Amniotic fluid plays a huge role in the development of the unborn child and the course of labor. Not only the condition of the unborn baby, but also the mother, depends on their quantity and quality.
Polyhydramnios, as an obstetric pathology, is common, but few pregnant women attach particular importance to this complication, although it, like all other deviations from the physiological course of pregnancy, requires, if not treatment, then careful observation.
The consequences of polyhydramnios are very serious and can become tragic, including the loss of an unborn child.
Amniotic fluid - why and in what volumes is it needed?
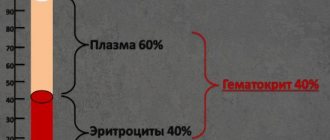
In the mother's tummy, the baby is surrounded by amniotic fluid, which protects him from injury, shock, and infection. In addition, it ensures the movement of the baby inside the placenta and affects the dilation of the cervix during childbirth. In the first half of pregnancy it is colorless and transparent, in the third period it is a little cloudy. The composition of amniotic fluid changes throughout pregnancy. In the first trimester, it is similar in composition to blood plasma, in the last trimester it contains urine secreted by the fetus, its vellus hair, epidermis, and vernix. In addition, amniotic fluid consists of oxygen and carbon dioxide, fats, carbons, enzymes, electrolytes, proteins, hormones, vitamins, phospholipids and blood clotting factors. The amount of liquid is also different. So, in the ninth week of pregnancy it is about 30 ml, in the fourteenth - 100 ml. The amniotic fluid reaches its maximum volume (1000-1500 ml) at 36–38 weeks. Amniotic fluid is completely renewed every three hours due to the “mother-placenta-baby” system. There is a constant exchange of substances between the mother, the placenta and the child - the female body produces plasma, one of the membranes of the placenta, the amnion - fluid, the child secretes urine. Thanks to this exchange, water renewal occurs and its optimal composition is maintained. An ultrasound examination determines the amniotic fluid index. The unit of measurement is centimeters (cm) or millimeters (mm). From 20 to 35 weeks, the normal AFI is 8–18 cm. An index of more than 25 cm indicates the presence of pathology.
Polyhydramnios - AFI above the upper limit
Causes
To endure this condition with minimal consequences or to avoid them completely, you need to understand what it is. All links of the unified system “woman - placenta - fetus” participate in the formation of amniotic fluid.
As the baby grows, it swallows fetal fluid, receiving nutrients from it. After processing, it is excreted into the amniotic sac in the form of urine. In this case, every three hours the fetal fluid is completely renewed.
Due to various negative reasons, the optimal balance may be disrupted. When the production of fetal fluid prevails over excretion from a woman’s body, its amount increases disproportionately.
To control, doctors use the amniotic fluid indicator, which is calculated during an ultrasound. If its index exceeds the table limits, then polyhydramnios is diagnosed.
Dangerous consequences of polyhydramnios
If the volume of amniotic fluid is higher than average, they speak of polyhydramnios. The consequences of this pathology can be different, it all depends on the form, degree, and time of diagnosis. For the expectant mother, excess fluid threatens abnormal position of the fetus, early birth, premature aging of the placenta, and late gestosis. For the child, there is a threat of fetoplacental insufficiency, infection, umbilical cord entanglement, abnormalities in the development of the gastrointestinal tract, nervous system, and hypoxia. The most dangerous option is spontaneous abortion with a fatal outcome.
Why is it dangerous?
The main danger of polyhydramnios in pregnant women is the threat of miscarriage. This is how the pathology ends in 35% of women. In most cases, pregnant women have severe toxicosis at any stage, which often turns into vomiting, which threatens dehydration. A large amount of water interferes with the correct presentation of the fetus, so the child’s incorrect position is often observed: pelvic or transverse. The risk of fetoplacental insufficiency, when the functioning of the placenta is disrupted, cannot be excluded. The fetus develops oxygen starvation, which harms its full development.
Why does polyhydramnios occur?
