Gestosis (“late toxicosis”) is a complication of pregnancy, accompanied by increased blood pressure, the formation of edema, and headaches. In some cases, swelling does not occur, and the disease is more complicated. During gestosis in pregnant women, protein is found in the urine.
The disease can begin to develop at 16-20 weeks of pregnancy, and is often detected later - at 26-28 weeks. But in most cases, gestosis occurs after the 34th week of pregnancy. The later it develops (the closer to childbirth), the easier its course will be.
With gestosis, malfunctions in the functioning of many organs are observed. But above all, the functioning of the urinary and cardiovascular systems is at risk. In severe cases of gestosis, disorders of the central nervous system (CNS) occur. Pathology can also cause hypoxia (insufficient oxygen supply) in the fetus.
Preeclampsia is a fairly common disorder during pregnancy. It is diagnosed in 20-30% of pregnant women.
What are the signs by which the disease is determined?
Main features
- swelling or dropsy (first the hands and feet swell);
- the appearance of protein in the urine;
- blood pressure is higher than normal.
Dangerous symptoms are warning signs of a seizure attack
- nausea;
- headache;
- stomach ache;
- lethargy and drowsiness;
- flashing “flies” before the eyes.
The combination of such symptoms is characteristic of preeclampsia , which is the result of gestosis. The following conditions may occur against the background of seizures: stroke, heart attack, placental abruption, pulmonary edema, renal failure, placental abruption, retinal detachment. Such complications develop very quickly and can be present in pregnant women of any age.
Preeclampsia is divided into groups, depending on the existing symptoms
1. Edema of pregnant women
They can be obvious or hidden. The latter appear in the early stages of the disease. They arise due to fluid retention in tissues. Self-medication is unacceptable here. Diuretic medications cannot eliminate the problem, but only worsen the condition of the pregnant woman and the fetus. Not all swelling during pregnancy is associated with gestosis. Only a specialist can identify complications.
2. Preeclampsia
This condition most often occurs after the 20th week of pregnancy. Sometimes preeclampsia occurs at the end of the first week after birth. Its symptoms are hypertension, edema and proteinuria. In severe cases, the blood supply to the brain is disrupted. This is manifested by severe headache, vomiting and visual impairment.
3. Eclampsia
This is the most severe form of gestosis. It has a whole range of symptoms, the most dangerous of which are seizures.
Gestosis can manifest itself in different ways. Some women have minimal symptoms. Others suffer from fulminant attacks that have catastrophic consequences.
Eclampsia
Eclampsia is the result of severe damage to all systems and manifests itself as a syndrome of multiple organ failure. More often it develops following the previous form, but can occur suddenly with any severity of nephropathy.
Eclampsia occurs with convulsions, which may be preceded by increased headaches, blurred vision, twitching of the eyelids and facial muscles, anxiety, and mental disorders are possible. Seizures can be triggered by bright light, minor pain or a sharp sound, but often occur on their own either once or in a series of seizures.
Their duration is 1 - 2 minutes, after which a loss of consciousness occurs, which returns slowly, followed by amnesia. Sometimes loss of consciousness occurs without convulsions.
Cause of the disease - Doctors' opinions
Doctors cannot accurately name the reasons that cause gestosis. But there is a clear opinion that such a complication rarely occurs in healthy women. Most often, gestosis develops against the background of existing diseases of the mother. Increased blood pressure, impaired renal or liver function, as well as other somatic diseases are indirect causes of toxicosis in pregnant women.
It is impossible to name the causes of gestosis more precisely. A pregnant woman experiences disruptions in her body that can lead to serious problems. In some cases, doctors resort to early delivery to save the life of the child and mother. Therefore, before conceiving, a woman needs to undergo examination.
This will allow you to predict possible complications that may arise during pregnancy. If necessary, a woman is prescribed a course of treatment even before pregnancy. Immunological diseases, blood clotting disorders, kidney diseases, vegetative-vascular dystonia, anemia, diabetes mellitus - these and many other disorders often lead to gestosis.
If you have problems with your kidneys, thyroid gland or blood pressure, be sure to visit your doctor.
The risk group includes
- women over 30 years of age and under 18 years of age;
- those who frequently had abortions;
- women who have given birth many times;
- those who have a short break between births.
No one is 100% immune from gestosis. Therefore, experts strongly advise you to regularly come for examination. Monitoring blood pressure and weight, blood and urine tests are measures that allow timely detection of complications.
A pregnant woman’s excellent health is not yet an indicator of good health. Sometimes test results show poor results in the absence of external signs of gestosis.
Why does gestosis appear in pregnant women?
Preeclampsia or toxicosis is a complication associated with pregnancy. It may be early or late. Early toxicosis is known to all pregnant women. It manifests itself at the earliest stages. Its main symptoms are nausea and vomiting. Early gestosis usually does not have an aggressive nature.
All its signs are noticed not only by the pregnant woman herself, but also by the people around her. Late toxicosis is more insidious. They are the ones who lead to dangerous complications. Late gestosis is a leading cause of maternal mortality. This complication is less noticeable.
It manifests itself in three main signs:
- swelling;
- protein in urine;
- high blood pressure.
Not all women experience the full range of symptoms. Only one of them can indicate the presence of gestosis. Only swelling is visible here. Pressure rises may not be very significant. In this case, the woman does not feel them. Changes in the composition of urine also do not bother the pregnant woman. Therefore, towards the end of the term, doctors measure blood pressure and weigh in weekly.
Late gestosis sometimes has an unpredictable development. Sometimes they begin to progress dramatically. In this case, the woman’s health condition rapidly deteriorates. A pregnant woman may feel worse and worse every hour. Pathology in this form is treated only in an inpatient setting.
Today, about 27% of pregnant women experience gestosis. Symptoms of the disease subside after childbirth. The complication arises due to the fact that the mother’s body cannot optimally adapt to bearing a child. As a result, various violations arise.
Preeclampsia is characterized by spasm of the smallest blood vessels. As a result, the amount of blood that carries nutrients and oxygen to the cells is sharply reduced. The functioning of organs and systems is disrupted. Spasm of small vessels leads to an increase in blood in large vessels. All this leads to increased blood pressure.
