Ischemic stroke is a sudden disruption of brain tissue caused by a cerebrovascular accident. It is important to determine the course of the disease in time and receive treatment. The risk of occurrence depends on lifestyle, heredity, gender and age of the patient, as well as the presence of chronic diseases. You should know in advance what ischemic stroke is, its symptoms, consequences and treatment. At the first signs of illness, you should consult a doctor.
Classification of ischemic strokes
Since ischemic stroke is often the outcome of one of the previous cardiovascular diseases, several types are distinguished in neurology:
- Cardioembolic is a type of ischemic stroke that occurs due to arrhythmia, previous myocardial infarction, or existing valvular heart disease.
- Lacunar is a type of ischemic stroke caused by minor occlusion of the arteries.
- Atherothrombotic - its cause is atherosclerosis of large arteries, which causes arterial embolism.
- An ischemic stroke of unknown origin is an ischemic stroke, the root cause of which has not been established; it is possible that there are several reasons that could lead to the development of this disease, so it is difficult to immediately make an accurate diagnosis.
- Ischemic stroke, which is related to rare causes: dissection of arterial walls; blood hypercoagulation or non-atherosclerotic diseases.
Ischemic stroke is also classified depending on the time of occurrence. For example, there are 5 periods of ischemic stroke:
- Acute: occurs in the first three days. It should be said that in the first three hours after a stroke, the patient can benefit from thrombolytic drugs that are administered systemically. If the symptoms begin to regress, then on the first day of the disease a diagnosis of transient ischemic attack is made.
- Acute: lasts up to 4 weeks.
- Early recovery period: can last up to 0.5 years.
- Late recovery period: lasts up to two years.
- Time of residual effects: manifests itself after 2 years from the moment of illness.
It should also be noted that in practice, minor stroke is also common, which is characterized by regressive symptoms observed within 3 weeks from the onset of the disease.
Consequences of the disease
The consequences are directly related to how extensive the area of brain tissue damage is and how quickly medical assistance was provided. Urgent consultation with a doctor plays an important role in maintaining and restoring circulatory functions. Among the main complications after an illness are:
- disturbance of urination and defecation;
- epilepsy;
- cerebral paralysis;
- thrombosis;
- infectious complications caused by long-term rehabilitation;
- cognitive impairment;
- dysfunction of the musculoskeletal system;
- paralysis of the limbs and the whole body;
- facial asymmetry.
The consequences of a cerebral infarction can be different, depending on the location of the pathology. Thus, among the complications after an ischemic stroke of the right lobe of the brain there are:
- impaired concentration;
- speech disorders;
- short-term memory loss.
Complications after a stroke of the left hemisphere:
- pronounced mental disorders;
- disorientation in time and space;
- memory loss.
An ischemic stroke can provoke cerebral edema, necrosis of the posterior and middle parts of the brain stem, and cause secondary hemorrhage in the brain, which, in turn, will cause death.
Etiology and pathogenesis of ischemic stroke
Since in medical practice ischemic stroke is not considered as an independent disease, there is no need to talk about any etiological cause that causes it.
However, doctors mention risk factors that affect the incidence of this disease, including:
- Modifiable factors: arterial hypertension, diabetes mellitus, asymptomatic lesions of the carotid arteries, myocardial infarction.
- Non-modifiable factors: heredity.
In addition to these two large groups of risk factors, there are also factors caused by lifestyle: stressful situations, prolonged psycho-emotional stress, poor standard of living, low physical activity, excess weight, bad habits.
A special sequence of biochemical changes occurring in the patient’s body, and in particular in the brain, is usually caused by focal cerebral ischemia (acute form), which entails various kinds of disorders at the tissue level, which causes the death of brain cells or cerebral infarction .
If we talk about the nature of the changes that occur during an ischemic stroke, it depends on the level and duration of reduced activity in the cerebral blood flow, as well as on how sensitive the brain substance is to ischemic processes.
