After successful fertilization and fixation of the embryo in the uterine cavity, a temporary organ begins to form - the placenta. For the entire nine months of pregnancy, it will become a connecting element between the mother and her baby, transmitting to the fetus through the blood vessels all the nutrients and oxygen necessary for development. Normally, placental tissue should attach and form in the lower part of the uterus or on its walls. In most cases, the membrane is attached to the back wall of the organ and partially covers both side walls, since in this area the muscles provide a more intense blood supply. On the front part of the uterus, the placenta forms much less frequently, since this part of the organ changes greatly during pregnancy. It is worth noting that the location of the membrane in the back of the womb protects it from possible damage.
Placenta previa is the most dangerous pathology during pregnancy, and according to statistics it is observed in 0.6% of all expectant mothers. Attachment of an organ in the wrong part of the womb is dangerous primarily because it causes heavy and prolonged bleeding that is difficult to stop. As a rule, women with this pathology are at risk and are under constant medical supervision throughout the entire period. When diagnosed with placenta previa, the ligamentous membrane is formed and attached in the uterus incorrectly - in the lower part of the organ. By its position, it completely covers the internal os, or is partially located below the level of the presenting part of the fetus. Sometimes the tissues of the organ are located entirely below the developing fetus, so during childbirth they will prevent it from passing through the birth canal.
Causes of improper position of the placenta in the uterus during pregnancy - who is at risk?
The formation of the “baby place” is carried out in the uterus at the site of attachment of the fertilized egg. As for the site itself, it is the fertilized egg that chooses it on the principle of “the best” for survival (that is, without scars and various neoplasms - and, of course, with a thick endometrium).
In the case when the “best” place is in the lower part of the uterus, the egg is fixed there. This is called placenta previa (its incorrect location).
What are the reasons?
Safety measures for maintaining pregnancy
The following precautions will help the pregnant woman avoid further complications caused by the low location of the placental surface:
- Strenuous activities such as intense cardio or heavy lifting should be avoided. Moderate yoga practice during pregnancy is recommended.
- No sex allowed
- The best position is lying in bed.
Precautions are important because placenta previa can lead to serious complications.
Fetal factors
- Surgical interventions (caesarean section and abortions, removal of fibroids, etc.).
- Multiple pregnancy.
- Uterine fibroids or endometriosis.
- Abnormal structure of the uterus or its underdevelopment.
- Childbirth with complications.
- Endocervicitis.
- Isthmic-cervical insufficiency.
Considering that women giving birth for the first time are unfamiliar with cesarean section and multiple pregnancies (as well as most female diseases), their risk of placenta previa is the lowest.
Video
Kuznetsov Pavel Andreevich, associate professor and head of the CDO, will talk about the peculiarities of the location of the placenta and how this affects the course of labor. Share information about what determines the location of the placenta. He will also give several recommendations for women with this pathology.
In any case, if you undergo the necessary examinations on time, thanks to modern diagnostic methods, you can identify the location of the placenta, its functionality and structural features. A timely diagnosis and prescribed treatment will significantly protect you and your unborn baby. Share your life experience in the comments.
How was your pregnancy with a low-lying placenta? How was the birth? Your story can support other women with the same problem or warn against mistakes made.
Types of abnormal location and placenta previa
In accordance with the specific features of the location of the placenta, specialists (note - based on information obtained after an ultrasound) distinguish certain types of placenta presentation.
- Full presentation. The most dangerous thing. An option when the placenta completely covers the internal os (note: the opening of the cervix). That is, the baby simply will not be able to get into the birth canal (the exit is blocked by the placenta). The only option for childbirth in this case is a caesarean section.
- Incomplete presentation. In this case, the placenta covers the internal os only partially (a small area remains free) or the lower part of the “child’s place” is located at the very edge of the internal os. In most cases, even with incomplete presentation, “classical” childbirth is also impossible - only a cesarean section (the child simply will not fit into part of the narrow lumen).
