Chronic colitis is a set of long-term, wave-like diseases of different parts of the colon, accompanied by morphologically confirmed inflammatory and dystrophic changes in its mucous membrane, and disruption of the functioning of the organ.
It is generally accepted that the phenomena of chronic colitis are present to one degree or another in at least half of patients with gastrointestinal diseases. This pathology is common on all continents and occurs equally often in both men and women. Male patients seek medical help for chronic colitis more often after the age of 40; in women, the disease is more common in the age group from 20 to 60 years.
The greatest prevalence of the disease is observed in Europe and North America, however, the collective term “chronic colitis” is not used in Western medicine.
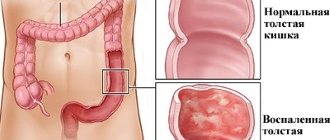
Variants of localization of the inflammatory process in chronic colitis
Causes and risk factors
The causes of chronic colitis are very diverse; the disease can be provoked by both pathogenic microorganisms and adverse effects of external physical factors, as well as internal causes.
Causal factors for the development of chronic colitis:
- infectious process (infection with bacterial agents (usually Shigella, Salmonella, Yersinia, less often Clostridia, Campylobacter), viruses (enterovirus and rotavirus), protozoa (Giardia, amoeba, balantidia, etc.), pathogenic fungi, helminths);
- activation of one’s own opportunistic microflora;
- systematic gross violations of the diet;
- chronic diseases that contribute to the development of endogenous intoxication (chronic renal failure, liver failure, decompensated diabetes mellitus, thyrotoxicosis, etc.);
- chronic exogenous intoxication with salts of heavy metals, pesticides, alkalis, alcohol and other aggressive substances;
- long-term food allergies;
- chronic coprostasis;
- exposure to ionizing radiation;
- congenital pathology of enzyme systems;
- long-term use of medications that irritate the wall of the large intestine (salicylates and other non-steroidal anti-inflammatory drugs, laxatives, etc.).
Risk factors for chronic colitis:
- presence of severe chronic diseases;
- industrial contact with toxic substances;
- immunodeficiency states;
- long-term dysbiosis;
- autonomic dysfunction (impaired innervation of the intestinal wall);
- treatment with antibacterial drugs;
- chronic alcohol disease;
- acute infectious and inflammatory diseases of the gastrointestinal tract;
- the presence of space-occupying formations, adhesions and other mechanical factors that impede the passage of the contents of the large intestine;
- food stereotype with a small amount of fiber, liquid in the diet, consumption of large quantities of processed meat products, soft bread, seasonings, sauces, fatty, fried, spicy foods;
- atherosclerotic disease (ischemia of the mucous membrane of the large intestine);
- abuse of laxatives and enemas.
Antibacterial therapy and abuse of laxatives can lead to exacerbation of chronic colitis
A significant role in the development of chronic colitis is played by autoimmune aggression, when, against the background of active inflammation, the production of antibodies to the structural elements of the mucous membrane of the large intestine is activated, exacerbating the pathological process.
In most cases, with chronic colitis in a patient, it is possible to establish a combination of several causative factors that mutually reinforce each other. However, in some patients it is not possible to reliably establish the root cause of the disease, in which case they speak of cryptogenic colitis.
Classification
Colitis is conventionally divided into two main groups:
- infectious;
- non-infectious.
The first are acute and are the result of infectious pathogens (viruses, bacteria, fungi) entering the body. A chronic course is characteristic of non-infectious colitis. The following types are distinguished:
- nonspecific ulcerative;
- Crohn's disease;
- microscopic;
- ischemic;
- collagen;
- eosinophilic;
- lymphocytic;
- ray;
- Behcet's syndrome;
- caused by taking medications.
Separately, pseudomembranous colitis is distinguished. It belongs to a mixed form of pathology, as it is caused by the bacterium Clostridium difficile and at the same time has a chronic course.
Forms of chronic colitis
Depending on the etiological factor, chronic colitis is divided as follows:
- infectious (viral, bacterial, mycotic);
- parasitic;
- nutritional (food origin);
- intoxication (a consequence of exposure to both internal and external toxins);
- ischemic (impaired blood supply to the wall of the large intestine);
- radiation;
- medicinal;
- mechanical;
- allergic;
- mixed etiology;
- cryptogenic (with unknown cause).
Depending on the location of the inflammatory process:
- total, or pancolitis;
- segmental (with localization of inflammation in a specific part of the large intestine: typhlitis (cecum and appendix), transversitis (transverse colon), sigmoiditis (sigmoid colon), proctitis (rectum).