It is interesting that the degree of reversibility of changes occurring in the tissue will be determined at each pathological stage by the level of decrease in cerebral blood flow, as well as by such an indicator as its duration, together with those factors that affect the sensitivity of the brain to damage of a hypoxic nature.
There are several medical terms that are controversial in their definition. In order to debunk all doubts, let's name them.
In neurology, the core of the infarction is the zone of irreversible damage, while the penumbra is usually called the zone of ischemic damage, which is characterized by a reversible nature. In the study of a particular case of ischemic stroke, doctors pay considerable attention to the duration of the existence of the penumbra, since over time those changes that were previously reversible become irreversible.
Another important term is the “oligemic zone,” which is an area with a preserved balance between the needs of the tissue and the processes that provide it with these needs, even despite reduced cerebral blood flow. Such zones usually exist for a very long time, without moving into the core of the infarction. This term should not be confused with the term "penumbra".
Theory
Ischemic stroke is also called “cerebral infarction.” This definition fully corresponds to the pathogenesis occurring in the organ during insufficient blood supply.
The word “ischemia” itself means a deficiency of blood supply to an organ or tissue due to a decrease or complete cessation of arterial blood flow to this part of the body.
The word “stroke” refers to a violation of the blood circulation in the brain, which is often accompanied by loss of consciousness or paralysis. If blood vessels burst simultaneously with this phenomenon, rapid death of brain cells occurs.
The process of tissue destruction does not stop even after normal blood flow has been restored. It is for this reason that it is extremely important that a person receives the necessary medical care in a timely manner. After suffering a cerebral infarction, the patient needs rehabilitation. It is an important part of general therapy, preventing possible complications.
Women are more susceptible to the occurrence of pathology.
Clinical picture of ischemic stroke
Clinical manifestations of ischemic stroke are quite varied and depend on the location of the lesion and the area of brain damage. Most often, the lesion is located in the carotid region (accounting for more than 80% of cases of ischemic stroke), less often in the vertebrobasilar region.
The main feature of a heart attack in the area of blood supply to the middle type cerebral artery is the presence of a collateral blood supply system. If we talk about such a phenomenon as occlusion of the proximal part, then in the cavity of the middle cerebral artery it contributes to the subcortical type of infarction, while the cortical part will not be affected during the blood supply. If collateral data are missing, a large infarction may develop in the portion supplied by the middle cerebral artery.
If a heart attack occurs in a part characterized by blood supply to the superficial branches of the middle type cerebral artery, then the development of deviation of the eyeballs in the direction of the affected part of the hemisphere cannot be excluded. If the dominant hemisphere is affected, then the development of the ipsilateral form of ideomotor apraxia begins. In addition, total aphasia can be observed. If the subdominant hemisphere was affected, then we are talking about anosognosia. In addition, the development of dysarthria or aprosody cannot be ruled out. A contralateral type of space neglect may also occur.
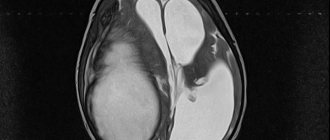
Diagnostics – accurate determination of the location and size of the lesion
Establishing a diagnosis and determining the exact location of the lesion and its size is one of the conditions for proper stroke treatment. The same point affects the course of the recovery period. In addition to the clinical picture and anamnesis data, instrumental research methods are also important for diagnosing stroke.
- Computed or magnetic resonance imaging. If a hemorrhagic stroke is suspected, it may be supplemented with contrast. This method allows you to clearly determine the location and size of the pathological focus, see the displacement of the midline structures of the brain, and also confirm or refute the presence of edema.
- Contrast angiography. In case of hemorrhagic stroke, this method allows one to determine the cause of vessel rupture; in case of ischemic stroke, the severity of vascular spasm and its specific area.
- Encephalography is mandatory for all patients who have fallen into a coma. The test accurately determines the vitality of the brain's cortex.