- Lower presentation. The most favorable option regarding the dangers of pregnancy and childbirth. In this case, the placenta is located 7 (or less) cm from the perimeter of the entrance directly into the cervix/canal. That is, the area of the internal os is not blocked by the placenta (the path “from the mother” is free).
The main types of placenta previa are low, complete and partial.
Treatment of a pregnant woman with a similar diagnosis
The process of treating pathological placental attachment depends on the intensity of bleeding and the volume of blood lost. In the best case, if the discharge was not heavy and stopped quickly, the expectant mother can stay at home and undergo outpatient treatment. A woman is advised to maintain absolute peace and avoid stress and physical activity. Sexual activity with this diagnosis is also excluded, even in the first trimester of pregnancy.
An anomaly for a period of more than 24 weeks requires mandatory treatment in a hospital under the supervision of an obstetrician-gynecologist. Doctors can try to maintain and continue the pregnancy until the due date only if the bleeding was not heavy and the woman feels well. If the pregnancy is long enough, a pregnant woman cannot leave the hospital until the baby is born, even if the bleeding stops.
In a maternity hospital, a woman must observe strict bed rest, undergo a course of medication to improve uterine contractility, treat anemia and exclude fetal-placental insufficiency. If heavy bleeding occurs, surgical delivery is prescribed to avoid anemia, the consequences of low blood pressure and fetal hypoxia. An operation to remove a child can be prescribed for the pregnant woman’s health reasons, regardless of the age and condition of the child.
Childbirth with placenta previa
When the pregnancy has been maintained until the 37th week of pregnancy, the most effective and safe method of delivery is selected. Doctors take into account all aspects of the current situation, taking into account the individual characteristics of the woman and child. Caesarean section is mandatory in case of complete presentation. In this case, the natural course of childbirth is impossible, since the internal os and birth canal are completely closed to the child. Moreover, during childbirth with this position of the placenta, it will gradually exfoliate under the influence of uterine contractions, provoking heavy bleeding.
A caesarean section is routinely performed for partial placenta previa if there are serious complications or risks. For example, the child took a pelvic position, or another position in the womb that is unsuitable for natural childbirth. In addition, the presence of postoperative scars on the uterine tissue and the mother's age exceeding 30 years also suggest a cesarean section. It is also important to take into account the constitution of the pregnant woman - if the structure of the pelvis is too narrow, the natural birth of a child is excluded.
In the absence of serious indications for a cesarean section, the gynecologist can perform a natural birth. For this purpose, early opening of the membranes is carried out to induce labor, and in the absence of bleeding, normal childbirth is carried out. Any complications: delayed labor, sudden bleeding and other factors require immediate surgical intervention.
Opening the amniotic sac allows you to position the baby's head near the entrance to the pelvis, thereby securing the detached part of the placenta. If the placental tissue is correctly pressed against the uterine walls and pelvis, further process of its detachment stops and bleeding stops. Sometimes the bleeding does not stop after the bladder is opened, or the cervix has not yet had time to ripen and open, in which case the obstetrician must perform an emergency caesarean section. If the situation is favorable - the bleeding has stopped and the fetus is in normal condition, the continuation of natural childbirth is stimulated.
When bleeding suddenly begins at an early stage of labor - after the first contractions, an opening of the amniotic sac is also first prescribed, and if complications arise, the child is removed surgically. As practice shows, despite the possibility of a natural birth with partial placenta previa, obstetricians prefer to prescribe a cesarean section. According to statistics, surgery is performed for 80% of women with this diagnosis. This is mainly explained by the desire of doctors to avoid complications during childbirth caused by weak labor, hypoxia and other factors.
Carrying out a natural birth in a pregnant woman with a pathological position of the placenta involves constant monitoring of the child’s condition and monitoring the contractile activity of the uterus. It should be noted that bleeding may resume after a successful birth if the process of detachment of the placenta is disrupted. The fact is that the entire area of the membrane in pathology will be located in the lower segment of the uterus, where the contractile abilities of the organ are significantly reduced, so they cannot ensure normal separation and expulsion of the placenta.
