
- Regular urine tests (general and Nechiporenko) and fecal tests for helminths;
- Vaccinations are excluded for 2 years, and after this time, routine vaccination is carried out, but with the permission of the attending physician and under “antihistamine cover”;
- Compliance with an anti-allergenic diet – 2 years;
Advice to parents or other relatives about treatment at home, relapse prevention, nutrition and behavior at school and at home.
Diet
Hypoallergenic diet
- Efficacy: therapeutic effect after 21-40 days
- Timing: constantly
- Cost of products: 1300-1400 rubles. in Week
Diet Table No. 1
- Efficacy: therapeutic effect after 3 weeks
- Terms: 2 months or more
- Cost of products: 1500 - 1600 rubles. in Week
Diet 7 table
- Efficacy: therapeutic effect after a week
- Terms: 1 month or more
- Cost of products: 1200-1300 rubles per week
A hypoallergenic diet is prescribed, which involves excluding obligate allergens from the diet: milk, fish, citrus fruits, chocolate, cocoa, orange and red vegetables/fruits, as well as extractive substances. For abdominal syndrome, a modified Table No. 1 according to Pevzner is indicated until it is completely relieved. For nephritis - dietary Table No. 7 with a gradual transition to a hypochloride diet.
Therapy
Modern medicine offers comprehensive treatment for hemorrhagic vasculitis. The goal of therapy is to normalize the normal functioning of the affected organs and the immune system, which contributes to impaired blood supply, which in turn destroys blood vessels.
The patient must remain calm and completely limit physical activity. It is also recommended to follow a gentle diet. You should exclude from your diet the consumption of foods that can provoke allergic reactions.
It is recommended to follow a gentle diet
In order to get an accurate answer to the question of how to treat hemorrhagic vasculitis, it is recommended to contact a qualified specialist. Patients ask themselves: which doctor treats this pathology? In this case, you will need to consult a rheumatologist, who will give appropriate recommendations and prescribe an appropriate treatment regimen.
Principles of basic treatment
The basic principles of basic treatment include the following recommendations:
- Take medications that promote an adsorbing effect (activated carbon, Eterosgel, Polyphepan). Such medications have the ability to remove harmful substances and toxins from the body, preventing them from entering the systemic bloodstream.
- Use medications from the group of antiplatelet agents that prevent the formation of blood clots and disrupt the process of platelet adhesion. Taking this group of medications helps improve blood flow even through the smallest vessels.
- The use of antihistamines to help eliminate allergic reactions in the body.
- Antibiotics and antimicrobials.
- Infusion treatment to cleanse the blood and provide a detoxifying and restorative effect.
- The use of corticosteroids (hormonal agents) to provide an anti-inflammatory effect, eliminate swelling, and prevent the development of allergic manifestations.
During treatment, it is recommended to abstain from drinking alcohol and grapefruit juice.
Additional treatment
If necessary, the doctor can supplement the basic treatment regimen:
- The use of cytostatics that suppress the functioning of the immune system.
- The use of drugs from the group of non-steroidal anti-inflammatory drugs. Tablets and capsules have a pronounced anti-inflammatory, analgesic and antipyretic effect.
- Prescribing membrane stabilizing drugs. Vitamin complexes may be prescribed, which include vitamin C and B vitamins, as well as the use of Ascorutin (a combination of rutin with vitamin C). Such substances accelerate regeneration processes, normalize capillary permeability, and strengthen the walls of blood vessels.
In severe cases of the disease and manifestations of severe intoxication, the patient may be recommended to undergo a plasmapheresis procedure. During the procedure, the blood is cleansed of harmful and toxic elements.
Symptomatic treatment is aimed at eliminating complications of the disease. For example, in case of disruption of the normal functioning of the gastrointestinal tract, the patient will be prescribed medications from the group of antispasmodics and drugs that normalize acidity.
As a supplement, it is recommended to perform massage, as well as special therapeutic exercises. Patients who ask: how to do a massage should contact their doctor with these questions and entrust the procedure to a qualified specialist. This will help achieve a better therapeutic effect.
In what cases surgery may be required?
Surgery may be required in the following cases:
- Kidney transplantation in case of serious violations of the normal functioning of the kidneys and the ineffectiveness of drug treatment.
- Excision of affected areas of the intestine, removal of dead tissue.
In most cases, the disease can be cured with conservative treatment methods. Radical therapy may be prescribed to the patient if serious complications develop.
Prevention
The main measures to prevent hepatitis B in its relapses include:
- Adequate treatment of acute infectious diseases of the upper respiratory tract and timely sanitation of infectious chronic foci of ENT organs.
- Exclusion/minimization of contacts with allergens (if there is a history of allergic reactions) and control of medications.
- Preventing hypothermia of the body.
- Strengthening the immune system (hardening, rational nutrition).
- Dispensary observation of ill persons for 2 years.
Consequences and complications
The main complications of hepatitis B include: intestinal obstruction , pancreatitis , perforation , peritonitis , posthemorrhagic anemia , thrombosis / infarction in organs, neuritis , cerebral disorders. The lethal outcome develops mainly as a result of abdominal complications (intestinal perforation, peritonitis), the development of chronic renal failure , and hemorrhages in organs (brain).
Forecast
The prognosis is generally favorable and in 75% of cases patients recover within 1-2 years after the disease. In a number of patients with a chronic relapsing course, the disease can continue indefinitely with periodic relapses of one (skin) or several syndromes. The frequency of relapses throughout the entire period can vary from one to monthly, acquiring a monosyndromic character over time: mainly in the form of cutaneous purpura or a skin-articular form, less often - chronic nephritis in the form of a hematuric form with preservation of kidney function over a long period.
The prognosis is less unfavorable with the development of nephritis , especially when the process becomes chronic with manifestations of glomerulonephritis and transition to chronic renal failure. Purpura fulminans has a poor prognosis.
List of sources
- Lyskina G. A. Systemic vasculitis. In the book: Pediatric rheumatology. Guide for doctors / Ed. A. A. Baranova, L. K. Bazhenova. M.: Medicine, 2002. pp. 221–270.
- Kulaga V.V., Romanenko I.M., Afonin S.L. Allergic diseases of the blood vessels of the skin. Lugansk: “Etalon-2”, 2006. 168 p.
- A practical guide to childhood diseases, edited by prof. Kokolina V.F. and prof. A.G. Rumyantsev, volume IV. Hematology/oncology of childhood (edited by Rumyantsev A.G. and E.V. Samochatova). Medical practice – M. Moscow 2004 Zinovieva G.A., Frolkova E.V. Hemorrhagic vasculitis. Clinic and treatment // ros. pediatrician, journal — 1998. -N12. P.24-26.
- Krivosheev O.G., Gulyaev CB, Semenovykh A.G. Modern principles of treatment of Henoch-Schönlein purpura // Doctor. 2007. No. 4. -P.54-55.