Cholecystitis is an inflammation of the gallbladder. Accompanied by disruption of the biliary system and severe stagnation of bile. Statistically, it accounts for 10-12% of cases among diseases of the digestive system and most often occurs in females over the age of 40.
A gastroenterologist diagnoses and treats this disease.
Classification
Cholecystitis is a rather complex disease, since it has several forms and each of them has its own unique symptoms and clinical picture.
Based on etiology, there are two main types:
- calculous (with stones);
- non-calculous (stoneless).
According to the course of the disease, like many other pathologies, cholecystitis can be:
- spicy;
- chronic.
There is also a classification according to the type of inflammation:
- catarrhal;
- purulent;
- phlegmonous;
- gangrenous;
- mixed.
Phlegmonous and gangrenous are classified as a separate category of destructive cholecystitis. They are characterized by severe inflammation, affecting all the membranes of the bladder, and can lead to its rupture.
Causes
The main cause of cholecystitis is an infectious factor. Infection can enter the gallbladder in three ways: through the blood, through the lymph, and from the intestines in an ascending manner.
The primary reasons include the following:
- Inflammatory diseases of the gastrointestinal tract: dysbiosis, pancreatitis, infectious enterocolitis, appendicitis
- Parasitic infections, most often giardiasis or ascariasis
- Inflammatory process in the urinary system: cystitis, pyelonephritis
- Viral liver damage
- Inflammation of the pelvic organs – prostatitis, adnexitis
There are also factors predisposing to the appearance of cholecystitis, which prepare favorable conditions for the occurrence of inflammation of the gallbladder.
- Congenital anomalies of the gallbladder
- Heredity
- Changes in hormonal levels (pregnancy, menstrual irregularities, use of oral contraceptives)
- Allergic reactions
- Decreased immunity
- Sedentary lifestyle
- Overeating, poor nutrition, eating large amounts of fried, spicy and fatty foods
- Alcohol abuse
- Impaired blood supply to the gallbladder
- Changes in the composition of bile
Often chronic cholecystitis is a complication of other diseases. For example, inflammation of the gallbladder can occur against the background of diabetes. Often cholecystitis is detected during the inflammatory process in other organs, for example, with sore throat, pneumonia and other serious diseases. Chronic cholecystitis usually develops against the background of cholelithiasis, pancreatitis, gastritis, and obesity.
Calculous cholecystitis
Calculous cholecystitis (stone cholecystitis) is a combination and mutual action of three pathological processes in the body, including metabolic disorders, stone formation and inflammation.
The formation of stones is the result of pathological processes caused by metabolic disorders. Stones consist of cholesterol, pigments (bilirubin) and lime, almost always they are mixed, with a predominance of cholesterol. Normally, excess cholesterol, bilirubin and calcium are removed in the stool.
Gallstones may have the following structure:
- Crystalline;
- Fibrous;
- Amorphous;
- Layered.
The size of the stones varies. Stones with a diameter of less than 3 mm and having an even shape are easily removed from the body through the intestines.
Stones in calculous cholecystitis are divided into:
- Primary (formed only in the gallbladder);
- Secondary (formed in the bile and intrahepatic ducts).
Chronic calculous cholecystitis is an inflammation of the walls of the gallbladder, which is characterized by periods of remission and exacerbation. The period of exacerbation of chronic calculous cholecystitis should be considered as acute inflammation.
Periods of chronic calculous cholecystitis:
- The period of remission (calm) is due to the elimination of the cause of anxiety (temporary restoration of the outflow of bile into the duodenum);
- The period of exacerbation occurs due to secondary obstruction (blockage) of the duct and/or layering of infection.
Symptoms of exacerbation appear some time after eating fatty foods:
- Feeling of heaviness in the epigastric region, right hypochondrium or navel;
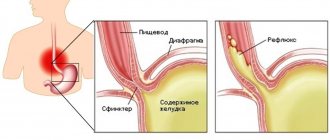
- Dyspeptic disorders (diarrhea and constipation, bitterness in the mouth, heartburn).
Since calculous cholecystitis is based on cholelithiasis (CGD), diagnosis, treatment and prevention of chronic calculous cholecystitis are considered taking into account the course of cholelithiasis.
Clinical picture
Most often, inflammation of the gallbladder occurs as a result of stagnation of bile. It becomes thicker, and gradually clots begin to form in it. This leads to a decrease in its bactericidal properties. In addition, with gradual thickening, stone formation occurs. They have a mechanical effect on the walls of the gallbladder, damaging the protective epithelium and making it more susceptible to the effects of pathogenic microorganisms.
If there are worms in the body, then under their influence the patency of the ducts occurs. And this, in turn, causes stagnation of bile, which is aggravated by the release of toxic metabolic products of worms. As a result of the reaction of the immune system, an inflammatory process occurs.