- Lumbar puncture. It is carried out if a hemorrhagic stroke is suspected not only for diagnostic, but also for therapeutic purposes. In case of hemorrhage in the brain, the cerebrospinal fluid contains an admixture of blood, which is determined not only laboratory, but also visually by its color.
Accurate diagnosis is extremely important - without determining the location of the lesion and its size, it is impossible to prescribe adequate therapy. In addition, these examination methods make it possible to observe the dynamics of changes occurring during treatment.
Infarction of the subdominant hemisphere
If an infarction of the subdominant hemisphere occurs, then the disease will be characterized by emotional disturbances and spatial non-response.
How much paresis will spread during a heart attack into the cavity of the blood supply (striatocapsular arteries) will depend on the location and area of the lesion itself (usually the upper part of the body: face, limbs or cotralateral part of the body). Speaking about an extensive infarction of the striatocapsular type, the main symptom is occlusion of the cerebral (middle) artery, which is expressed in aphasia or homonymous lateral hemianopia.
Forecast
How long a person will live after an ischemic attack depends on the location, size of the damage, time of initiation of treatment and concomitant diseases.
For reference. According to statistics, up to 25% of patients who have suffered a major ischemic stroke die within the first month. These are mainly those people whose attack occurred due to atherosclerosis or blood clot rupture.
The main cause of death in cerebral infarction is cerebral edema and its displacement. Sometimes exacerbation of cardiovascular diseases leads to death.
In the next 14-21 days of acute ischemic stroke, death occurs due to heart failure, the formation of a blood clot in the pulmonary artery, and pneumonia.
Survival rates for ischemic stroke are up to 70% at the end of the first 12 months. After 5 years, about 50% are still alive, after ten – a quarter. With a repeated attack, the prognosis worsens.
It is noted that the recovery of patients is best in the first three months, and the strength and movements of the leg muscles are normalized faster and better than in the arms.
For reference. The prognosis for complete paralysis is unfavorable. If recovery does not occur within a year, after this period normalization of the condition is unlikely. The exception is speech.
Doctors use several scales that allow them to assess the prospects for recovery.
NIHSS scale
The grading system is based on the manifestation of symptoms of the disease at the acute stage. The degree of consciousness, speech preservation, ability to control movements and their coordination, muscle strength, facial expressions, attention, eye movements, field of vision are analyzed. Moreover, if a person scores few points, the prognosis is satisfactory; if a person scores high, the prognosis is unfavorable.
For reference. If the patient scores up to 8-10 points on this scale, the probability of recovery is 70%, the observed disorders are characterized as mild. From 9 to 12 – medium; up to 15 – heavy; up to 33 – extremely severe. Indicator 34 characterizes coma. The probability of recovery for a patient who scores more than 20 points is no more than 16%.
Rankin scale
The Rankin scale is also often used. Based on various pathological symptoms, it describes the levels of the patient’s condition and the prognosis for the preservation of functions. A patient diagnosed with grade zero does not have any limitations or residual symptoms.
In the first degree, minor disturbances associated with speech, movements, and sensitivity are noted. The person remains able to work.
With the second, the patient loses some functions and cannot take care of himself fully.
With the third, a person walks independently with the help of a frame or a cane, but cannot fully take care of himself - cook, clean, go to the store. In some cases of left-sided lesions, a decrease in intellectual functions is observed.
The fourth characterizes patients who need help every day with dressing, moving, and eating.
With the fifth, the patient needs help and care constantly, he cannot be left alone.
Symptoms of lacunar infarction
If we talk about lacunar infarction, then clinically it is manifested by the development of lacunar syndromes, which is reflected in hemihypesthesia, hemiparesis, both individually and in combination.
Most often, a heart attack that occurs in the blood supply of the anterior cerebral artery manifests itself symptomatically in the form of movement disorders. With ongoing occlusion of the cortical branches, the development of motor deficits begins in the area of the feet or in the lower extremities. In addition, there is an implicit paresis of the upper extremities, which also manifests itself in severe damage to the tongue and face as a whole.