The following factors provoke bleeding:
- Excessive physical activity.
- Vaginal examination.
- Constipation or direct bowel movement with strong straining.
- Visit to the bathhouse or sauna.
- Sexual contact.
- And even a strong cough.
Bleeding can be different, and the volume/intensity does not depend at all on the degree of presentation. In addition, it should be noted that bleeding can be not only a sign, but also a serious complication of presentation when it does not stop for a long time.
Symptoms and signs of complications
Improper attachment of placental tissue in the uterus often causes regular bleeding. It should be noted that bleeding with this pathology occurs at any stage of pregnancy. A pregnant woman may notice brown discharge especially often in the second trimester - when the fetus and uterus are actively growing, injuring the placental tissue. Heavy bleeding with painful sensations in the last stages usually occurs due to increased uterine contractions, which negatively affect the placenta.
Mainly, bleeding provokes repeated detachment of the placental tissue when it does not have time to stretch as the part of the uterus to which it is attached increases. A similar thing happens during active labor, if the placenta prevents the baby from entering the birth canal. It is worth noting that blood is released from damaged vessels of the placenta or uterus, and the fetus itself remains intact, but it may suffer from oxygen starvation. The fact is that the damaged organ, partially separated from the uterine walls, no longer participates in the exchange of oxygen and nutrients.
Detachment, disruption of the integrity of blood vessels and bleeding are usually provoked by strong physical exertion, too sharp a cough, careless actions of the gynecologist during a vaginal examination, rough sexual intercourse, high intra-abdominal pressure after constipation, a hot bath or a visit to the sauna. Heavy discharge may appear suddenly, without any discomfort. It is worth noting that bleeding may periodically stop, or become less intense, stop completely for a while, and then continue in the form of scanty discharge. In the last weeks of the period, discharge becomes frequent and abundant.
Depending on the area of damaged or exfoliated placental tissue, the intensity of bleeding and pain in a woman depends. With extensive detachment, heavy and painful discharge begins. If they become regular, the woman develops anemia. In addition, the pregnancy risks being terminated for the same reason that caused the bleeding. With complete placenta previa in the later stages, premature birth most often occurs.
Low blood pressure during pregnancy
(see also: How to normalize blood pressure during pregnancy) can also be a symptom of abnormal position of the placental tissue. According to statistics, 25-34% of expectant mothers with low blood pressure are diagnosed with pathological attachment of the placenta. Often the pathology is accompanied by gestosis - late toxicosis, which causes complications and disruption of the functioning of many organs of the child. Moreover, the expectant mother’s blood loses the ability to clot normally, thereby provoking even more bleeding. Ultimately, the baby in the womb runs the risk of taking an incorrect position - most often transverse or oblique, or pelvic, which prevents natural childbirth.
Bleeding and its nature
By the type of bleeding during pregnancy, you can determine the type of organ abnormality. When the placental tissue completely blocks the uterine os, the pregnant woman suddenly begins to bleed profusely, but painlessly. Most often this happens at night, so a woman can literally wake up “in a pool of blood.” Intense bleeding often stops as suddenly as it appears, or becomes more scarce. With partial presentation, bleeding usually occurs in the last days before the due date. It is important to note that bleeding is not always a symptom, especially when the bleeding has not stopped for a long time.
Diagnosis of placenta previa - how is it determined?
- Obstetric external examination (note: height of the uterus, position of the fetus).
- Auscultation (in case of presentation, the noise of the placenta/vessels is usually noted directly in the lower part of the uterus near the placenta).
- Gynecological examination with speculum. Palpation determines complete presentation if there is a soft and large formation that occupies all the vaginal vaults, and incomplete presentation - when it occupies only the lateral or anterior vault.