Non-calculous cholecystitis occurs when pathogenic microflora enters. There are cases of the development of such inflammation as a result of pancreatitis. Pancreatic enzymes irritate the walls of the gallbladder, which makes them very susceptible to the effects of pathogenic microflora.
Etiology and pathogenesis
The pathogenesis of the disease is associated with impaired motor function of the gallbladder. The normal circulation of bile is disrupted, causing it to stagnate and thicken. Later, infection sets in. An inflammatory process occurs. In chronic cholecystitis, inflammation develops more slowly and is sluggish. It can gradually move from the walls of the gallbladder to the biliary tract. With a long course, adhesions, deformations of the bladder, fusion with nearby organs (intestines), and the formation of fistulas can form.
The following factors contribute to the development of chronic cholecystitis:
- congenital disorder of the structure of the gallbladder, decreased tone, physical inactivity, prolapse of certain abdominal organs, pregnancy (factors contributing to mechanically caused stagnation of bile);
- diet violations (overeating, obesity, regular consumption of spicy, fatty foods, alcoholism);
- hypotype biliary dyskinesia;
- intestinal parasites (giardia, amoeba, roundworm, opisthorchid);
- cholelithiasis.
Severity
Based on the severity of clinical manifestations, the following forms of the disease are distinguished:
- Easy. It is characterized by a low-intensity pain syndrome lasting 10-20 minutes, which is self-limiting. Digestive disorders are rarely detected. Exacerbations occur 1-2 times a year and last no more than 2 weeks. The function of other organs (liver, pancreas) is not changed.
- Moderate weight. The painful sensations are persistent with pronounced dyspeptic disorders. Exacerbations develop more often than 3 times a year and last more than 3-4 weeks. Changes in liver function are noted (increased ALT, AST, bilirubin).
- Heavy. Accompanied by pronounced pain and dyspeptic syndromes. Exacerbations are frequent (more than once a month), long-lasting (more than 4 weeks). Conservative treatment does not provide significant improvement in well-being. The function of neighboring organs is impaired (hepatitis, pancreatitis).
The fourth form of pathology
The most dangerous form of acute cholecystitis is the gangrenous form of the disease. It develops rapidly and is quite difficult to diagnose, since patients are in extremely serious condition and cannot describe their sensations. All layers of the wall of the gall sac are involved in the pathological process, necrotic areas are formed that can rupture at any time. It is the danger of bladder perforation that puts gangrenous cholecystitis among a number of critical conditions.
The patient experiences a sharp increase in symptoms of intoxication:
- lethargy;
- headache;
- vomit;
- nausea;
- tachycardia (110-120 beats per minute);
- confusion.
Pallor and dryness of the skin are visually noted. On palpation, the abdominal wall in the hypochondrium and epigastrium is tense, the abdomen is slightly swollen, so it is impossible to palpate the bubble. Due to gangrene of the gallbladder wall, the nerve receptors die off. Therefore, the pain syndrome in such patients is reduced. There is a dull, constant pain under the right rib. The temperature rises above 39.0*. In elderly and senile people, the classic picture is blurred and is not expressed by clear symptoms, which makes timely diagnosis of the disease even more difficult. Hyperthermia does not reach high numbers. If, against the background of a low temperature, the symptoms of poisoning of the body are sharply expressed, it means that total necrosis of the gallbladder has occurred.
Gangrenous form
Regardless of the extent of the necrotic area, the patient undergoes surgery during which the dead areas are removed. In case of extensive gangrene, the entire bladder is removed. Laparoscopic cholecystectomy is performed using a laparoscope and is considered the least traumatic procedure. Since all the surgeon’s movements are displayed on the monitor using a mini video camera, the doctor controls his actions and removes only damaged tissue without affecting healthy areas.
Surgery for cholecystitis
Symptoms of cholecystitis in adults
In general, the symptoms of cholecystitis in adults are quite similar. The manifestations of acute and chronic forms are very different. Therefore, it is worth systematizing the symptoms to make it easier to navigate exactly what form of inflammation the patient has and how it can be treated.
How does acute cholecystitis manifest?
The acute form of cholecystitis is manifested by severe pain in the right hypochondrium (it can radiate to the back/under the right shoulder blade/to the left side of the body). The pain becomes more pronounced after eating. The patient also complains of:
- constant nausea;
- a feeling of bitterness in the mouth, an unpleasant metallic taste;
- temperature increase;
- vomiting (single/multiple);
- loose stools (usually once).