Types of strokes and their differences in duration and dynamics of development
It is necessary to promptly determine what exactly we are dealing with. This is important for prescribing appropriate treatment.
There are three main forms:
- microstroke;
- average;
- extensive.
Predicting recovery is influenced by factors such as:
- gender and age characteristics;
- medical history and general condition of the body;
- presence of concomitant diseases.
According to dynamics there are:
- progressive;
- completed.
Infarctions in the vertebrobasilar blood supply
The cause of infarctions that occur in the vertebrobasilar blood supply is the occlusion of the perforating branch of the artery, which is called the basilar. The main symptoms of such infarctions are lesions of the CN from the ipsilateral part. The process of occlusion of the vertebral type of artery, as well as branches, which are often called penetrating, that is, directed from the distal part, often contributes to the occurrence of lateral medullary syndrome, which in neurology is called Wallenberg syndrome.
How to recover after a stroke
Rehabilitation is an important aspect of treatment. It is aimed at protecting functioning areas of the brain from destruction and preventing a recurrent attack.
Physiotherapy
After an illness, you can recover with the help of physiotherapeutic treatment and a set of exercises. If speech is impaired after a stroke, then additionally you need to work with a speech therapist.
Physiotherapy includes:
- massage;
- acupuncture;
- reflexology
The main goal of the procedures is to restore motor activity and restore basic self-care skills. The duration of physiotherapeutic procedures and the frequency of their implementation are determined by the doctor.
Exercise therapy - rehabilitation after a stroke at home
Exercise therapy involves regularly performing exercises to relieve muscle tone. At first, patients are recommended to do passive exercises (with the help of loved ones), and then move on to more dynamic ones.
Passive exercises begin with large articular joints. This load is indicated for bedridden patients and those who have suffered paralysis.
The active load is performed in strict sequence:
- In a lying position . The patient needs to: bend his elbows, perform circular movements with his hands, clench and unclench his fingers.
- In a sitting position . They are done 1-1.5 months after surgery. The complex includes: sitting on a stool, circular movements of the head, bending, slow bending of the spine, raising the legs (right and left alternately).
- In a standing position . The purpose of the complex is to teach a person to walk. The complex includes: balance exercises, leg swings, squats, body tilts to the right and left.
Diet
The performance of the cardiovascular system depends on nutrition. During the rehabilitation period, you need to follow a diet to improve the metabolism in the body.
Basic diet rules:
- Avoid coffee and strong tea.
- Do not eat fatty and salty foods.
- Eliminate marinades, smoked foods and preserves from the diet.
- Minimize consumption of sweets and sugars.
- Introduce more berries, fruits and vegetables into your diet. After a stroke, cranberries and lingonberries are especially useful. Compotes, fruit drinks and jelly are made from the berries. Berries improve vascular permeability and prevent the development of atherosclerosis.
- Use unrefined sunflower oil.
- Eat small portions often.
During the rehabilitation period, it is important to eat a lot of red and green vegetables. They contain vitamins and microelements that increase the elasticity of blood vessels.
Diagnosis of ischemic stroke
Immediately before starting to collect anamnesis, doctors determine changes in cerebral circulation that have occurred since the onset of the disease. Experts determine the speed and level of progression of the onset of symptoms.
Ischemic stroke is characterized by a sudden onset of neurological symptoms. Important risk factors that you should pay attention to when diagnosing ischemic stroke are: atrial fibrillation, diabetes mellitus, atherosclerosis, arterial hypertension.
Diagnosis of ischemic stroke involves a physical examination, which is carried out according to accepted rules. When assessing the patient’s neurological status, attention should be paid to the presence of so-called cerebral symptoms:
- headache;
- generalized seizures;
- disturbance of consciousness.