- Ultrasound. The safest method (compared to the previous one). With its help, not only the fact of placenta previa is determined, but also the size, area and structure, as well as the degree of abruption, hematoma and the threat of miscarriage.
Normal fetal development during pregnancy is possible only with the correct functioning and location of the placenta. In some cases (less than 1% of the total number of births), placenta previa may occur, which can greatly complicate childbirth.
Table of contents:
1. Causes 2. Symptoms 3. Why placenta previa is dangerous 4. Diagnosis 5. Dangers of pathology 6. Types of placenta previa 7. How pregnancy and childbirth proceed 8. Reviews 9. Conclusion
The placenta is an organ that is part of the structure of the uterus and contributes to the normal development of the fetus during pregnancy. However, the course of pregnancy is affected not only by the proper functioning of the placenta, but also by its location. Pathologies of the location of the placenta in the uterus are called placenta previa and are an uncommon complication of pregnancy.
Causes
According to the causes of formation, placenta previa can be classified into two groups:
- associated with the condition of the woman’s body,
- associated with the developmental characteristics of the fertilized egg.
In most cases, the cause of placenta previa is the development of pathological changes in the uterine mucosa, leading to disturbances in the normal decidual reaction of the endometrium. These include:
- chronic inflammation of the endometrium,
- surgeries on the uterus, including uterine perforation, conservative myomectomy, cesarean section, etc.,
- developmental abnormalities or underdevelopment of the uterus,
- uterine fibroids,
- complications of the postpartum period,
- multiple births (repeated pregnancy increases the likelihood of placenta previa by 3 times, since by the second birth a woman accumulates a significant number of gynecological ailments).
If the nidation function of the trophoblast is impaired (the delayed appearance of enzymatic processes in it), then the timely grafting of a fertilized egg in the area of the uterine fundus is impossible, and it is grafted only in the lower parts of the uterus. Serious diseases of the liver, kidneys and heart can also lead to placenta previa, as they cause congestion in the pelvic organs. The result of these phenomena is a deterioration in the blood supply conditions in some areas of the uterine wall.
Migration of the placenta is also possible, which can be monitored using ultrasound. The initial stage of pregnancy is characterized by a central presentation of the branched chorion, and by birth the placenta can be located normally or low. In some cases, placenta previa is combined with its tight attachment, causing difficulties with independent separation after childbirth. In general, it is more correct to diagnose placenta previa in the second half of pregnancy, since the position of the placenta may change (except in the case of central placenta previa).
Symptoms
The main symptom of placenta previa is spotting, which is also the main complication of this disease. The type of presentation determines in what period of pregnancy bleeding occurs and its intensity. For example, central placenta previa often leads to the early (2nd trimester) occurrence of intense bleeding, and marginal or lateral placenta previa leads to the onset of light bleeding in the 3rd trimester or during childbirth.
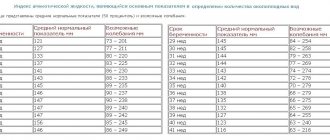
In most cases, the appearance of bleeding is observed in the 28th – 32nd week of pregnancy due to the greater severity of the preparatory activity of the lower segment of the uterus during this period. Between the 16th and 28th weeks of pregnancy, only 20% of cases of bleeding occur.
The main reason for bleeding during placenta previa is the constant increase in the size of the uterus throughout pregnancy: at the beginning its size is equivalent to a matchbox, and by the end of pregnancy the weight of the uterus can reach 1 kg (its volume is equivalent to the volume of the fetus, placenta, amniotic fluid). waters and shells). Such a significant increase in the size of the uterus is possible due to an increase in the volume of each fiber from its structure. The maximum change in the size of the uterus is observed in its lower region and closer to childbirth. The location of the placenta in this place leads to the fact that the placental tissue, which is not elastic, does not have time to adapt to the more rapidly changing dimensions of the uterine wall. The result of this is the detachment of a section of the placenta in which the vessels are damaged and bleeding occurs.