Signs of chronic cholecystitis
The chronic form of cholecystitis takes a long time to develop. With it, exacerbations alternate with remissions. Among the most common symptoms of chronic cholecystitis:
- mild aching pain in the right hypochondrium (may radiate to the right shoulder blade or shoulder);
- bloating;
- rare stool;
- bitterness in the mouth;
- dry mouth in the morning;
- increased fatigue, weakness;
- nausea (may worsen after eating).
Chronic cholecystitis is dangerous because patients may simply not pay attention to its signs for a long time. But the longer the inflammation lasts, the more difficult treatment will be during an exacerbation. If not treated promptly, this can lead to complete removal of the gallbladder. Therefore, you should contact a gastroenterologist if you experience discomfort in the liver area.
Signs of calculous cholecystitis
Calculous cholecystitis is often asymptomatic. Its acute form begins with an attack of biliary colic - pain in the right hypochondrium. The patient's condition may worsen after eating fatty or spicy foods or drinking alcohol. Soon after the painful symptom, vomiting of gastric juice begins.
Also for calculous cholecystitis:
- urine darkens and becomes cloudy;
- blood pressure decreases;
- heart rate increases;
- symptoms of intoxication are observed;
- a bitter taste appears in the mouth;
- the skin turns slightly yellow;
- diarrhea occurs.
Pain in the hypochondrium intensifies when coughing or changing body position.
Symptoms of catarrhal cholecystitis
Catarrhal cholecystitis makes itself felt:
- repeated vomiting mixed with bile;
- severe pain in the right hypochondrium (radiating to the lower back, right half of the neck or shoulder blade);
- arterial hypertension;
- white coating on the tongue;
- pain when feeling the abdomen;
- temperature rise.
Symptoms of gangrenous cholecystitis
The presence of the following symptoms allows the doctor to assume that a patient has a gangrenous form of cholecystitis:
- high body temperature;
- loose stools;
- frequent vomiting;
- very severe abdominal pain;
- dry mouth;
- lack of appetite;
- fainting;
- weakness.
Signs of purulent (phlegmonous) cholecystitis
The purulent form of inflammation of the gallbladder is characterized by:
- high temperature;
- flatulence;
- pain in the hypochondrium on the right side;
- attacks of nausea;
- vomiting (can be regular or one-time).
Duration of treatment and full recovery
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
By eliminating factors that provoke the appearance of chronic cholecystitis, gallstone disease can be prevented. To do this, it is important to constantly adhere to the principles of proper nutrition, use pharmacological drugs and phytotherapeutic agents prescribed by a doctor, receive proper sanatorium-resort treatment in a timely manner, and carry out regular sanitation of chronic infectious foci in the body.
These actions will help avoid relapses of acute cholecystitis and exacerbations of chronic cholecystitis, but cannot guarantee that the disease will never manifest itself again, even despite the long-term absence of any symptoms. In the treatment of cholecystitis, it is not the speed that is important, but the regular actions of the doctor and the patient, aimed at prolonged preservation of the health of the gallbladder and bile ducts. Therefore, the duration of treatment can only be judged in each specific case of the disease.
Regarding the issue of complete cure of cholecystitis, it is important to understand that with this disease irreversible changes in the walls of the gallbladder occur, therefore conservative methods cannot ensure complete recovery. However, when using complex therapy for the disease, stable remission can exist for a very long time, which explains the need to strictly follow all doctor’s instructions even after stopping drug treatment.
Complications
If cholecystitis, the symptoms of which are pronounced, is not treated in time, this can lead to serious complications for the patient’s life. First of all, this is perforation (rupture), after which inflammation of the abdominal cavity occurs due to bile entering the peritoneum. Symptoms: nausea, vomiting, sharp and constant abdominal pain, fever. Recognizing perforation and fluid in the peritoneum is possible only with the help of ultrasound.
Another complication of cholecystitis is a peri-vesical abscess. This is a condition in which suppuration occurs in the walls of the gallbladder and the tissues around it. Symptoms of this process are high body temperature, enlargement of the diseased organ, acute pain in the right hypochondrium.
If pus collects only in the gallbladder, it is called an empyema. When there are rocks and sand in the bubble, it makes things more difficult. Using an ultrasound, you can see an increase in its size. The patient suffers from fever, tension in the anterior abdominal wall and pain.
How to protect the gallbladder from inflammation
To prevent cholecystitis at any age, it is important to follow a proper diet. You should also avoid factors that will contribute to the occurrence of an inflammatory process in the gallbladder. These factors include obesity, physical inactivity, intestinal infections, and stress.
To maintain the body in a healthy state and control the functionality of the biliary system, it is necessary to adhere to a healthy diet, avoid overeating, lose weight quickly, move a lot (and regularly, which is important), and avoid stressful situations.