In addition, patients may present with meningeal and neurological symptoms. If we talk about the types of laboratory tests, they are represented by urine and blood analysis (biochemical), coagulogram.
The main methods of instrumental diagnosis of ischemic stroke are CT and MRI, which also help to make a differential diagnosis, distinguishing ischemic stroke from various forms of intracranial damage or monitoring the dynamics of tissue changes during the treatment of this disease.
The most important ischemic symptom indicating damage in the area of the middle cerebral artery, which can be detected with CT diagnostics, is the weak expression of the lenticular nucleus and cortex, which subsequently leads to the development of cytotoxic edema.
In addition, during the course of an ischemic stroke, the doctor may detect changes associated with hyperdensity of the areas of the posterior or middle artery located on the affected side (for example, this could be thrombosis or embolism of the vessel).
During the first week of the disease, the area of gray matter with ischemic damage is characterized by an increase in the level of density, up to an isodense or slightly hyperdense state. The latter indicates the beginning of the development of the process of neovasogenesis or restoration of blood flow. Doctors also call this process the “fogging” effect, since at this time it is not always possible to determine the boundaries of ischemic damage, especially if the cerebral infarction has reached the subacute period.
MRI can accurately identify diffusion-weighted images of the affected area. Due to the resulting cytotoxic edema, water molecules usually move into the intracellular space (from the extracellular space), which leads to a slowdown in the rate of diffusion. All these changes that occur in the human body can be detected on the diffusion-weighted image obtained during MRI. It is this type of diagnosis that helps to identify the irreversibility of damage occurring in the structures of the brain.
Causes and factors for the development of a life-threatening condition
Risk factors for heart and vascular disease are similar in many ways. Conventionally, they can be divided into internal and external.
Internal factors are considered:
- diabetes;
- excess body weight;
- gender, since it was found that in men the disease occurs at a slightly earlier age than in women;
- age, since stroke is diagnosed more often in older people;
- heredity, manifested in the presence of hypertension, stroke, or a history of heart attack in close relatives.
External risk factors include:
- Climate and time of year. There is a direct dependence of ischemic stroke on the time of year and weather conditions. The most unfavorable periods are the winter and spring seasons, when there are often sudden changes in weather, large amounts of precipitation, and fluctuating atmospheric pressure and air temperature. It is at such moments that cerebral circulation disorders become more frequent.
- Smoking. An addiction doubles the risk of heart and vascular diseases. Due to the influence of nicotine and many other substances, the composition of the blood changes, blood pressure increases and the heart rate increases. The heart of a smoker makes more contractions than a non-smoker, which leads to premature wear of the heart muscle.
- Inactive lifestyle. Insufficient physical activity has a detrimental effect on human health, leading to obesity, the development of arterial hypertension, diabetes, multiple excess cholesterol levels, which contributes to the formation of cholesterol plaques and blood clots, increasing the risk of circulatory disorders in the brain.
- Regular alcohol consumption. Most often, strokes in young people occurred while they were intoxicated. Systematic consumption of alcohol in large quantities leads to cerebral hemorrhages and cerebral infarction.
- Emotional stress. Overstrain of the nervous system changes the biochemical composition of the blood, the level of electrolytes and leads to oxygen starvation of the vascular wall, which threatens subsequent changes.
Differential diagnosis
First of all, ischemic stroke should be distinguished from the hemorrhagic type of stroke. Neuroimaging techniques for studying the disease play a significant role in differential diagnosis. In some cases, it may be necessary to distinguish between ischemic stroke and acute hypertensive encephalopathy. Ischemic stroke should also be distinguished from toxic or metabolic types of encephalopathy, from brain tumors, abscesses, encephalitis and other brain lesions of an infectious nature.
Risk factors
The most common conditions affecting the development of stroke include the following:
- gender and age characteristics (men and women over 60-65 years old are at risk);
- high blood cholesterol;
- high blood pressure;
- bad habits: alcohol abuse, drug use, smoking and substance abuse;
- unhealthy diet (spicy, fatty foods, and high salt content);
- inactive lifestyle;
- overweight;
- heredity.