Changes occur in the kidneys, which leads to the appearance of protein in the urine. The brain also suffers. This is manifested by nausea, headaches, and flashing “spots”. If a pregnant woman experiences dry skin and itching, this is a clear sign of changes in the liver.
The woman experiences swelling and the blood becomes thicker. Such processes also affect the condition of the fetus. Its growth and development slows down. The baby experiences a lack of oxygen (hypoxia).
Toxicoses of the first half of pregnancy
Lecture for doctors “Toxicoses of the first half of pregnancy.” The lecture for doctors is given by Dyakova S.M., obstetrician-gynecologist, teacher - total work experience of 47 years.
Toxicosis of pregnant women (preeclampsia) is a pathological condition during pregnancy associated with the development of the fertilized egg, which disappears in the postpartum period. This is a complication of pregnancy, which is a consequence of the insufficiency of the mother’s adaptive capabilities, in which her body cannot sufficiently provide for the needs of the growing fetus. Gestosis is manifested by various disorders of neurohumoral regulation. Disorders of the functions of the central and autonomic nervous systems, cardiovascular and endocrine systems appear, as well as disruption of a number of metabolic processes, immune response, etc. There are early and late toxicoses.
Early toxicosis of pregnant women
It develops in the first 20 weeks of pregnancy and is called toxicosis of the first half of pregnancy . Of the existing many theories of the development of early toxicosis (such as neurogenic, corticovisceral, hormonal, allergic, immune), the theory of disruption of neuroendocrine regulation and metabolism, which develops as a result of previous diseases, characteristics of pregnancy, and the influence of unfavorable environmental factors on the body, is currently adhered to. Early toxicosis of pregnancy is most often accompanied by vomiting and drooling (ptyalism).
Vomiting occurs in approximately 50–60% of pregnant women, but only 8–10% of them require hospital treatment. The appearance of vomiting is associated with hormonal imbalance. The onset of vomiting temporarily corresponds to the peak production of human chorionic gonadotropin. With vomiting during pregnancy, the endocrine activity of the adrenal cortex may change in the direction of reducing the production of corticosteroids. Vomiting of pregnant women can also be regarded as an allergization of the body when trophoblast particles enter the maternal bloodstream. Vomiting is most severe during multiple pregnancies and hydatidiform moles.
There are III degrees of severity of vomiting during pregnancy.
I. Mild degree is characterized by vomiting up to 5 times a day, while the condition of the pregnant woman is not disturbed; vomiting can be associated with food intake or odors or appear on an empty stomach.
II. Moderate severity is accompanied by vomiting up to 10–12 times a day, symptoms of intoxication, weakness, loss of body weight and decreased diuresis.
III. Severe degree (uncontrollable or excessive vomiting) is characterized by repeated vomiting (up to 20 times or more per day), leading to rapid loss of body weight, exhaustion, metabolic changes and dysfunction of vital organs. Severe vomiting is characterized by severe weakness, agitation or apathy, low-grade fever, tachycardia, decreased blood pressure, and the appearance of acetone, protein, and casts in the urine. Often with severe vomiting, jaundice occurs; in rare cases, toxic liver degeneration develops.
Treatment of vomiting of pregnancy of the first degree of severity is carried out on an outpatient basis with monitoring of the dynamics of weight gain of the pregnant woman and regular urine tests for acetone. A diet with frequent, split meals, rinsing the mouth with astringents is prescribed, frequent walks in the fresh air are recommended, and acupuncture is prescribed.
Treatment of vomiting of pregnant women of II and III severity is carried out in a hospital setting. Complex treatment is prescribed, the purpose of which is to normalize the functions of the central nervous system, restore the loss of nutrients and fluid, correct electrolyte balance and acid-base balance. Termination of pregnancy is carried out in case of failure of treatment, with persistent low-grade body temperature, severe tachycardia, progressive loss of body weight, proteinuria, cylindruria, acetonuria, jaundice.
Hypersalivation is often present with vomiting of pregnancy, but can sometimes occur as an independent form of early toxicosis of pregnancy. With severe drooling, saliva loss per day can reach 1 liter or more. Excessive drooling has a depressing effect on the psyche of a pregnant woman, leading to dehydration, hypoproteinemia, sleep disturbance, loss of appetite and body weight. Maceration of the skin and mucous membrane of the lips is sometimes observed. It is advisable to treat hypersalivation in a clinical setting. In this case, atropine and a local infusion of astringent and antiseptic herbs (oak bark, chamomile, sage) are used. Severe hypoproteinemia is an indication for plasma transfusion. Hypnosis and acupuncture are used as auxiliary methods.
A special form of early gestosis is jaundice caused by cholestasis (cholestatic hepatitis). This form of toxicosis occurs rarely, usually occurs at the beginning of the second trimester of pregnancy and progresses as its duration increases. It is characterized by predominant liver damage, often accompanied by itchy skin, increased cholesterol levels and alkaline phosphatase activity in the blood with normal alanine aminotransferase activity. This form of gestosis is often complicated by premature termination of pregnancy, bleeding during childbirth, and the formation of fetal malformations. When pregnancy is terminated, jaundice disappears, but may recur in subsequent pregnancies. Differential diagnosis is carried out with jaundice that occurs during pregnancy due to viral hepatitis, cholelithiasis, body intoxication, hemolytic anemia. Treatment is carried out in accordance with the general principles of hepatitis treatment. A diet, vitamins, glucose, protein preparations, etc. are prescribed. Considering the extremely serious significance of liver damage during pregnancy, primarily for a woman, the question of premature termination is often raised.
Early toxicosis of pregnant women can also be expressed in some forms of dermatosis. The most common is itchy skin. It can appear at the beginning and end of pregnancy, and can be localized and limited to the vulva area or spread throughout the body. Itching can be severe and constant, which worsens the well-being and mood of the pregnant woman. Insomnia and irritability may occur. With this form of toxicosis, it is necessary to exclude diseases accompanied by itchy skin. It is necessary to exclude diabetes mellitus, fungal and parasitic skin lesions, trichomoniasis, helminthic infestation, allergic reaction, etc. Treatment comes down to the prescription of drugs that regulate the functions of the nervous system, desensitizing agents, and UV irradiation.