Diagnostics
The main difficulty in verifying a diagnosis is considered to be determining the type and nature of the disease. The first stage of diagnosis is a consultation with a gastroenterologist. Based on complaints, studying the medical history, and conducting a physical examination, a specialist can establish a preliminary diagnosis. Upon examination, positive symptoms of Murphy, Kera, Mussi, and Ortner-Grekov are revealed.
To determine the type and severity of the disease, the following examinations are carried out:
- Fractional duodenal intubation. During the procedure, three portions of bile (A, B, C) are collected for microscopic examination. Using this method, you can evaluate the motility, color and consistency of bile. In order to detect the pathogen that caused bacterial inflammation, the sensitivity of the flora to antibiotics is determined.
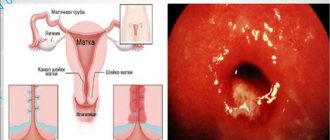
- Ultrasound of the gallbladder. It is the main diagnostic method, it allows you to determine the size and shape of the organ, the thickness of its wall, contractile function, and the presence of stones. In patients with chronic cholecystitis, thickened sclerotic walls of the deformed gallbladder are visualized.
- Laboratory blood test. In the acute period, neutrophilic leukocytosis and accelerated ESR are detected in the CBC. A biochemical blood test shows increased levels of ALT, AST, cholesterolemia, bilirubinemia, etc.
- Cholecystocholangiography. Allows you to obtain information about the functioning of the gallbladder and biliary tract in dynamics. Using the X-ray contrast method, impaired motor function of the biliary system, stones and deformation of the organ are detected.
In doubtful cases, hepatobiliary scintigraphy, FGDS, MSCT of the gallbladder, and diagnostic laparoscopy are additionally performed to study the functioning of the biliary tract. Differential diagnosis of cholecystitis is carried out with acute diseases accompanied by pain (acute pancreatitis, appendicitis, perforated gastric and duodenal ulcers). The clinical picture of cholecystitis should be distinguished from an attack of renal colic, acute pyelonephritis, and right-sided pneumonia.
Treatment of the disease in the acute stage
Treatment methods depend entirely on the symptoms of cholecystitis in women. Treatment of chronic pathology in the remission stage is significantly different from the fight against the disease during an exacerbation.
If a patient has an attack, then therapy is aimed at eliminating symptoms and stopping the pathogenetic reactions of the disease. In the remission stage, treatment involves preventing relapses.
Drug therapy for chronic cholecystitis during exacerbation is based on the following pharmaceuticals:
- Antibiotics: Erythromycin, Doxycycline, Ciprofloxacin, Biseptol, Furozolidone, Metranidazole, Oxacillin.
- Antispasmodics: “Papaverine”, “Pitofenone”, “Drotaverine”, “Platifillin”.
- Choleretic drugs: “Sorbitol”, “Nicodin”, “Allohol”, “Cyqualon”.
- NSAIDs: Baralgin, Spazgan.
- Propulsants (medicines that stimulate peristalsis), for example Domperidone.
- Antiemetics: Cerucal, Diprazin.
- Multienzyme medications: Festal, Pancreatin.
- Sedative medications: tincture of valerian, motherwort.
An event such as tubeless tubing is very popular in the fight against chronic cholecystitis. Its essence is to flush the ducts with subsequent stimulation of the bile secretion process.
How to relieve an attack of cholecystitis?
When cholecystitis and its acute symptoms appear, treatment is necessary. Therefore, the first thing you need to do is call an emergency doctor.
While waiting for the doctor to arrive, you should:
- Ensure a state of rest for the patient;
- Give a pain reliever (antispasmodic);
- Give the patient mineral water without gas (sodium chloride), especially after vomiting;
- Apply a cold compress.
What should not be used during an attack of cholecystitis and its symptoms before treatment:
- Apply a heating pad;
- Use narcotic painkillers or analgesics;
- Drink alcoholic beverages;
- Do an enema;
- Use any medications other than antispasmodics.
How to give first aid
First of all, during an attack of acute cholecystitis, the patient should call an ambulance, and before it arrives, the patient must be placed on his right side and ensured rest.
When providing first aid, under no circumstances should you feed the patient anything, warm his stomach, try to rinse his stomach or intestines, or give any medications. Any of the above actions can change the clinical picture of the disease, which will complicate the diagnosis and prevent the prescription of effective treatment. After the patient is taken to the hospital, doctors first carefully examine him, offer options for relieving pain through antispasmodic injections, carry out detoxification procedures and prevent the possibility of developing the process of bile stagnation. Only after providing first emergency aid can specialists begin to develop an algorithm for effective treatment of the patient and prescribe diagnostic procedures. If first aid was not provided to the patient or was provided incorrectly, there is a risk of developing serious complications.