Unfortunately, even with the modern level of medicine, the causes of polyhydramnios cannot always be recognized. If a mother suffers from diabetes, kidney disease, vascular disease, or heart disease, she is at risk. The cause of the disease can be TORCH infections, so during pregnancy, tests are prescribed for the presence of antibodies to these diseases and, if necessary, a course of treatment. Polyhydramnios can also develop in case of incompatibility of the Rh factors of the mother and father, or fetal pathologies. In recent months, the amount of water may exceed the norm due to the fact that the child swallows more water, and this provokes an increase in its quantity. The likelihood of developing polyhydramnios increases when carrying twins or triplets.
Various rhesus
The causes and consequences of polyhydramnios are interrelated. If the expectant mother has a negative Rh factor, and the father of the child has a positive one, then a conflict may arise. This usually does not happen during the first pregnancy. After childbirth, antibodies can form in the woman’s blood, which in subsequent pregnancies will try to destroy the foreign body. In this case, polyhydramnios often develops.
Fixing an existing problem can be quite difficult. However, prevention allows a woman not to encounter the development of Rh conflict. For this purpose, immunoglobulin is administered. Please note that the procedure takes place over a certain period of time under the supervision of specialists. These products are available only by prescription.
Forms, degrees, types of polyhydramnios
The form of polyhydramnios is determined by the amniotic fluid index. Depending on how much higher it is than normal, three forms are distinguished.
This is what polyhydramnios looks like
Moderate polyhydramnios
This form is diagnosed based on the results of an ultrasound examination, without visible external signs and complaints about changes in condition. Water accumulates gradually, the discrepancy with the norm is insignificant. With moderate polyhydramnios, the chances of successful pregnancy and childbirth are quite high.
Acute polyhydramnios
It manifests itself as a sharp increase in the volume of amniotic fluid. It can develop within a day or several hours, while the pregnant woman’s condition sharply worsens - the stomach grows quickly, severe shortness of breath, pain in the lower abdomen and perineum occurs. Most often it occurs from 16 to 20 weeks of pregnancy and is diagnosed at an early stage. This type of disease is very dangerous because it threatens uterine rupture.
Chronic polyhydramnios
With this type of pathology, the fluid enters gradually, so it appears in a more erased form, often without visible symptoms and does not feel pregnant. The chronic stage appears at 30–33 weeks. Chronic polyhydramnios can be accurately determined by ultrasound. Characteristic symptoms of the pathology are an overly large belly, a sudden appearance of stretch marks, a dull heartbeat, excessive activity of the fetus, and incorrect positioning of the child in the uterus. A woman may feel heartburn, tachycardia, shortness of breath, and weakness. Swelling appears that does not go away after rest.
Chronic polyhydramnios has three stages:
- light, in which the amount of liquid does not exceed 3 liters;
- medium, when the volume of liquid is within 3–5 liters;
- heavy - the volume of water is more than 5 liters.
There are five types of polyhydramnios:
- relative - the indicators are slightly higher than normal, but the amount of water corresponds to the size of the fetus. It is not dangerous if the pregnant woman does not suffer from any infection. Most often occurs in women carrying a large child;
- moderate, the volume of fluid is close to the upper limits of normal or the deviation from it is insignificant with an increase in symptoms. It may not appear externally;
- borderline - the amount of water on the verge of normal and increased;
- pronounced, the characteristic symptom of which is a very rapid increase in abdominal volume and all signs of pathology are clearly defined;
- idiopathic, occurring for unexplained reasons.
What kind of pathology
As mentioned above, this disease appears due to increased accumulation of fluid in the uterus. The fetus periodically absorbs a certain portion, which then exits the body with urine. This is how the required volume is adjusted. However, often the balance is upset and the amount goes beyond the norm.
Symptoms and signs
It is very difficult to independently determine polyhydramnios, since its symptoms are often perceived by pregnant women as normal. There is an explanation for this, because the signs of this pathology are loss of strength, shortness of breath, the appearance of stretch marks and swelling of the limbs, pain in the lower abdomen, and increased fetal activity. The symptoms of chronic polyhydramnios are not clearly expressed, they increase gradually, the woman gets used to the changes and may not pay attention to them. There are other signs, such as changes in the fundus of the uterus or difficulty listening to the baby's heartbeat, but only a doctor can determine them.