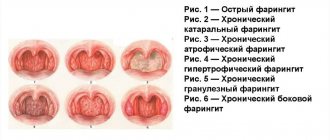
In accordance with the morphological picture of damage to the mucous membrane:
- catarrhal;
- erosive;
- ulcerative;
- atrophic;
- mixed.
Depending on the severity of the inflammatory process, chronic colitis can occur in mild, moderate and severe forms with a constant, recurrent or intermittent course of the disease.
In some patients, it is not possible to reliably establish the root cause of the disease; in this case, they speak of cryptogenic colitis.
Based on the presence of motor dysfunction or manifestations of dyspepsia, 2 forms of chronic colitis are distinguished:
- with motor dysfunction (hyper- and hypokinetic forms);
- with dyspepsia (fermentative or putrefactive).
When to see a doctor
Chronic colitis (treatment, drugs will help reduce inflammation and prevent serious complications) is not dangerous for humans, however, the degenerative process that affects the deep intestinal mucosa will cause great discomfort.
A person’s life will change, since complex treatment of pathology involves nutritional correction. Patients must strictly adhere to all the specialist’s prescriptions.
You should visit a gastroenterologist as soon as the first disturbances in the functioning of the digestive system appear. A correctly diagnosed diagnosis and selected therapy by a doctor will help you quickly get rid of inflammation and return to your previous life.
Symptoms of chronic colitis
The main clinical manifestations of chronic colitis are local manifestations of the disease:
- diarrhea (from 4-5 to 15 times a day in severe forms of the disease), in some cases possibly alternating diarrhea with constipation;
- the urge to defecate (possibly false) occurs against the background of a sharp change in body position (bending, jumping), after eating (the so-called snacking symptom, more pronounced during transversity), under the influence of stressors, in the early morning hours (“alarm clock chair” with proctosigmoiditis);
- pain, discomfort before or after defecation;
- periodically occurring dull, aching or sharp cramping pain in the abdomen (over the entire surface or in the lower part), intensifying after eating a meal high in fiber, dairy products, fatty, fried foods, carbonated drinks, etc., decreasing or completely stopping after passing gas or bowel movements;
- decreased appetite;
- episodes of vomiting, single or repeated;
- weight loss;
- bloating, rumbling;
- feeling of incomplete bowel movement after bowel movement;
- belching of air, sometimes with the smell of rotten eggs;
- bitterness in the mouth;
- nausea;
- abundant mucus in the stool;
- intestinal crises, characterized by a series of urgent urges to defecate with the release of first normal feces, and then more liquid feces, often mixed with clear mucus, accompanied by cramping pain, relieved after bowel movement.
Manifestations of chronic colitis
In addition to local manifestations, there are general symptoms of chronic colitis:
- deterioration in general health;
- decreased performance;
- irritability, emotional instability;
- decreased tolerance to habitual physical activity;
- fast fatiguability;
- disturbance of sleep and wakefulness (drowsiness during the day, insomnia at night).
Exacerbation of chronic colitis is accompanied by increased symptoms, which during the period of remission may be practically absent or mild in nature. Exacerbations are more often provoked by errors in diet, psycho-emotional or physical stress, and exacerbation of concomitant chronic pathology.
The characteristics of painful sensations depend on the localization of the inflammatory process: with typhlitis, pain is determined in the right iliac region, with sigmoiditis - in the left, with proctitis - in the projection of the rectum.
Complications
Complications can only be caused by ulcerative colitis. The consequences may be:
- perforation of the ulcer, which often causes peritonitis. Symptoms of chronic colitis in this case will be expressed in severe bloating and tension in the abdominal muscles, chills accompanied by high fever, coating on the tongue and weakness of the body;
- gangrene of the affected areas of the intestines and colon. In this case, the person suffers from low blood pressure, weakness and high fever;
- blood poisoning or spread of infection to other organs;
- bleeding in the intestines - this indicates chronic ulcerative colitis;
- the appearance of an oncological tumor.
Diagnostics
Diagnosis of chronic colitis is based primarily on the characteristic clinical picture.
Male patients seek medical help for chronic colitis more often after the age of 40; in women, the disease is more common in the age group from 20 to 60 years.
Data from an objective examination, laboratory and instrumental research methods, indicating the presence of chronic colitis:
- pain on palpation, the characteristic shape of a spasmodic inflamed intestine in the form of a dense cord, and a drumming sound when percussed over the site of the lesion are objectively determined;
- an increase in the number of leukocytes and acceleration of ESR in a general blood test during an exacerbation of chronic colitis;
- during scatological examination, undigested fiber, starch grains, iodophilic microflora (during fermentation processes) or the remains of undigested striated muscle fibers (during putrefactive processes), mucus are found in feces;
- signs of inflammation, dystrophy and atrophy of the colon are detected endoscopically (sigmoidoscopy, colonofibroscopy);
- When conducting an X-ray examination with a contrast agent, smoothing of the structure of the mucous membrane and the disappearance of haustra (the “water pipe” symptom) are noted.