Occasionally, dermatoses manifest themselves in the form of eczema, herpes, and impetigo herpetiformis. With impetigo herpetiformis, the likelihood of perinatal mortality is high. These dermatoses are treated in the same way as in the absence of pregnancy.
Tetany is one of the rare forms of pregnancy toxicosis. Its cause is a violation of calcium metabolism in pregnant women. A manifestation of this form of toxicosis is the occurrence of muscle spasms of the upper and lower extremities and face. It is also necessary to take into account the possibility of hypoparathyroidism occurring in connection with pregnancy. To treat this form of toxicosis, calcium supplements are used. An even rarer form of early toxicosis in pregnant women is bronchial asthma. It should be differentiated from exacerbation of previously existing bronchial asthma. Treatment includes the prescription of calcium supplements, sedatives, a complex of vitamins, and general ultraviolet radiation.
Pregnant women who have suffered early toxicosis need careful outpatient monitoring, as they often subsequently develop late toxicosis.
Late toxicosis of pregnant women
Toxicoses that develop after 20 weeks of pregnancy are called late or toxicoses of the second half of pregnancy . In the 1990s. this term has been replaced by the term “OPG-gestosis” (edema, proteinuria, hypertension). OPG-gestosis is a syndrome of multiple organ functional failure that occurs as a result of pregnancy. The causes of this pathology have not been sufficiently elucidated to date. The immunological theory explains the occurrence of symptoms of OPG-gestosis by the reaction of the pregnant woman’s body to fetal antigens. In this case, the formation of autoimmune complexes occurs, activating the kinin system. Subsequently, arterial hypertension occurs. In addition, hemocoagulation increases, accompanied by fibrin deposition and impaired blood supply to the placenta and organs of the pregnant woman. The immune theory of the occurrence of OPG gestosis is confirmed by the detection of subendothelial deposits of complement, immunoglobulins G and M in the kidneys of a pregnant woman.
Generalized vasospasm with subsequent or simultaneous development of hypovolemia is important in the development of OPG-preeclampsia. According to most scientists, the primary disorder is the uteroplacental circulation, after which a spasm of peripheral vessels occurs, as a result of which the volume of the vascular bed decreases and hypovolemia occurs.
V.N. Sterov and co-authors believe that there are two main reasons for the development of OPG-gestosis: diffusion-perfusion insufficiency of the uteroplacental circulation and the presence of extragenital pathology in the pregnant woman, primarily circulatory disorders in the kidneys. In both cases, multiple organ failure syndrome occurs with different clinical features and consequences. Mixed forms of OPG-gestosis are possible, in which several systems are affected simultaneously.
For all reasons for the development of OPG-gestosis, dysfunction of the placenta occurs. Uteroplacental perfusion decreases sharply: with full-term physiological pregnancy it is 162 ml/min per 100 g of placental tissue, with OPG-preeclampsia it is only 59 ml/min per 100 g of placental tissue. This is mainly due to a decrease in pulse blood pressure and worsening venous outflow. With a mild course of OPG-preeclampsia, the disturbance in perfusion is eliminated by increased cardiac activity of the pregnant woman and an increase in blood pressure. As the symptoms of OPG-gestosis increase, hypoxia and acidosis develop in the mother’s body. They lead to a continued decrease in uteroplacental perfusion, which can have consequences such as hypoxia, malnutrition and fetal death. Obesity, multiple births, polyhydramnios, stress, and physical exertion are additional factors that contribute to increased disturbances in uteroplacental perfusion. When a woman lies on her back, the uterus presses on the inferior vena cava, which impairs perfusion. Vascular disorders resulting from the development of OPG-preeclampsia disrupt the diffusion capacity of the placenta. The process is also enhanced by the activation of lipid peroxidation. Products of incomplete breakdown of fats cause damage to cell membranes, which leads to a sharp deterioration in gas exchange, disruption of the barrier, filtration and purification, endocrine, immune and metabolic functions of the placenta, in which areas of thrombosis, ischemia, hemorrhage and edema begin to form. As a result of these changes in the placenta, the needs of the fetus are not fully met, and its development is delayed. In the placenta, the synthesis of estrogens and progesterone, which contribute to the normal development of pregnancy, decreases. Basically, disorders of perfusion and diffusion functions are associated with each other. Severe perfusion-diffusion insufficiency of the placenta in severe forms of OPG-gestosis V.N. Sterov and co-authors call placenta shock syndrome .
A more frequent development of OPG-gestosis is observed during repeated births, if its signs were observed in previous pregnancies, as well as in women with diseases of the urinary system, hypertension, and diabetes mellitus.
Clinical picture and diagnosis. Clinical manifestations of OPG gestosis are as follows: significant increase in body weight, the appearance of edema, proteinuria, increased blood pressure, convulsions and coma.
OPG gestosis manifests itself in four clinical forms. These are dropsy, nephropathy, preeclampsia and eclampsia.
Hydrops of pregnant women is expressed in the appearance of severe persistent edema in the absence of proteinuria and normal blood pressure values. At first, edema may be hidden (positive ring sign, McClure-Aldrich test), and excessive weight gain is noted. Next, visible swelling appears in the lower extremities, in the vulva, torso, upper extremities and face. The general condition of the pregnant woman usually does not suffer. Pregnancy in most cases ends with delivery on time. Sometimes pregnancy nephropathy develops.
Nephropathy in pregnant women consists of three main symptoms: proteinuria, edema, and increased blood pressure.
There are III degrees of severity of nephropathy.
I. Edema of the lower extremities, blood pressure up to 150–90 mm Hg. Art., proteinuria up to 1 g/l – I degree.
II. Edema of the lower extremities and anterior abdominal wall, blood pressure up to 170/100 mm Hg. Art., proteinuria up to 3 g/l – II degree.
III. Severe swelling of the lower extremities, anterior abdominal wall and face, blood pressure above 170/100 mm Hg. Art., proteinuria more than 3 g/l – III degree. The onset of preeclampsia and eclampsia can occur with II and even I degree of severity of nephropathy.