Leave a request for selection of a boarding house
for an elderly person with a stroke
Treatment of ischemic stroke
A person with even the slightest suspicion of an ischemic stroke should be hospitalized in a special department as quickly as possible. If the first symptoms of an ischemic stroke were detected no later than 6 hours from the onset of their manifestation, the patient is sent to the intensive care unit. Typically, the patient is transported in a reclining position, with the head raised to 30 degrees.
Hospitalization is not indicated for those patients who are in a state of terminal coma, suffer from oncology, or have a history of dementia with pronounced disability.
Treatment for ischemic stroke is usually:
- non-pharmacological (involves carrying out measures aimed at caring for the patient, as well as regulating the swallowing reflex, treating infectious diseases, which often manifest themselves in the form of pneumonia or genitourinary tract infections);
- medicinal (this type of therapy will be most effective only at the initial stage of the disease, in the first 6 hours from the onset of symptoms; medicinal treatment involves a multidisciplinary approach, which can be carried out within the walls of a special vascular department, usually located in the intensive care unit, where at any time you can perform a CT, MRI or ECG, as well as blood and urine tests.
Stages of development
In the process of developing an ischemic stroke, there are several stages. The first of them, acute, lasts up to 21 days from the onset of the attack. It can be divided into the most acute stage, lasting five days, when symptoms increase. This is the stage where most people die.
The second lasts up to six months. Reversible changes occur in cells during this period. Compensation for disturbances begins, blood circulation around the affected nuclei is restored. The stage is called the early recovery stage.
The third conditionally begins 6 months after the impact and lasts up to a year. During this period, cysts and glial formations form in the affected areas.
For reference. A year after the attack, the fourth stage begins. It is called the stage of residual manifestations. It lasts for the rest of a person’s life.
Maintaining body functions is the main stage of treatment
The main goal of any type of treatment for ischemic stroke is the correction of particularly important body functions and the mandatory maintenance of homeostasis. To achieve this goal, monitoring of all important physiological components is carried out, as well as measures aimed at maintaining hemodynamics, respiratory processes, and water and electrolyte balance. When treating a patient, one should also normalize his intracranial pressure in order to get rid of cerebral edema in the future. In addition, regular prevention of this disease and therapy aimed at combating the possible consequences of ischemic stroke should be carried out.
The main infusion solution during the treatment of this disease is sodium chloride solution. As for the use of glucose-containing solutions, in recent years doctors have abandoned them due to the possible development of hyperglycemia.
If an ischemic stroke develops against the background of diabetes mellitus, then the patient is given subcutaneous injections of insulin (short-acting). The exception is when specialists establish glycemic control while the patient is clearly conscious and does not suffer from impaired swallowing function.
In the first 2 days from the onset of the disease, doctors regularly measure the level of hemoglobin oxygen saturation in the blood. If the figure reaches 90-92%, then doctors administer oxygen therapy (usually starting with 2 liters per minute).
If the patient’s level of consciousness decreases to 8 points or less (calculated on the Glasgow scale), then this indicates an indicator for tracheal incubation. The decision whether to use mechanical ventilation in the future or not will be made based on the existing resuscitation provisions. If the patient's level of wakefulness is markedly reduced, there are clinical and other neuroimaging characteristics indicating cerebral edema (or increased intracranial pressure), then it will be necessary to maintain the head in an elevated state so that the neck does not flex. Coughing or signs of an incipient epileptic seizure should be minimized, as well as muscle excitation should be curbed. It should be remembered that infusions of hypoosmolal solutions are contraindicated.
Prognosis for future life after illness
The main factors that play a role in making a prognosis are the area and degree of brain damage, the age of the patient, the causes of stroke and the form of its course. The final outcome will also be affected by the timeliness of medical care and placement of the patient in a hospital, correct diagnosis of the disease, the presence or absence of concomitant diseases, complications, and the duration of rehabilitation.