Placenta previa always causes external bleeding, in which blood passes through the cervical canal to the outside, rather than accumulating between its wall and the placenta, forming a hematoma. The onset of such bleeding is usually unexpected and does not cause pain. Thus, they can be distinguished from bleeding that occurs during premature termination of pregnancy (accompanied by cramping pain). The first bleeding inevitably entails subsequent bleeding, occurring with varying frequency, duration and intensity.
The appearance of bleeding after the 26th – 28th week of pregnancy can be caused by physical activity, sexual intercourse and an increase in intra-abdominal pressure, including examination by a gynecologist. Therefore, a gynecological examination of women with placenta previa must be carried out with all precautions and in a hospital setting that provides emergency care if necessary. Prolonged bleeding poses a danger to the life of the child and mother.
Why is it dangerous?
Why is placenta previa dangerous? Anomalies in the location of the placenta are dangerous for both the baby and the mother. And all because the walls of the uterus constantly stretch as the gestation period and the size of the fetus increase. At the same time, the risk of premature placental abruption increases significantly, as a result of which the baby loses contact with the mother’s body and, in the absence of timely medical care, may die from an acute lack of oxygen and malnutrition. The mother is also in danger: during the process of placental abruption, massive bleeding may develop.
Therefore, if at the time of birth the placenta still covers the internal os of the cervix, childbirth naturally is impossible. After all, the process of childbirth begins with the opening of the cervix, accompanied by stretching of the internal os, the outcome of which can be placental abruption, which will lead to bleeding, and the lives of the expectant mother and baby will be at risk.
Diagnostics
In most cases, diagnosis of placenta previa occurs in the 2nd trimester of pregnancy and is based on complaints of periodic bleeding. There is no pain in this case. During the examination (or ultrasound), an abnormal position of the fetus may be revealed, as well as a high standing of the presenting parts of the child above the passage into the pelvis (due to the low location of the placenta preventing them from descending into the underlying part).
The most objective, accurate and safe method of obtaining information about the movement and location of the placenta is ultrasound. In practice, a three-time ultrasound is used - at the 16th, 24th - 26th and 34th - 36th week. If these examinations did not reveal any pathologies in the location of the placenta, then most likely the cause of bleeding is other factors (for example, the presence of pathological lesions of the cervix and vaginal area).
Dangers of pathology
Placenta previa often increases the likelihood of threatened miscarriage and the development of hypotension (stable decrease in blood pressure). Hypotension leads to weakness, decreased performance, fainting and headaches. In addition, bleeding can often cause anemia, which reduces the level of hemoglobin in the blood. As a result, symptoms of hypotension may worsen and fetal development may slow down (growth retardation). In addition, in the first year of life, children of mothers who suffered from anemia during pregnancy have a reduced level of hemoglobin, which causes a decrease in the body's immunity.
The location of the placenta in the lower part of the uterus often leads to the fetus occupying an incorrect position (oblique, transverse). The fetus may not be positioned with its head, as usual, but with its legs or buttocks towards the exit of the uterus. This will require surgical intervention during childbirth, since it is not possible naturally.
Kinds
1. Presentation along the anterior wall . This is more likely not a diagnosis, but simply a statement of fact and it is not at all necessary that any complications will follow, although the risk of their development cannot be completely excluded. Ideally, the placenta should be located along the back wall of the uterus, since this is the place where the uterus is least susceptible to changes during pregnancy.
The anterior wall intensively stretches and becomes thinner, which can lead to placental abruption or its further displacement to the uterine os.
2. Lower placenta previa . Normally, the placenta is located at the bottom of the uterus. We know that the uterine fundus is on top, therefore, the pharynx is on the bottom. When the placenta is located low (low placentation), it is attached closer to the pharynx, reaching it by less than 6 cm.
In this case, 2 scenarios are possible: either the placenta will descend even more, and we can talk about complete or partial presentation, or it will rise up to the bottom along with the walls of the uterus increasing in size. With low placentation, natural childbirth usually occurs without problems.