How to diagnose polyhydramnios
The volume of the abdomen should not exceed the norm.
Polyhydramnios can be suspected during a routine examination in the presence of characteristic complaints and accompanying signs, such as pale skin, a significant increase in abdominal circumference, the presence of a venous network, too easy movement of the fetus in the uterus, difficulties in listening to the heartbeat. To confirm the diagnosis and determine the causes of occurrence, a number of studies and tests are prescribed:
- An ultrasound examination will help determine the amniotic fluid index - the main indicator of pathology, as well as clarify the gestational age, the size of the child and the amount of amniotic fluid;
- Doppler and CTG to assess the condition of the fetus;
- blood glucose test to rule out diabetes;
- smear on vaginal microflora;
- clinical blood and urine analysis;
- blood test for TORCH infections.
Childbirth
As already mentioned, labor occurs earlier than expected with polyhydramnios. In the last stage of pregnancy, a dense bladder may rupture suddenly, after which amniotic fluid flows out profusely and sharply. At this moment, a fetal limb or umbilical cord may fall out, and the woman’s labor will be weakened. Sometimes a pregnant woman does not feel contractions at all. With polyhydramnios, childbirth is associated with other complications:
- poor position of the baby inside the womb (for example, buttocks down);
- heavy bleeding after childbirth;
- placental abruption.
How is polyhydramnios treated?
The possibility of treating polyhydramnios depends on the form, stage and time of its detection. Early diagnosis and determination of the causes of the pathology significantly increases the chances of recovery without serious consequences. If the disease is moderate or severe, hospitalization is recommended. If polyhydramnios is caused by diabetes, medications that reduce glucose levels are used. If there is a Rh conflict, therapy is recommended to prevent hemolytic disease in the child. In the case of an unknown cause of polyhydramnios, treatment includes taking tocolytics, antiplatelet agents, antispasmodics, vitamins, drugs to improve uteroplacental blood flow and blood microcirculation, diuretics, and antibiotics.
Treatment
Subsequent treatment tactics depend on the identified cause. In exceptional cases, the reason for the deviation remains unclear. In this case, special treatment is prescribed to improve the baby’s condition and reduce the amount of water.
- Various kinds of vitamins.
- Using a broad-spectrum drug - Erythromycin, Rovamycin, Josamycin.
- Medicines to improve blood flow of the placenta and umbilical cord - Curantil, Actovegin.
In other cases, the woman is admitted to a hospital. In mild cases, if there is no increased circulatory or respiratory impairment, doctors will continue the pregnancy and continue to monitor the condition.
In the worst case, in the acute form, doctors may prescribe an artificial abortion, as this can pose a serious threat to the life of the woman in labor.
Treatment is based on antibiotics. In advanced stages, broad-spectrum antimicrobials are used. The main goal of treatment is to establish microcirculation, uteroplacental blood flow, and the metabolic process. During treatment, diuretics and vitamin medications are prescribed.
How does childbirth occur with polyhydramnios?
Pregnancy with mild or moderate polyhydramnios continues until the due date and most often ends in a successful natural birth. If the baby develops problems with heartbeat or blood flow problems, labor is induced early. Premature labor can begin due to a sudden rupture of the amniotic sac. With subsequent excessive discharge of water, prolapse of the fetal limb and parts of the umbilical cord may occur. In this case, an emergency caesarean section is performed. Abnormal fetal position, often observed with polyhydramnios, is also considered an indication for surgery. To avoid a decline in labor activity subsequently due to early and abundant discharge of water, the amniotic sac is punctured. After the puncture, the water does not recede so quickly, the uterus contracts gradually, and contractions increase. If it is necessary to stimulate labor, it can begin 2 hours after the water breaks; early stimulation can provoke the passage of the placenta. In the second stage of labor, agents are used to promote uterine contraction. Newborns following pregnancy with severe, acute polyhydramnios may require close monitoring by a neonatologist.