- Restoring vital functions after a cerebral infarction can be difficult due to complications:
- Having suffered extensive hemispheric or brainstem infarctions, accompanied by paralysis, paresis, disorders of motor, swallowing and speech functions;
- Severe state of the general hemodynamics of the body in diseases of the cardiovascular system in the stage of decompensation;
- Damage to both vascular systems, which results in limited collateral circulation.
Recovery after a stroke can be much easier and faster if:
- The ischemic stroke suffered was localized to a small, discrete area;
- The patient's age is less than 30 years;
- The general condition of the heart and blood vessels is satisfactory;
- During the disease process, only one extracranial vessel was affected.
The prognosis is largely influenced by the following factors:
- The area and location of the necrosis focus. If it is located in the area of vital centers of the brain and affects a large number of tissues, the likelihood of an unfavorable outcome (even death) increases greatly.
- Patient's age. The older the person, the more severe the disease and the greater the likelihood of complications.
- The severity of neurological disorders. The more acute the stroke, the less likely it is to restore body functions.
- The cause of the disease. For example, when the cause of a cerebral infarction is atherosclerosis or a blood clot, the prognosis becomes less favorable.
- The development of all kinds of complications. High mortality is recorded due to damage to the respiratory and cardiovascular centers, cerebral edema, the transition of ischemic stroke to hemorrhagic, etc.
Forecasts are divided into favorable, average and unfavorable.
- Favorable prognosis. It is given if, after suffering a pathology, one or more body functions were slightly impaired. As a rule, after high-quality rehabilitation and compliance with all medical recommendations, a crisis period of the disease begins, after which the patient completely returns to normal life.
- Average forecast. The course of the disease was accompanied by gastrointestinal dysfunction, diabetes mellitus, pneumonia and other pathologies.
- Poor prognosis. It is given if a large area of brain tissue is affected.
Features of prognosis depending on the affected parts of the brain
The brain stem contains a huge number of nerve bundles, a thermoregulation center, respiratory and vestibular centers. If during a cerebral infarction one of the departments that plays an important role in life support was affected, then the likelihood of further normalization of its work is very low. That is why with necrotic lesions of the trunk it is often very difficult to make any predictions.
The cerebellum is anatomically located close to the brainstem and is responsible for the coordination of movements. If this department has been affected, a person ceases to feel his body, he loses balance and orientation in space. With timely assistance, cerebellar function can be restored during the rehabilitation period.
The cerebral cortex is responsible for fixing and transforming information received through the optic nerves. When the right hemisphere is damaged, the patient loses the ability to see what is located in the left part of his visual field and vice versa. Changes in this part of the brain also affect the perception of visual images in general, including familiar people and everyday objects. After ischemia, complete restoration of vision can take up to six months, and poor recognition of rarely seen objects can persist until the end of the patient’s life.
If several parts of the brain organ are affected at once, a cerebral coma may occur. This is the most severe type of stroke, which is accompanied by extensive necrosis of soft tissues. Coma is often accompanied by loss of the ability to breathe independently (regular shortness of breath) and complete disruption of the cardiovascular system. The risk of death after a coma is very high, and with a favorable outcome, the chance of restoring previous body functions is less than 15%.
Nutrition of patients with ischemic stroke
The main task of therapy for ischemic stroke is considered to be proper nutrition of the patient and control of water-electrolyte balance. This requirement must be implemented regardless of where the patient is being treated: be it in the intensive care unit or in the neurological department.
The main indicator for enteral tube feeding will be the progress of swallowing function. The amount of dose of administered nutrients is calculated based on data on the metabolic needs of the patient’s body, as well as its physiological losses. If food is administered orally (or using a tube), the patient should take a semi-sitting position.