3. Incomplete (partial) placenta previa . There are two types of this presentation: lateral and marginal. With lateral presentation, the placenta covers the internal os (exit from the body of the uterus into the cervix) by 2/3. At the edge - by 1/3. There is no need to panic if you have been diagnosed with partial presentation.
Very often the placenta moves into the correct position before birth. There is a high probability that the birth will be successful naturally, but everything is decided individually in each case.
4. Complete (central) presentation . The most severe case of abnormal location of the placenta. The placental tissue completely covers the uterine os, that is, the child simply will not be able to enter the birth canal. In addition, the pathology is also dangerous for the life of the mother, since the pharynx area is the most extensible part of the uterus, which cannot be said about the placenta.
The uterus increases in size and placental tissue is detached, which cannot stretch as effectively and quickly. The integrity of the blood vessels is disrupted, which leads to severe bleeding, which, with complete placenta previa, can begin as early as the second trimester and bother the woman until childbirth. Childbirth is possible only by caesarean section.
How is pregnancy and childbirth going?
Caesarean section for placenta previa is required at 38 weeks of pregnancy. In this case, natural childbirth is dangerous due to severe bleeding, which threatens the life of the child and mother and occurs as a result of placental abruption when the child tries to exit. A caesarean section is also prescribed in the following cases:
- placenta previa, accompanied by intense bleeding that threatens life,
- repeated bleeding with severe hypotension and anemia, not eliminated by taking special medications and combined with fetal pathologies,
- the presence of other uterine pathology in case of partial placenta previa.
Natural birth is possible in pregnant women with partial placenta previa who carry the fetus to term. The final location of the placenta is determined when the cervix is dilated by 5 cm. A small partial presentation and minor bleeding require opening of the membranes, leading to lowering of the fetal head and compression of the bleeding vessels. As a result, the bleeding stops and childbirth occurs naturally. If bleeding continues, surgical intervention is required.
Reviews
Allah. Good afternoon I was diagnosed with placenta previa, I asked many times how to raise placenta previa? At the appointment, the gynecologist prescribed me to drink ginipral and chimes “to raise the placenta,” prevent abruption and avoid premature birth. Moreover, she prescribed a long appointment, a control ultrasound at 28 weeks, and if the placenta is below 5 cm, she said that she would need to stay in the hospital and get IVs. Is this prescription legal? I looked at the information about ginipral, there are a lot of side effects, chimes is used to improve the condition of the placenta, but “raising” it with the help of medications, as I read in your answers, is impossible in any case.
Of course, ginipral cannot affect the speed of placenta movement. And if you do not have a threat of late miscarriage (regular cramping pain in the lower abdomen every 10-15 minutes or constant nagging pain), then taking ginipral is not advisable. Curantil especially has nothing to do with low placentation. And why “improve” the condition of the placenta, if, as I understand it, there are no problems with the development of the fetus? I will add that 2.4 cm from the internal os is already good for 23 weeks of pregnancy. Even if the placenta remains positioned this way at the end of pregnancy, you can give birth spontaneously without any threat to your health (although I think your placenta will rise). It is also impossible to influence the speed of placenta movement with any droppers. I think that you are not in vain to be wary - you do not need to take medications.
I have the same problem; an ultrasound at 17 weeks was diagnosed with a low-lying placenta. I was in the hospital, constantly bleeding, without pain. The ultrasound showed that there was no threat of interruption, and there was no detachment either. I was discharged from the hospital, after 2 days the bleeding began again, the gynecologist at the hospital said that this would be the case. But for some reason I’m scared, and I have no one to ask but you. Please tell me, can this happen? ? ? I still have to suffer with the discharge for a long time, because as soon as I see it I become very scared! ! ! Although according to the ultrasound everything is fine, the heart rate is good, there is no detachment or threat of interruption!