The author of this article was diagnosed with polyhydramnios in one stage or another form (but not severe or acute) in all three pregnancies. In the latter case, the cause of the pathology was identified as twins with one placenta and a common amniotic sac separated by a thin septum (monochorionic diamniotic twins). During my second pregnancy, I had to suffer a severe respiratory viral infection, with an exacerbation of the herpes virus. The causes of polyhydramnios during the first pregnancy could not be discovered. All three pregnancies ended in physiological birth on time. True, I couldn’t do without taking medications prescribed by the doctor; during my second pregnancy I even had to stay in the hospital. The treatment was classic - antibiotics, vitamins, drugs that improve blood flow. The main thing is that all births passed without complications, and the children were born healthy. Unfortunately, not all pregnancies complicated by polyhydramnios end as successfully, so you should listen to the doctor’s recommendations and your own feelings.
Folk remedies
Photo: ivona.bigmir.net
Of course, there are no traditional medicines that can eliminate polyhydramnios during pregnancy. When the first signs of a pathological process appear, you should immediately contact a medical institution, where a qualified specialist will prescribe appropriate treatment. Polyhydramnios during pregnancy is a serious gynecological pathology, which without appropriate treatment can lead to various complications. That is why it is extremely important to carefully follow all the doctor’s recommendations and under no circumstances self-medicate at home.
In addition, do not forget about the importance of preventive measures, the observance of which will significantly reduce the risk of developing pathology. These include:
- pregnancy planning;
- timely diagnosis and treatment of infectious and inflammatory diseases of the reproductive organs, including sexually transmitted infections;
- the use of barrier methods of contraception (condoms) during sexual intercourse, as well as the exclusion of casual sexual intercourse;
- timely registration with the antenatal clinic (no later than 12 weeks of pregnancy);
- regular visits to an obstetrician-gynecologist.
Also, do not forget about proper nutrition. It is recommended to consume more dairy products, vegetables and fruits rich in fiber and vitamins. You should not overuse fried and spicy foods, as well as canned foods. It is important to give up bad habits (smoking, drinking alcohol and drugs), which are known to increase the risk of developing pathology. Particular attention is paid to the sleep and rest regime, the observance of which helps to strengthen the general condition of the pregnant woman.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Prevention of polyhydramnios
Unfortunately, it is almost impossible to accurately exclude the possibility of developing this pathology, since the causes of its occurrence are often not obvious. Symptoms such as shortness of breath, fatigue, tachycardia are very common in pregnant women. Abdominal volume that exceeds the norm may be a consequence of excessive weight gain, and not everyone knows how to independently measure the height of the uterine fundus or feel the position of the child. However, the expectant mother can take measures to reduce this risk:
- before pregnancy, conduct the necessary research to identify existing diseases, cure them or achieve remission;
- to maintain a stable condition, use special medications and diet;
- do not miss doctor’s consultations, monitor changes in your health, undergo the necessary studies;
- lead a healthy lifestyle, eat rationally and nutritiously, and rest.
In most cases, childbirth with polyhydramnios is quite successful, sometimes a little more difficult than in the absence of this pathology. The main thing is to get in the right mood and follow the doctor’s instructions.
Reviews
Arina, 25 years old
In the third trimester of pregnancy, I was diagnosed with polyhydramnios. I spent some time in the hospital, because in addition to the excess amniotic fluid, there was a slight leakage. The child was born at 37 weeks, there was no umbilical cord entanglement.
Tatyana, 30 years old
In the 1st trimester I developed polyhydramnios. After lengthy examinations and tests, in addition to polyhydramnios, problems in the development of the fetus were diagnosed. The pregnancy had to be terminated and then treated for a long time.
Anna, 24 years old
In the 2nd trimester, or more precisely, at 20 weeks, I felt unpleasant abdominal pain and increased activity of the baby. Despite the fact that the baby himself was small at this stage, his movements in the tummy caused me discomfort. I went to the gynecologist, they sent me for an ultrasound, where polyhydramnios was detected. I was very afraid that I would have to terminate the pregnancy, but thanks to competent treatment, it was possible to save it. The birth itself took place at 36 weeks. We had to stay a little longer in the maternity hospital, since the baby’s weight was low.
Polyhydramnios during pregnancy is a pathological condition that requires mandatory treatment. It is important to understand that the sooner you start therapy, the greater the chances of having a healthy baby. Take care of yourself and have an easy birth!