Treatment of acute cholecystitis
Treatment of acute cholecystitis in adults is carried out in a hospital setting, strict bed rest is indicated. During the first 24-48 hours, gastric contents are evacuated through a nasogastric tube. During this period, fluid is administered intravenously.
After the signs of acute inflammation subside, the probe is removed and the patient is prescribed a water-tea break for several days, and then diet No. 5a according to Pevzner. 3-4 weeks after all the symptoms of the disease have subsided, the diet is expanded, and the patient is transferred to diet No. 5. Diet for acute cholecystitis is one of the main methods of treatment. Frequent meals in small portions promote good bile flow. To reduce the load on the liver and biliary system, it is reasonable to reduce the content of animal fats, seasonings, and essential oils in the diet.
Western experts have a different approach to organizing a diet for acute cholecystitis. They also limit the fat content in the diet, but recommend eating no more than 2-3 times a day with a mandatory 12-16-hour break at night. Conservative treatment of acute cholecystitis includes performing a perinephric novocaine blockade according to Vishnevsky to relieve acute pain, as well as prescribing antispasmodic and antibacterial drugs.
In 90-95% of patients, obstruction of the bile duct is caused by a calculus (stone). In other cases, a violation of the outflow of bile occurs due to swelling of the walls of the bile duct caused by an inflammatory process or blockage by parasites or a tumor.
After relief of the symptoms of acute cholecystitis in the presence of stones in the gallbladder, lithotripsy is recommended, i.e. dissolution of stones (with ursodeoxycholic and chenodeoxycholic acids).
Surgical treatment of acute cholecystitis is carried out for the following indications:
- emergency – development of complications (peritonitis, etc.);
- urgent – ineffectiveness of conservative therapy carried out within 1-2 days.
The essence of the operation is to remove the gallbladder (cholecystectomy). It is performed using both traditional open and laparoscopic methods.
Treatment in women
Features during pregnancy
Therapy for cholecystitis during pregnancy is selected with the participation of the gynecologist observing the woman, since this treatment should combine both high efficiency and complete safety for the development of the child.
Treatment of cholecystitis in pregnant women is fundamentally no different from generally accepted measures, but takes into account medications acceptable during pregnancy.
Therapy during breastfeeding
The occurrence of pain in the right hypochondrium in new mothers is quite common. Cholecystitis can occur when metabolic processes are disrupted due to childbirth. If a woman was diagnosed with stones in the gallbladder or ducts before pregnancy, then cholecystitis after childbirth is very likely. In this case, conservative therapy is most often used, but a woman logically has a question about the safety of breastfeeding her child.
Modern doctors do not see an urgent need to stop lactation when treating cholecystitis in the postpartum period. Firstly, this does not always require the use of antibiotics, since more often cholecystitis in this case manifests itself in a chronic course. But even if antibiotic therapy is urgently needed, doctors today can offer their patients several types of effective drugs that will not affect the baby in any way and will not pass into breast milk. The main therapeutic treatment for cholecystitis during lactation will be strict diet therapy. Prohibited and permitted products must be selected by the gastroenterologist together with the gynecologist to ensure both the restoration of the patient’s gallbladder and the normal quality of breast milk.
Treatment of chronic cholecystitis
Without the formation of stones, treatment of chronic cholecystitis in adults is always carried out using conservative methods, the main one of which is dietary nutrition (diet 5 - split meals with a sufficient volume of liquid, mineral water). If there are gallstones, limit hard work, physical overload, and bumpy driving.
At home, the following drugs are used to treat chronic cholecystitis:
- Antibiotics, most often broad-spectrum or cephalosporins
- Enzyme preparations - Pancreatin, Mezim, Creon
- Detoxification - intravenous infusions of sodium chloride, glucose solutions
- NSAIDs - sometimes used to relieve inflammation and pain
Choleretic drugs are usually divided into:
- Choleretics are drugs that enhance the formation of bile. Preparations containing bile and bile acids: allohol, lyobil, vigeratin, cholenzyme, dihydrocholic acid - hologon, sodium salt of dehydrocholic acid - decholin. Herbal preparations increase the secretion of bile: flakumin, corn silk, berberine, convaflavin. Synthetic drugs: osalmide (oxafenamide), hydroxymethylnicotinamide (nicodine), cyclone, gymecromone (odeston, holonerton, cholestil).
- Cholekinetics are divided into: promoting the secretion of bile and increasing the tone of the gallbladder (magnesium sulfate, pituitrin, choleretin, cholecystokinin, sorbitol, mannitol, xylitol) and cholespasmalytics, reducing the tone of the biliary tract and sphincter of Oddi: drotaverine hydrochloride, no-spa, olimethine, atropine, platiphylline, aminophylline, mebeverine (duspatalin).