Chronic colitis: results of irrigoscopy
Preventive measures
In order to prevent the development of chronic colitis, the following recommendations must be followed:
- Eat properly.
- Treat infectious diseases in a timely manner (before they become chronic).
- Stop smoking and drinking alcohol.
- Do not abuse medications.
- Use protective equipment when in contact with toxic substances.
If symptoms of the disease are detected, you should consult a gastroenterologist.
Video from YouTube on the topic of the article:
Treatment of chronic colitis
Drug therapy for chronic colitis:
- intestinal antiseptics;
- for indomitable diarrhea - enveloping, astringent drugs, sorbents;
- for constipation - laxatives (stimulating secretion in the intestines, increasing the volume of feces, softening and lubricating agents), the drug of choice is lactulose;
- defoamers for flatulence;
- enzyme preparations;
- prokinetics if necessary;
- selective antispasmodics.
In addition to medication, adherence to a special diet for chronic colitis plays a significant role in treatment:
- limiting carbohydrates and dairy products;
- frequent, split meals;
- for persistent diarrhea - avoid legumes and fiber-rich foods;
- for constipation - drink large amounts of water (at least 2 liters per day), foods high in fiber that stimulate peristalsis;
- refusal of fried, hot, spicy, fatty foods.
For exacerbation of chronic colitis, diet 4a is indicated
During the period of exacerbation of chronic colitis, diet No. 4a is recommended (stale white bread, low-fat weak broths, steamed meat and fish dishes, pureed porridge in water, soft-boiled eggs, steamed omelettes, jelly, decoctions and jelly from blueberries, bird cherry, pear, quince, rose hips, tea, coffee and cocoa on water).
First aid for exacerbation
The stage of exacerbation of colitis begins unexpectedly, so most patients are not ready for this. The onset of the disease is acute. It begins with sharp cramping pain and diarrhea, less often - constipation. If these signs of pathology appear, which can last from several days to a week, you should urgently call a doctor.
An exacerbation of the disease occurs suddenly, so the patient is completely unprepared for it. It manifests itself as a sharp pain localized in the abdominal area and often accompanied by frequent and loose stools. As soon as these signs of an incipient attack of illness appear, which can last from several hours to a week, you should immediately call a doctor. In order to alleviate the patient’s condition before his arrival, the following measures must be taken:
- An electric heating pad or a bottle of hot water applied to the stomach can reduce the painful spasms that always accompany exacerbation of colitis;
- If during an attack of colitis there is such a symptom as severe diarrhea and vomiting, it is necessary to take activated charcoal, and if constipation accompanies the attack, take a decoction of hay;
- In the case when the attack is very severe or is accompanied by an increase in temperature, the patient should be immediately put to bed;
- When an exacerbation of colitis begins, you can also do an enema that contains corticosteroids. This will help prevent the development of severe inflammation;
- Eating any food is strictly prohibited, since the damaged intestine cannot perform its functions.
These methods can temporarily stop the acute manifestations that usually accompany an exacerbation of colitis, but if further treatment is ignored, they will arise again after a while, but in a more severe form. Therefore, to prevent this situation from happening again, the patient needs immediate hospitalization and appropriate treatment.
Patients with developing intestinal colitis are also quite often interested in the question of what to do to prevent exacerbation of the disease from occurring for as long as possible? Here we can only advise that during remission of the disease, strictly follow all the recommendations of the attending physician regarding preventive drug treatment and a diet appropriate to the disease.
And when asked what to do when an exacerbation of colitis is accompanied by diarrhea with blood, a recommendation should be made to immediately undergo a full diagnosis, since such a symptom may also indicate the development of more serious pathologies in the intestines in an acute form. It should also be remembered that in case of exacerbation of colitis, the first step is to consult a specialist, and not to self-medicate, which is always fraught with the development of not only severe, but also terrible complications.
Recommendations
- Consultation with a gastroenterologist.
- Fibercolonoscopy.
| • | Leading specialists and institutions for the treatment of this disease in Russia: |
| doctors of the State Scientific Center for Coloproctology (director - Doctor of Medical Sciences, Professor Shelygin Yu.A.), doctors of the Russian Scientific Center for Surgery named after Academician B.V. Petrovsky. | |
| • | Leading specialists and institutions for the treatment of this disease in the world: |
| St Mark's Hospital, UK. |