A low-lying placenta has the ability to migrate (move) with increasing gestational age. This may be accompanied by bleeding (which is not dangerous). Heavy bleeding before 36 weeks of pregnancy is extremely rare. A child with low placentation also develops normally. We cannot influence the speed of placenta movement with medications or exercises. It just takes time (one month or more). Until the placenta rises, you cannot be sexually active - this can cause bleeding. Otherwise, you can lead a normal lifestyle, excluding heavy physical activity. If the blood stain is less than 10 cm in diameter, then there is no need to worry. If it is more than 10 cm, this is also not scary, but it is already a reason for hospitalization.
I am 14 weeks pregnant. Ultrasound revealed marginal insertion of the choriton, posterior localization. Many people say that during pregnancy the placenta can rise, but the doctor told me that when it is located posteriorly, the choriton does not migrate. Is this true and what does this mean for me and the child? PS The child is very welcome and long-awaited, until 13 weeks there were no problems at all, no tone, no discharge, no pain.
Placenta previa (at the beginning of pregnancy it is called chorion), including marginal attachment, occurs quite often in the early stages of pregnancy (up to 40-50% of all pregnancies). The placenta has the ability to migrate (move) with increasing pregnancy. If the placenta is located on the front wall of the uterus, then this process can occur faster than when the placenta is attached to the back wall. But it is impossible to say that the placenta does not migrate along the posterior wall at all. A child with placenta previa also develops normally. We cannot influence the speed of placenta movement with medications or exercises. It just takes time (one month or more). Until the placenta leaves the internal os, you cannot be sexually active - this can cause bleeding. Otherwise, you can lead a normal lifestyle, excluding heavy physical activity. By the end of pregnancy, placenta previa remains in only 1% of pregnant women. If at 38 weeks the placenta is closer than 2 cm to the internal os, this will require a cesarean section. If above 2 cm, then labor proceeds normally.
Conclusion
Even after the birth of a child, with placenta previa, bleeding may develop, which is due to the low contractility of the tissues of the lower part of the uterus, hypotension and anemia.
The tight attachment of the placenta to the uterus, characteristic of this disease, makes it impossible to separate it independently, which requires manual separation of the placenta under general anesthesia. In rare cases, all the efforts of doctors cannot stop the bleeding. Then, to save the woman’s life, the uterus is removed. Such complications require careful monitoring after childbirth of the condition of women who have had placenta previa, and their compliance with the recommendations of doctors. Tweet Pin It
The course of pregnancy with an incorrect location of the placenta and possible complications
Possible complications of the presentation of the “baby seat” include the following:
- Threat of miscarriage and gestosis.
- Breech/leg presentation of the fetus.
- Maternal anemia and chronic fetal hypoxia.
- Fetoplacental insufficiency.
- Delay in fetal development.
It is worth noting that complete placenta previa in most cases ends in premature birth.
Treatment methods
The course of treatment is prescribed after a complete medical examination and examination of the woman in labor. The duration and features of treatment depend on the duration, location of the child and the type of internal bleeding. Therapy should be carried out under the supervision of specialists.
The course includes the following treatment methods:
- Hospitalization of the expectant mother to preserve and identify the nature of the disease.
- Taking medications that increase blood clotting and relieve spasms.
- Bed rest and rest.
- Limitation on active physical exercise and stress.
- Daily examination of the patient to determine the course of the disease.
- Premature birth and caesarean section are possible.
If a woman in labor experiences severe bleeding and a separation of the baby's place from the walls is detected, then a certain clinical protocol comes into play. The patient is urgently hospitalized and given emergency medical care. This condition is very dangerous for the woman and baby. If internal bleeding is not stopped in time, the baby will die in the womb and the woman will begin to have serious complications that will lead to disastrous consequences. Losing a large amount of blood can lead to a woman's critical condition. Losing 350–400 ml of blood at a time is considered especially dangerous.