When prescribing treatment for nephropathy in pregnant women, it is also necessary to take into account the degree of impairment of the cardiovascular, urinary systems, kidneys, and liver function. The severity of nephropathy is characterized by an increase in diastolic and a decrease in pulse pressure, as well as asymmetry of blood pressure. Further development of gestosis leads to increased hemodynamic disturbances: the volume of circulating blood, central and peripheral venous pressure decreases, cardiac output decreases, peripheral vascular resistance increases, and metabolic changes in the myocardium increase. To accurately determine the degree of proteinuria, daily urinary protein excretion is determined. It increases as gestosis progresses and in severe nephropathy exceeds 3 g. Impaired renal concentration function can be assumed by persistent hypoisosthenuria (specific gravity of urine - 1010–1015) in the Zimnitsky study. As gestosis worsens, diuresis decreases and the nitrogen excretion function of the kidneys decreases (the urea content in the blood reaches 7.5 mmol/l or more).
At the same time, the amount of protein in the blood plasma decreases (up to 60 g/l or less). The development of hypoproteinemia is associated with several reasons, one of them is a violation of the protein-forming and antitoxic functions of the liver and a decrease in colloid-oncotic pressure of the blood plasma. An increase in the permeability of the vascular wall and, as a result, the appearance of protein in the extracellular space can also be causes of hypoproteinemia. The more severe gestosis is, the lower the protein content in the blood plasma. The severity of gestosis is indicated by its early onset and long course, as well as severe thrombocytopenia and fetal malnutrition. In severe cases of nephropathy, there is a high probability of premature placental abruption, premature birth, and intrauterine fetal death. Nephropathy can result in preeclampsia and eclampsia.
Preeclampsia. It is characterized by signs associated with dysfunction of the central nervous system. by type of hypertensive encephalopathy (cerebrovascular accident, increased intracranial pressure and cerebral edema). Excitement of patients is noted, less often drowsiness. Against the background of high blood pressure, a woman experiences headaches, dizziness, and blurred vision (flickering spots before her eyes). Phenomena of hypertensive angiopathy of the retina are noted. Some pregnant women experience pain in the epigastric region, nausea, and vomiting. At this time, hemorrhages in the brain and other vital organs are possible. Sometimes premature birth, premature placental abruption, and fetal death occur. As the clinical manifestations of gestosis increase, cerebral circulation is disrupted. As a result, convulsive readiness appears, eclampsia occurs - convulsions and loss of consciousness.
Eclampsia occurs most often against the background of preeclampsia or nephropathy. Characterized by convulsions and loss of consciousness. A seizure in eclampsia may have a sudden onset, but in most cases it is preceded by symptoms of preeclampsia. It develops in a certain sequence.
The first stage lasts 20–30 s. At this time, small fibrillary contractions of the facial muscles are observed, which then spread to the upper limbs.
The second stage lasts 15–25 s. It is characterized by the appearance of tonic convulsions of all skeletal muscles, accompanied by impaired or complete cessation of breathing, cyanosis of the face, dilated pupils, and loss of consciousness.
At the onset of the third stage, which lasts 1–1.5 minutes, tonic convulsions turn into clonic convulsions of the muscles of the trunk, then the upper and lower extremities. Breathing becomes irregular, hoarse, and blood-colored foam comes out of the mouth due to biting the tongue.
The fourth stage is characterized by the fact that after the seizures stop, the patient falls into a coma (usually lasting no more than 1 hour, sometimes several hours or even days). Consciousness returns gradually, amnesia is noted, the patient is bothered by a headache and weakness. Sometimes the comatose state persists until a new seizure. A convulsive seizure may be single, or there may be a series of seizures of up to several dozen, repeated at short intervals (eclamptic status). The more seizures there were, the more often they were, the longer the period of the patient’s comatose state, the more severe the eclampsia and the worse the prognosis. Sudden loss of consciousness is possible, not accompanied by convulsions. Complications of eclampsia include the development of heart failure, pulmonary edema, acute respiratory failure, and aspiration pneumonia. Brain damage also occurs in the form of edema, ischemia, thrombosis, and hemorrhage. It is possible to develop retinal detachment, an acute form of disseminated intravascular coagulation, and hepatic-renal failure. In case of eclampsia, premature placental abruption and termination of pregnancy cannot be ruled out. During respiratory arrest, fetal death may occur due to hypoxia.
Therapy for gestosis depends on its severity. Treatment of dropsy in pregnancy is based on diet. Limit fluid intake to 700–800 ml and salt to 3–5 g per day. Diets in the form of fasting apple or cottage cheese days are used no more than once a week. For nephropathy in pregnant women, sedatives (tincture of motherwort, Relanium (2.0 ml intramuscularly), phenobarbital (0.05 at night)), desensitizing agents (diphenhydramine 0.1 2 times a day) are additionally prescribed. Antihypertensive drugs are used taking into account individual sensitivity and under regular A/D monitoring (2.4% aminophylline - 10.0 ml intramuscularly, no-spa - 2.0 ml intramuscularly, clonidine - 0.000075 each, 25% magnesium sulfate – 5.0–10.0 ml intramuscularly). In order to normalize the permeability of the vascular wall, ascorutin is prescribed - 1 tablet 3 times a day, calcium gluconate - 0.5, 5% ascorbic acid - 2.0 ml intravenously.
Reflexology and electrotranquilization have a good effect.
Hypovolemia is corrected using infusion therapy (10–20% albumin - 100.0 ml intravenously, hemodez - 400.0 ml intravenously). To restore water-salt metabolism, diuretics are used in the form of herbs (a decoction of bearberry leaves), veroshpiron - 1 tablet 2-3 times a day, lasix - 40 mg intravenously. To normalize metabolism, methionine, folic acid, and asparkam are used. For preventive and therapeutic purposes, when intrauterine hypoxia and fetal malnutrition occurs, nootropic drugs are prescribed - piracetam - 5.0 ml intravenously, ambrobene, hormones, tocolytics. To improve the rheological and coagulation properties of blood, disaggregants are prescribed: curantil 1 tablet 2-3 times a day, as well as rheopolyglucin - 400.0 ml intravenously, trental - 2.0 ml intravenously, antioxidants (vitamin E - 200 mg 1 time, Essentiale – 1 capsule 3 times a day).