During periods of exacerbation, herbal medicine is very widely used, in the absence of allergies to it - decoctions of chamomile, dandelion, peppermint, valerian, calendula. And during periods of remission, it is possible to prescribe homeopathic treatment or herbal medicine, but with other herbs - yarrow, marshmallow, tansy, buckthorn.
It is very important to follow a strict diet after an exacerbation of cholecystitis, then the symptoms gradually subside. In addition to a diet for gallstones and cholecystitis, it is also recommended to periodically apply tubages with xylitol, mineral water or magnesium; physical therapy is effective - electrophoresis, reflexology, SMT therapy.
In case of calculous chronic cholecystitis with pronounced symptoms, it is recommended to remove the gallbladder, the source of the growth of stones, which can pose a threat to life if they move. The advantage of chronic cholecystitis with stones from acute calculous cholecystitis is that this operation is planned, it is not an emergency measure and you can safely prepare for it. Both laparoscopic surgery and cholecystectomy from a mini-access are used.
When surgery is contraindicated, sometimes with chronic cholecystitis, treatment may consist of the method of crushing stones - shock wave lithotripsy; this extracorporeal procedure does not remove stones, but simply crushes, destroys them, and often causes them to re-grow. There is also a method for destroying stones using salts of ursodeoxycholic and chenodeoxycholic acids; in addition to the fact that this therapy does not lead to a complete cure, it is also quite long in time and lasts up to 2 years.
Physiotherapy for cholecystitis
Physical exercises and massages are presented for informational purposes. We do not recommend using them without a doctor's advice. We recommend reading: “When can physical exercise and massage pose a threat to health?”
Physiotherapeutic techniques are used to treat cholecystitis in remission. Experts call UHF therapy, mud therapy, mineral water therapy, diathermy and others the most effective physiotherapeutic methods in this case. In case of remission of pathology, patients are often recommended sanatorium-resort treatment in Essentuki, Borjomi.
Therapy can be lengthy and must be supervised by medical personnel.
Mineral water
Mineral water is part of the complex treatment of cholecystitis, so its use should be fully supervised by the attending physician. Drinking mineral waters from springs provides the optimal concentration of salt composition, however, in urban environments, you can also use bottled water, packaged in glass and sold in pharmacies.
With the help of mineral water, it becomes possible to stimulate the processes of bile formation and bile outflow in the human body. Thus, bile stagnation is eliminated, and along with it, pathogenic microflora leaves the body.
For cholecystitis, mineral waters are used, depending on the type of gallbladder tone disorder:
- in case of hypotension of the biliary tract, taking alkaline mineral water with a high concentration of salts is indicated;
- for hypertension - the concentration of salts in mineral water should be minimal;
- hypotonicity of the gallbladder requires complex therapy, which will include diet and the use of mineral waters.
Such therapy increases the fluidity of bile, thereby reducing the levels of bilirubin and cholesterol in the blood.
For effective treatment, it is recommended to flush the gallbladder with mineral water on the eve of therapeutic procedures, and then this must be repeated regularly once a week 1.5 hours before meals, when bile is released into the gall bladder, and again 30 minutes before meals. This promotes the excretion of bile into the intestines, where it can take part in the digestive process.
During treatment, mineral water is taken orally warm or hot - 30-50 degrees. You can only heat water in a water bath, and drinking it cold is strictly prohibited, since in this case it can cause spasm of the bile ducts and severe pain. Hot mineral water reduces the intensity of pain.
The amount of water used at one time should not exceed 200-250 milliliters. Sometimes in the first stages of treatment, doctors recommend taking only 100 milliliters of this water. The volume of mineral water used to treat cholecystitis can be calculated in each specific case of the disease, taking into account that the patient needs to use 4 milliliters of mineral water for every kilogram of his weight. You need to drink medicinal water 3 times a day, slowly, in small sips. The treatment period is usually 1 month. Contraindications to treatment with mineral waters include diseases of the gastrointestinal tract, post-stroke or post-infarction conditions.
Mineral waters can also be used in the complex therapy of cholecystitis and as a raw material for outpatient procedures, for example, for duodenal drainage.
In the case of cholecystitis, the introduction of mineral water using a probe into the duodenum can help the process of releasing bile into the intestinal area, and with long-term therapy, it can cleanse and improve the liver, eliminate traces of mucus and bile, and stop the inflammatory process.
In addition to the above methods of use, when treating cholecystitis, patients are also advised to take hydrogen sulfide baths, which have a positive effect on the nervous system, improve the metabolism of each organ, reduce inflammation in cholecystitis, relieve pain and improve the functionality of the body’s biliary system.