If the disease is characterized by a small volume of blood discharge, and the woman’s condition is not life-threatening, then she is not admitted to the clinic; treatment is allowed to be carried out at home, but under the supervision of a gynecologist. If symptoms of anemia, low blood pressure and heavy bleeding appear, the woman is prescribed an emergency delivery via cesarean section.
How does pregnancy proceed with established placenta previa?
- Period 20-28 weeks . If the presentation is confirmed on the 2nd ultrasound, and there are no symptoms, then a regular examination of the expectant mother by her gynecologist-obstetrician is sufficient. Usually, additional drugs are prescribed to reduce the tone of the uterus. If there is even spotting, hospitalization is required.
- Period 28-32 weeks. The most dangerous period for both: with an increase in the tone of the uterus in its lower parts, the risk of detachment and serious bleeding increases with the small size and immaturity of the fetus. In case of marginal or complete presentation, a hospital is indicated.
- Period 34 weeks. Even in the absence of bleeding and severe fetal suffering, the expectant mother is advised to go to hospital until the birth. Only constant supervision by specialists can guarantee a successful outcome of pregnancy and childbirth.
What should a pregnant woman do?
Physical and emotional stress is contraindicated for a pregnant woman with this diagnosis. It is recommended not to make sudden movements, avoid stressful situations and overwork. The expectant mother needs to lead an extremely careful lifestyle, since the health of her baby depends on it. During the period of bearing a child, her body needs full sleep, daytime rest and walks in the fresh air. It is worth including foods rich in iron in your diet to compensate for the deficiency of this element after bleeding. Constipation should be strictly avoided.
A pregnant woman should understand that such a diagnosis of any kind is a serious pathology that requires increased attention and a responsible approach to treatment. Of course, you shouldn’t immediately raise the alarm and suffer from nervous tension, but organizing the right lifestyle before giving birth is necessary. It is important to provide the most comfortable conditions not only for the pregnant woman, but also for the fetus, taking into account all its increased needs. Fortunately, thanks to the achievements of modern pharmacology and timely medical care, most pregnancies with this disorder end in the successful birth of a healthy child.
Prevention of pathology
In order to prevent improper attachment and formation of the placenta, it is necessary to avoid abortions, promptly treat inflammatory processes and diseases of the genital organs, and also normalize hormonal levels. A woman is recommended to regularly visit a gynecologist, have an ultrasound scan and take the necessary tests to avoid complications with diseases of the reproductive system. During pregnancy, the functioning of the cardiovascular system and hematopoietic organs should be monitored and, if necessary, replenishing iron deficiency.
In what cases is a caesarean section performed?
- First of all, with full presentation.
- Secondly, in case of incomplete presentation in combination with one of the factors (several factors) : breech presentation of the fetus or multiple pregnancy, scars on the uterus, narrow pelvis of the mother, polyhydramnios, burdened obstetric history (abortions or miscarriages, operations, etc.), age over 30 years, subject to 1st birth.
- In case of constant bleeding with a serious amount of blood loss (approx. - over 250 ml) and regardless of the type of presentation.
During natural childbirth, the doctor first waits until labor begins (on its own, without stimulants), and after dilating the cervix by one or two cm, opens the fetus/bladder. If after this the bleeding does not stop or even increases in momentum, then an urgent cesarean section is performed.
On a note:
Prevention of presentation, oddly enough, also exists. This is refusal of abortions or their prevention through the use of contraceptives and their correct use, timely treatment of inflammatory diseases and careful attention to women's health.
Take care of yourself and be healthy!
The site Colady.ru warns: self-medication can harm your health! The diagnosis should only be made by a doctor after an examination. Therefore, if you notice any alarming symptoms, be sure to consult a specialist!
When and which doctor to contact
This pathology is mainly accompanied by one characteristic symptom - bloody discharge. In this case, the woman feels well, but she should still immediately contact an antenatal clinic.
The gynecologist must monitor the condition and well-being of the woman and child. If you strictly follow the recommendations of a specialist, the chances of safely carrying and giving birth to a healthy baby are maximum.