The immunomodulator Derinat is administered in the form of 10.0 ml of a 0.25% solution, 1 drop per nose up to 8 times a day for 3–5 days or 5.0 ml of a 1.5% solution intramuscularly from 3 to 5 –8 injections.
Treatment of preeclampsia and eclampsia requires a special approach.
The basic principles were developed by V.V. Stroganov.
1. Creation of a therapeutic and protective regime, including rest, sleep and rest.
2. Carrying out activities aimed at normalizing the functions of the most important organs.
3. The use of medications to eliminate the main manifestations of eclampsia.
4. Fast and gentle delivery.
All activities are carried out in the intensive care ward by an obstetrician-gynecologist together with an anesthesiologist-resuscitator. All manipulations (injections, blood pressure measurement, catheterization, vaginal examination) are carried out under anesthesia.
Eclamptic status, eclampsia in combination with large blood loss, the development of symptoms of cardiopulmonary failure, and eclamptic coma are regarded as absolute indications for artificial ventilation. In these cases, it is necessary to prescribe glucocorticoids: hydrocortisone hemisuccinate (500–800 mg per day) or prednisolongemisuccinate (90–150 mg per day) with a gradual dose reduction. Artificial ventilation of the lungs is carried out in the hyperventilation mode until, without anticonvulsant therapy, there is no convulsive readiness for 2–3 days, the patient is contactable, blood pressure is stabilized, and there are no complications from the respiratory system. To prevent the occurrence and development of acute renal and renal-liver failure, inflammatory and septic diseases, it is necessary to replace blood loss during childbirth (for caesarean section - in the early postpartum period). In addition, it is advisable to carry out active antibacterial therapy. In case of renal and hepatic failure, extracorporeal detoxification methods are performed (hemodialysis, hemosorption, plasmapheresis), hemoultrafiltration. Delivery on time and the use of complex therapeutic interventions can reduce mortality in eclampsia.
The prognosis depends on the severity of OPG-preeclampsia. The prognosis can be very questionable in case of eclampsia, especially with the development of eclamptic coma against the background of cerebral edema, the appearance of ischemia and hemorrhages in the brain. The mortality rate for eclamptic coma can be 50%.
Prevention consists of early detection of diseases of various organs and systems, especially the cardiovascular, urinary and endocrine systems before pregnancy, timely treatment and careful monitoring of a pregnant woman with the above diseases throughout the entire period of pregnancy. Women at risk for OPG-preeclampsia in an outpatient setting especially deserve attention. An obstetrician-gynecologist should examine these patients at least once every 2 weeks in the first half of pregnancy and once a week in the second half.
One of the important preventive measures is timely detection and treatment of pretoxicosis. It is characterized by such signs as asymmetry of blood pressure in the arms (a difference of 10 mm Hg or more in a sitting position), pulse pressure of 30 mm Hg. Art. or less, a decrease in the oncotic density of urine, a decrease in daily diuresis to 900 ml, slight proteinuria and excessive weight gain.
Diagnosis of gestosis - diagnostic methods
If the doctor suspects gestosis, he prescribes the following procedures:
- general and biochemical blood tests;
- urine tests (24-hour, biochemical and clinical);
- weighing;
- blood pressure measurement;
- fundus examination;
- Ultrasound and Dopplerometry of the fetus.
The patient must be examined by a therapist, neurologist, ophthalmologist and nephrologist. A significant deviation of pressure from the norm is considered a serious problem. Doctors must take into account the initial blood pressure of a woman with blood pressure in the second period of pregnancy.
A special group consists of hypertensive patients, whose blood pressure is initially elevated. They are under constant medical supervision. If a woman only has edema, then she is at risk for a more severe form of gestosis.
From the moment edema appears, specialists begin to take measures to prevent complications. The success of treatment depends on the pregnant woman’s body.
When diagnosing edema, a specialist evaluates weight gain over the entire period of pregnancy, as well as over a month and a week. An increase of about 300-400 grams is considered normal. A pathological increase indicates hidden edema. In this case, measures are taken to correct nutrition and water-salt metabolism.
The gynecologist recommends sticking to a diet and fasting days. If this does not help, the doctor prescribes special medications. If a pregnant woman has a significant weight gain, but there is no edema, then she may be given an MCO test (McLure-Aldrich test).
It involves injecting a woman with a saline solution under her skin. The doctor records the time it takes for the papule to resolve. If the interval does not take 35 minutes, then there is swelling in the body.
The first sign of edema is slight numbness in the fingers . It is difficult for a woman to straighten her fingers; she can hardly put on rings. For minor swelling of the legs, the gynecologist prescribes treatment, which is carried out on an outpatient basis. If your arms, legs and face swell, your blood pressure is high, and there is protein in your urine, then you need to go to the hospital.
In this case, the woman’s condition can deteriorate sharply at any moment. Self-medication is not allowed here. Some women begin to take diuretics on their own, which further worsens the situation.
Preeclampsia in the second half of pregnancy
Late toxicosis occurs for many reasons. Disorders in the endocrine system, obesity, sexually transmitted diseases, hypertension - all these factors can contribute to the development of gestosis in the second half of pregnancy. Sometimes it is a consequence of the flu or acute respiratory viral infection.
Poor nutrition can also give impetus to the development of late toxicosis. It is impossible to cure it at home. The woman requires hospital treatment. She is put on IVs and prescribed medications that help replenish the lack of fluid in the vessels.
The cause of late toxicosis is often pathology in the placenta. In this case, childbirth is considered the most effective solution to the problem. In case of serious complications, a caesarean section is resorted to.
The initial symptoms of late toxicosis are detected during the next examination at the antenatal clinic. The doctor evaluates weight gain, measures blood pressure, examines urine samples and counts the fetal heartbeat. Based on the data obtained, he can conclude about the presence or absence of gestosis.