Therefore, mineral waters are a very effective treatment for cholecystitis, which, if used correctly, will help prevent inflammation in the gallbladder, reduce the concentration of bile, remove it and normalize the functionality of the gastrointestinal tract.
Gymnastics for cholecystitis
A sedentary lifestyle and lack of adequate physical activity contributes to the process of stagnation of bile in the gallbladder. Special gymnastics will help get rid of the manifestations of cholecystitis, activate blood circulation processes in the peritoneum, stimulate bile outflow and improve intestinal motility. All exercises aimed at activating the gallbladder must be performed in the morning, when the stomach is empty and there is no bile in the intestines.
Complex therapeutic exercises include breathing exercises that develop diaphragmatic breathing, which is effective for all organs in the abdominal cavity and strengthens the muscles of the diaphragm. These exercises are designed to provide stress on the abs, some of them should be performed in a position on the right side or on the stomach. Such gymnastics can be done on a gymnastic ball, lying on your stomach, on which you can swing and enhance blood circulation in the liver and gall bladder. Also among the exercises for the treatment of cholecystitis you can find turns and bends of the torso, which activate the gallbladder and stimulate choleretic processes.
When is surgery needed?
Surgery is often prescribed for acute forms. Unlike acute appendicitis, the decision to perform surgical manipulation is not made immediately. Doctors can monitor his condition for several days, do a biochemical analysis of the contents of the gallbladder, conduct an ultrasound, take blood for analysis, and only after finding out the full picture of the development of the disease, a final decision is made.
In what cases is surgery inevitable:
- If the attack does not disappear, conservative methods poorly stop it, and over time the intensity only increases;
- The cavities of the gallbladder are filled with pus with pathogenic microflora;
- There is a risk of developing peritonitis or it has already begun;
- With frequent severe attacks of biliary colic;
- Cholelithiasis, when it is not possible to achieve the outflow of bile with the help of medications and physiotherapy.
Pancreatitis developing against the background of the disease is also in favor of surgery. There are different types of surgical intervention:
- Complete or partial removal of the bladder;
- Burning of the mucous membrane;
- Application of an artificial fistula. This method can be considered an emergency measure; it is required if the abundance of pus and bile threatens the life and health of the patient. It helps empty the gallbladder of bile and pus.
Surgical intervention
The indication for surgical treatment is the ineffectiveness of conservative therapy, when biliary colic occurs every time with the slightest error in following a strict diet. In this situation, medications can alleviate the condition only for a short time, then the symptoms resume. The patient should be referred to a surgeon to consider surgical removal of the gallbladder.
The operation to remove the gallbladder is called cholecystectomy. It is carried out for acute calculous cholecystitis, choledocholithiasis and complicated forms of cholecystitis. When the bile ducts are blocked by a stone, the patient has clinical manifestations of obstructive jaundice and is plagued by frequent attacks of biliary colic. In cases of planned cholecystectomy, when there are no complications and no risk factors, the operation is performed endoscopically - through small incisions, 3 tubes are inserted into the abdominal cavity for illumination and manipulation. The minimal trauma of the operation allows the patient to fully recover in 2 weeks and go home within two days after the intervention.
In complex cases and the presence of exacerbations, surgeons perform a classic operation to remove the gallbladder, with access to the bladder through an incision under the right hypochondrium.
In severe complicated cases of the disease, when there is a risk of developing gangrene, gallbladder, bladder perforation and peritonitis, doctors can perform surgery through laparotomy access, through the anterior wall of the patient’s abdomen, for better visualization of possible complications and their elimination. However, these operations are performed quite rarely in modern conditions. After cholecystectomy, the patient must be re-examined by a gastroenterologist (sometimes a therapist), and also undergo rehabilitation and subsequent maintenance therapy. Diet therapy for cholecystitis is a mandatory component of treatment both before and after surgery.
Folk remedies
Folk remedies that help with chronic cholecystitis:
- Add 2 teaspoons of immortelle flowers, 2 teaspoons of lingonberry leaves, 3 teaspoons of knotweed and 1 teaspoon of chamomile flowers to boiling water. Let it brew for 2-3 hours. Take ½ glass three times a day.
- Tincture from a mixture of herbs. Mix decoctions of peony (30 ml), valerian (30 ml), hawthorn (30 ml), calendula flowers (25 ml), peppermint (20 ml), wormwood (30 ml) and motherwort (25 ml). A fresh cocktail should be taken 1/3 teaspoon three times a day, half an hour before meals, for several days. Then it is recommended to make a tincture from the mixture - add alcohol, close it and put it in a dark place for a week. Dilute one tablespoon of tincture with a spoon of water, take 3-4 times a day for a week.
- Mix St. John's wort and immortelle flowers in proportions 1:2. Brew with boiling water, leave to steep for 5-8 hours, then simmer over medium heat for 3-5 minutes. Drink ½ glass twice a day.
- Take a small handful of milk thistle seeds and chew on an empty stomach. The herb improves the choleretic function of the organ.
Herbal medicine is an excellent supportive therapy, part of a comprehensive treatment. Depending on which recipe and herbs you use, there will be a different effect - anti-inflammatory, improving the flow of bile, relieving pain, improving the entire digestive process, etc.
Diet
Diet No. 5, recommended for patients with cholecystitis, includes:
- Eating in fractional portions 5-6 times a day. It has been proven that this pattern of eating improves the flow of bile and normalizes the functioning of the gallbladder. In this case, the patient must follow a daily routine - eat at the same time.
- Consumption per day is from 85 to 90 g of proteins (half of which should be vegetable), from 70 to 80 g of fat (1/3 should be of vegetable origin), from 300 to 350 g of carbohydrates (no more than 90 g of sugar).
- Consume less than 10 g of salt per day.
- Drink about 2.5 liters of clean water per day.
- Complete abstinence from alcoholic beverages.
- Eating warm food (hot and cold are not recommended).
List of allowed and prohibited foods for every day:
| What not to eat if you have cholecystitis | Products allowed for cholecystitis |
Persons who have been diagnosed with cholecystitis must be from:
| The list of products allowed for inflammation of the gallbladder includes:
|
The calorie content of the diet of a patient with cholecystitis should be from 2100 to 2500 kcal. But, if the patient is overweight, these figures are calculated individually.
Nutritional Features
The text is for informational purposes only. We strongly urge you not to use diets, resort to any therapeutic menus or fasting without medical supervision. We recommend reading: “Why you can’t go on a diet on your own.”
The main goal of the diet for the disease in question is to limit the load on the biliary organs, improve the process of bile production, and normalize the functioning of all organs of the gastrointestinal tract.
Dietary features for cholecystitis include the requirement to eat frequently (at least 5 times a day), and at strictly prescribed times.
The fragmentation of nutrition and its structure over time will have a beneficial effect on the production of bile in the gallbladder. It is also necessary to build your diet in such a way that the daily calorie content of food is within the range of 2100-2500 kilocalories, which would be distributed in the required proportions to all substances necessary for human life - proteins, carbohydrates, fats, vitamins and microelements.
When eating food, it is important to maintain its temperature, which should not be too high or low. The fact is that the thermal regime of food is very important for the normal functioning of the entire gastrointestinal tract, so you should only eat food that is comfortable in temperature. At the same time, it is necessary to drink enough clean water throughout the day, since it activates choleretic processes and stabilizes renal function. The most optimal dosage is to drink 2.5 liters of water per day.
In addition to the above restrictions, it is worth mentioning the excess salt content in cooked food and finished products. With cholecystitis, it promotes thickening of bile, which prevents its outflow from the gallbladder, provoking attacks of biliary colic and increasing the risk of stone formation, so limiting salt in the diet must be observed. Alcohol can also have a very bad effect on the development of cholecystitis. It promotes the formation of stones and, as a consequence, the occurrence of complications in cholelithiasis.
Prevention
Attention should be paid to preventive measures to avoid the manifestations of cholecystitis. Pay attention to your diet - eat fresh, healthy foods, avoid excessively fatty, spicy, smoked and salty foods. Eat at least five times a day in small portions at fixed times (such a simple technique will allow all organs of the gastrointestinal tract to function correctly, and therefore prevent the possibility of failure).
Every day, devote at least half an hour to physical activity (perform exercises consisting of 7-10 exercises). Watch your body weight (extra pounds are not beneficial). The use of aggressive diets and excessive physical activity will provoke an existing disease or lead to its primary manifestation. It is better to lose weight gradually, losing 500-700 grams weekly.
The disease is serious, and if you do not recognize it and do not start treating cholecystitis on time, it can aggravate the situation - lead to complications, chronic forms, and disability.
Forecast
The prognosis for uncomplicated forms of acute cholecystitis, provided timely medical care is provided, is generally favorable. Acute non-calculous cholecystitis usually ends in complete recovery and only in a small percentage of cases becomes chronic; the likelihood of chronicity of acute calculous cholecystitis is much higher.
The prognosis sharply worsens with the development of complications (peritonitis, peri-vesical abscess, empyema). The probability of death in this case is, according to various sources, 25–50%.
Why does vomiting with bile occur: causes and treatment in adults Light-colored feces in an adult: causes and treatment Pancreatitis: symptoms, treatment and diet for pancreatitis Toxic liver hepatitis - symptoms and treatment