If the doctor insists on hospitalization, then you cannot refuse. Late gestosis does not go away on its own. The symptoms will only get worse. If you miss time, you may experience preeclampsia or more severe complications (seizures).
Reviews
Alexander, gynecologist
Gestosis is a disease that threatens the life of the pregnant woman and the fetus. If among the pregnant woman’s close relatives there were those who suffered from gestosis, you should definitely inform your doctor about this.
Elizabeth, therapist
How does gestosis manifest during late pregnancy? The most obvious sign is swelling, surges in blood pressure, and especially its increase, as well as a general deterioration in well-being. Such symptoms should be reported to your doctor immediately.
Stefania, 28 years old, store director
During my second pregnancy, I suddenly encountered a disease such as gestosis, although my first pregnancy was easy. I was diagnosed with the disease in the first trimester, and I spent the entire second and third trimester in the hospital. The birth took place by caesarean section, the baby was born healthy, but I had to recover for a long time.
Zhanna, 36 years old, hairdresser
During pregnancy I was diagnosed with gestosis. Since the treatment was not carried out in a timely manner, the disease turned into eclampsia, and I lost the child.
Miroslava, 29 years old, nutritionist
I always thought my pregnancy would be easy. But already in the second trimester I observed signs of gestosis, treatment for which was started almost immediately. She was treated on an outpatient basis and in a hospital, and gave birth herself.
If you detect the first signs of gestosis, you need to inform your doctor about it as soon as possible. The pathology will not go away on its own, which means that your life and that of your child is at risk. Take care of yourself and have an easy pregnancy!
How does childbirth occur with hystosis?
The severity of the disease affects the choice of time and method of delivery. The doctor takes into account the condition of the mother and child.
The most favorable births are those that occur through the natural birth canal. This is a truth that has been supported by all gynecologists and obstetricians from time immemorial.
But for such a birth, the following conditions are needed: a mature cervix, proportionality of the mother’s pelvis and the fetal head, cephalic presentation of the fetus, the woman’s age is not older than 30 years, the absence of illnesses in the mother and other factors.
With gestosis, childbirth can be accompanied by complications. Therefore, it is carried out very carefully, using antispasmodics and painkillers. Delivery with gestosis is considered stressful for the fetus and mother.
Research conducted by specialists has shown that with this disease, the woman and fetus have reduced anti-stress resistance. Any aggressive influence during childbirth (fatigue, hyperstimulation of the uterus, painful manipulations) can have dire consequences. A woman has every chance of suffering from fulminant and critical hypertension.
As a result, cerebral blood flow may be impaired, leading to eclampsia. Statistics show that eclampsia during childbirth occurs quite often. It can occur not only during vaginal delivery, but also during caesarean section.
Typical complications of gestosis during childbirth
- fetal asphyxia;
- premature placental abruption;
- heavy bleeding in the postpartum period.
The main way to relieve a woman of gestosis is childbirth. But for an immature and premature baby, delivery before the due date is not a very favorable outcome. But in some cases, the baby has a better chance of surviving outside the mother's body. Then the only strategy of doctors becomes delivery. It allows you to save the life of the child and mother.
Childbirth with gestosis is carried out against the background of stabilization of laboratory and clinical parameters.
Indications for early birth (regardless of gestational age):
- nonconvulsive or convulsive eclampsia, seizures;
- gestosis, which progresses even with hospital treatment;
- rapid deterioration in the woman’s health;
- retinal disinsertion;
- placental insufficiency, which progresses;
- placental abruption;
- signs of hepatopathy.
Doctors perform a gentle and quick delivery. Preference is given to childbirth through the natural birth canal. This avoids the stress that surgery and anesthesia cause. The woman is given pain relief.
Caesarean section is performed if there are absolute indications: preeclampsia and eclampsia, placental abruption, oliguria, coma.
Gestosis after childbirth
After childbirth, some women experience symptoms of gestosis. Such patients are prescribed appropriate treatment, which is continued until their condition stabilizes. The treatment regimen is determined individually.
What are the degrees and classifications of gestosis?
Experts distinguish between early and late gestosis. The first occurs at 22-24 weeks and lasts quite a long time.
The second may appear when the period is 36 weeks. Late gestosis usually does not have severe complications.
During this period, the baby has already formed and delivery is not accompanied by dangerous symptoms.
Severity of gestosis:
- light,
- average,
- heavy,
- eclampsia.
Doctors also distinguish pregestosis or the preclinical stage of the disease. There is also a division into combined and pure gestosis. Concomitant conditions are important here. Pregnant women with extragenital diseases that were not detected in time are included in the group of women suffering from pure gestosis.
If complications arise against the background of an existing disease, then we are talking about combined gestosis. In practice, 70% of women have the combined form. The most unfavorable symptoms are observed in pregnant women who have liver disease, kidney disease, endocrine disorders, hypertension and metabolic syndrome.
Edema plays an important role in the diagnosis of gestosis. They can have different degrees of severity :
grade I - swelling of the lower extremities;
degree II - swelling of the lower and upper extremities, as well as the abdominal wall;
grade III - swelling spreads to internal organs.
Edema may be hidden. They may be accompanied by proteinuria and arterial hypertension. The course of the disease is determined by conducting blood and urine tests. At the same time, the doctor monitors the condition of the fetus. The severity of gestosis can be judged by the number of baby's heartbeats.
Early gestosis
Early gestosis or toxicosis worries many pregnant women. It occurs in the first half of the term. Doctors cannot name the reasons for early gestosis.
The main manifestations of toxicosis:
- dizziness,
- nausea,
- salivation,
- vomit.
They can be expressed with different strengths. If gestosis manifests itself too clearly, then doctors prescribe treatment. Toxicosis is so widespread that its symptoms are considered normal during pregnancy.
In fact, gestosis has a pathological basis. Normally, pregnancy in a healthy woman should not be accompanied by nausea and vomiting. Pregnancy is a physiological normal state of the body. This is not a pathology.
The mechanisms of development of early gestosis have not been studied. Experts believe that it is a pathological reaction of a woman to pregnancy. Immune, allergic, toxic, reflex and neurogenic mechanisms are involved in the development of toxicosis.
In some cases, gestosis in early pregnancy takes the form of asthma, dermatosis, tetany or osteomalacia.
Late gestosis
This is a complication that occurs in the second half of pregnancy. It develops until childbirth. Such toxicosis leads to disruption of a woman’s systems and organs.
The reasons for the development of late gestosis have not been studied by science. According to some versions, gestosis occurs due to immunological incompatibility of the fetus and mother.
Other experts believe that hormonal processes are to blame. Late gestosis has been detected very often in recent years.
Many obstetricians attribute this to the increased incidence of late births. Women who give birth after 35 years have chronic diseases that complicate the course of pregnancy and childbirth.
A woman may notice the first signs of late gestosis at 28 weeks. Pregnant women usually experience swelling. This is the mildest manifestation of the disease. Edema is also called “edema of pregnancy.” In more severe cases, the complication manifests itself as nephropathy.
Mild gestosis
A mild degree of the disease is characterized by a slight increase in blood pressure. It exceeds the norm by 20%. Protein in urine is 1.0 g/l. Signs include swelling. The woman is undergoing outpatient treatment.
Severe gestosis
Blood pressure exceeds the norm by 40% and more. Protein content - 3.0 g/l. The pregnant woman's health is deteriorating. She develops a headache, swelling increases, and protein in her urine increases.
Sleep may also be disrupted and vision may deteriorate. The patient is admitted to the hospital. If the condition is very serious, the pregnant woman is sent to intensive care. Treatment tactics depend on the condition of the woman and the fetus.
Pathogenesis of gestosis
The basis of the pathogenesis of the disease is a generalized spasm of blood vessels. This is manifested by an increase in pressure. Due to damage to the endothelium, spasm occurs. Dystrophic changes occur in the patient’s organs and tissues. The functions of the liver, kidneys and nervous system are impaired, and the fetus and placenta are also affected.
The mechanism of development of gestosis is a controversial issue. Many experts adhere to the hormonal theory. The cause of complications in this case is considered to be dysfunction of the adrenal glands, changes in the production of estrogen or the hormonal status of the placenta.
There are doctors who support the renal theory of the occurrence of gestosis. The kidneys are compressed by the growing uterus, which entails a number of disorders in the body. But this theory is refuted by facts that claim that toxicosis occurs in pregnant women even without compression of the kidneys.
There is also an immunogenetic theory, which states that some pregnant women have disrupted placentation due to genetic characteristics.
Symptoms
The classification distinguishes between “pure” gestosis and those arising against the background of concomitant diseases. The main clinical signs of late gestosis:
- High blood pressure. It is more convenient to navigate by average pressure indicators. It is determined using a machine or formula by dividing by “3” the sum of systolic and double diastolic pressure. Normally it should not exceed 100 mm. Hg Art. The onset of the disease is indicated by exceeding this figure by 15 mm.
- Presence of edema.
- Increased protein content in urine.
Some women may only have two of the three main symptoms. Depending on their severity and taking into account subjective symptoms and other indicators, the following forms of gestosis in late pregnancy are distinguished:
- Dropsy of pregnancy.
- Nephropathy.
- Preeclampsia.
- Eclampsia.
Dropsy of pregnancy
This is the mildest form of late gestosis. Its main symptom is swelling of varying degrees:
- 1st - only shins;
- 2nd - anterior abdominal wall and legs;
- 3rd - swelling of the face also occurs;
- 4th - anasarca (total swelling).
Edema is accompanied by a decrease in the amount of daily urine (up to 30–60% or more) and a weight increase of more than 350 grams within a week.
Nephropathy
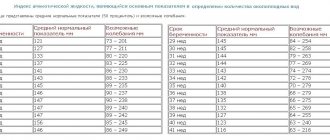
It can develop independently or as a result of ineffective treatment of dropsy, as evidenced by the addition of high blood pressure and/or protein in the urine. Depending on the symptoms, there are 4 degrees of nephropathy, which are conveniently determined using the presented 8-point Wittlinger scale. Based on the calculated sum of points, the severity of nephropathy is determined:
- Easy – 2 – 10 points.
- Average – 11 – 20 points.
- Severe - more than 21 points.
| Number of points | Blood pressure indicators (mm Hg) | Amount of protein in urine g/day | Edema | Daily urine output (diuresis) in liters | Increase in body weight (kg) from the beginning of pregnancy. | Subjective symptoms |
| 0 | 120 and 80 | No | No | More than 1.0 | Up to 12 | No |
| 2 | 140 and 90 | up to 1.0 | limited | — | 13 — 15 | weakness, increased thirst, slight shortness of breath when walking, etc. |
| 4 | 160 and 100 | 2 – 3 | common | 0,9 – 0,6 | From 16 and over | — |
| 6 | — | 4 or more | — | Less than 0.5 | — | — |
| 8 | 180 and 110 | — | — | No urine for more than 6 hours | — | — |
What are the dangers of gestosis during pregnancy?
Gestosis is dangerous due to its complications. If it is accompanied by vomiting, then the pregnant woman may be dehydrated. The functions of many organs and systems are impaired. The kidneys, liver and heart suffer. The most severe complication is yellow acute liver atrophy, which can be fatal. But this pathology develops very rarely. If gestosis is extremely severe, the pregnancy is terminated.
If the course of early toxicosis is favorable, its symptoms disappear by the 12th week. If it continues, then doctors talk about pathology. This may be caused by exacerbation of chronic diseases or some obstetric pathology.
Any form of late gestosis poses a danger to the fetus. Blood circulation in the blood vessels of the placenta is disrupted. The acute form of the disease causes detachment, premature birth or death of the child. Sluggish gestosis causes intrauterine growth retardation in the baby.
Treatment
You can begin therapy for gestosis only after diagnosis and consultation with a specialist; self-medication is prohibited. With timely medical interventions, the chances of a successful pregnancy outcome and natural childbirth increase. If the patient has nephropathy of any severity, preeclampsia or eclampsia, then treatment takes place in an inpatient setting.
Treatment of pathology in pregnant women is aimed at normalizing the water-salt balance, stabilizing metabolic processes, improving the functioning of the cardiovascular system and central nervous system.
Complex therapy includes:
- avoiding stressful situations;
- conducting physiotherapy, which has a calming effect;
- bed, semi-bed rest;
- inclusion of foods rich in vitamins in the diet, as well as taking multivitamins for expectant mothers;
- treatment with medications to normalize the functions of the organs and systems of the expectant mother and the child suffering from hypoxia in the womb.
Drugs used in treatment:
- calming and sedative effects (motherwort or valerian); in severe cases, tranquilizers and antipsychotics may be prescribed;
- disaggregants (Curantil), anticoagulants (Fraxiparin) - only under strict control of blood clotting;
- antioxidants (ascorbic acid);
- antihypertensive drugs.
If the treatment did not produce any results and the disease began to progress, specialists may prescribe early delivery. In this case, the birth of a premature baby is less dangerous than its presence in the belly of a pregnant woman.
Treatment of mild gestosis, which is characterized only by swelling and other mild symptoms, is carried out at home. In all other cases, the expectant mother must be under the supervision of doctors around the clock due to the fact that the disease can begin to progress at any time.
What are the principles for treating gestosis?
Modern doctors cannot completely eliminate gestosis. In many cases they control this complication. Timely treatment helps prevent the development of severe complications. Self-medication is an unacceptable measure. Without the help of a professional, gestosis enters a severe stage.
Basic principles of treatment:
- maintaining a medical and protective regime;
- taking sedative medications (valerian, motherwort or stronger drugs);
- drug treatment of internal organs;
- careful and timely delivery.
If gestosis is treatable and does not progress, then induction of labor is not used. Premature birth is a forced measure that is used in severe cases.
If treatment does not lead to positive changes, and the condition of the mother and child worsens, then the question of childbirth arises.
The treatment regimen for toxicosis is developed individually. Doctors take into account many nuances: the severity of the disease, concomitant diseases, the condition of the fetus, etc. Mild toxicosis begins to be treated in the antenatal clinic.
If after a week the woman’s condition has not improved, she is sent to the hospital. Medicines for gestosis are mandatory. It is impossible to cure this disease with herbs and diets.
Pregnant women with edema that accompany moderate and mild degrees of gestosis are treated in a hospital (department of pathology of pregnant women). In severe cases of gestosis with signs of preeclampsia, the woman is admitted to the intensive care unit.
The duration of treatment depends on the severity of gestosis. The best treatment for severe forms is delivery. Therefore, three hours after ineffective treatment for preeclampsia, the patient undergoes a cesarean section.
Prevention of gestosis
- proper nutrition;
- active lifestyle (pregnant women benefit from yoga, swimming, fitness);
- frequent walks in the fresh air;
- absence of bad habits and stress;
- taking preventive medications as prescribed by a doctor (Magne-B6, vitamin E, chimes, etc.);
Diet for gestosis
Proper nutrition can improve the condition of a pregnant woman. A woman should have healthy foods on her table. The emphasis should be on foods rich in protein. This includes lean meat, cottage cheese, fish and eggs. Sweet, fatty, fried, smoked and salty foods should be excluded.
Fast food is strictly prohibited. The daily menu should include fresh vegetables, fruits, juices and herbs. You should eat more fiber foods to relieve constipation.
If there is swelling, the doctor will create a diet. He recommends monitoring the amount of fluid you drink and excrete. Pregnant women must control the amount of food they eat. Otherwise, there will be a strong weight gain, which can lead to a number of complications.
Pregnant food should be rich in vitamins and microelements. You should drink purified water, excluding coffee, strong tea and carbonated drinks. Doctors usually prescribe special vitamin complexes for pregnant women. They must be accepted without fail.
Find out the important causes of oophoritis, how it affects pregnancy and how to be cured without consequences.
What symptoms and signs of endocervicitis you need to know in order to respond in time, read here
Modern types of diagnostics of ovarian dysfunction are described in this article https://womensmed.ru/bolezni/disfunkciya-yaichnikov/disfunkciya-yaichnikov-lechenie-i-simptomatika.html
Prevention
In the antenatal clinic: identifying pregnant women at high risk of developing gestosis.
Pregnant women are recommended to get enough sleep, limit stress situations, eat a diet low in sodium, and eat foods high in protein (lean meat and fish, low-fat cottage cheese and milk).
There is no specific preventive drug therapy for gestosis.
Early diagnosis of mild forms of gestosis in a antenatal clinic, pathogenetically based therapy and timely hospitalization are the prevention of worsening gestosis.
To date, gestosis remains the most mysterious complication of pregnancy with an unknown etiology, incompletely studied pathogenesis, and the absence of radical methods of treatment and prevention. At the same time, early detection of signs of gestosis and adequate therapy can prevent the worsening of gestosis and prolong pregnancy for some time.
What are the possible consequences of gestosis?
Preeclampsia is a dangerous condition that can lead to dire consequences. It ranks second among the causes of death of mothers (the first place is given to bleeding). A complication of gestosis is perinatal mortality (its rate reaches 32%).
Women suffering from gestosis suffer from endocrine disorders, hypertension, and kidney pathologies. Children born to such mothers experience problems with psycho-emotional and physical development. Many children often get sick in early childhood.
Possible complications
Diseases at a late stage can lead to a number of complications. The most dangerous thing is the death of mother and child. Dangerous complications include the following:
- coma;
- intracerebral hemorrhage;
- renal failure;
- breathing problems;
- loss of vision;
- placental abruption;
- DSV syndrome;
- hemorrhagic shock.
Rare complications include acute fatty hepatosis and HELLP syndrome.
All complications arise very quickly. Therefore, the woman should be operated on immediately. However, this also does not provide a 100% guarantee, since bleeding may develop during the postoperative period.
How to avoid gestosis
In order for this pathology to bypass you, its prevention must begin even before conception. All chronic diseases should be identified and treated. Hidden infections can be detected if you undergo testing. It is very important to lead a healthy lifestyle.
Eliminate bad habits, eat right and follow a daily routine. All this will contribute to the normal course of pregnancy.
In conclusion, I would like to add that I agree with all this, subject to the competence and adequacy of the attending physician.