To prevent deep vein thrombosis (in the case of ischemic stroke), the use of compression bandages or stockings is prescribed. This method also helps prevent the development of pulmonary embolism. In addition, direct anticoagulants can be used.
Who is guilty?
The main cause of ischemic stroke is a blood clot that has become mobile (thromboembolus). It could form directly in the heart: if it contracted arrhythmically or after a heart attack an aneurysm formed in it. But more often the blood clot could “fly off” from the veins of the lower extremities, especially if they were varicose.
Such blood clots can “travel” through the bloodstream. And if they are “carried” into the brain, then they block the artery that is slightly smaller than their own diameter.
Those vessels that are more likely to be damaged are:
- or too tortuous - then the blood flow speed in them is low;
- or they already have inflammation (vasculitis);
- or they have an atherosclerotic plaque.
The second reason is vascular atherosclerosis. An atherosclerotic plaque itself can cause ischemic stroke. This does not happen when it gradually increases in volume - causing the vessel to expand compensatoryly. This happens when the plaque crumbles, exposing the living cells of the vessel. In this case, they produce substances that attract platelets there. And when a blood clot “crawls” onto the plaque from above and blocks 90% of its lumen or more, a stroke develops.
The third reason is hypertension. When a person does not take any measures to combat it, his vessels undergo changes: their wall thickens, and accordingly, the lumen becomes narrower.
An increase in blood viscosity can also cause ischemic stroke. This happens when a person has blood diseases, there is a change in the amount of sex hormones, which is also observed with long-term use of oral contraceptives. There are cases when a stroke occurs due to dehydration (due to diarrhea, vomiting, high fever) - if a person does not try to return water to the body.
Spasm of cerebral vessels - when taking vasoconstrictor drugs, alcohol, nicotine, or migraines - can also cause a stroke. The most vulnerable vessels are usually affected.
Ischemic stroke occurs for another group of reasons. These are gas, fat embolisms, amniotic fluid embolism. The mechanism is the same as when a vessel is blocked by a blood clot that “flies off” from the venous system. Only here the blood flow in the vessel becomes impossible due to a fat drop, a large gas bubble or some volume of amniotic fluid, which, instead of pouring out, was absorbed into the bloodstream.
The rarest cause is a brain tumor that compresses nearby vessels, stopping blood flow through them.
All of these mechanisms lead to the fact that the part of the brain that was previously fed by the blocked artery begins to die. The larger the artery, the larger the area.
Neuroprotection
Speaking about the treatment of ischemic stroke, one should also mention a type of therapy such as neuroprotection. Its main focus is the use of special drugs that have neurotrophic and neuromodulatory functions. The most famous such drug today is Cerebrolysin (it belongs to the neurotrophic series of drugs). As is known, the central nervous system and spinal cord lack such an important property as storage. In other words, if you stop blood flow in these areas for 5 minutes, the neurons will begin to die. Therefore, the need to introduce neuroprotectors is mandatory. It should be carried out in the first minutes after the onset of an ischemic stroke.
Treatment of ischemic stroke will be successful with an integrated approach: basic therapy, rehabilitation, neuroprotection and reperfusion.
Complications
In ICD-10, the consequences of ischemic stroke are assigned code 169. If the diagnosis is incorrect and thrombolysis is performed during an attack, the course of the latter may worsen.
For reference. With right-sided and left-sided lesions, disturbances occur in the motor area. The limbs are paralyzed, muscle weakness develops, which does not allow the patient to care for himself or move around. Discoordination of movements, especially voluntary ones, is noted.
Sensitivity suffers, and it takes longer to restore it than to normalize motor activity.
Most patients experience consequences such as psycho-emotional disorders. Ischemic stroke is characterized by a tendency to depression, emotional lability, in many cases, aggressiveness, and the appearance of fears.
Impairments in the intellectual sphere with left-sided lesions lead to memory impairment, inability to analyze the situation, childishness, and disorientation in space and time. With right-sidedness, fantasy suffers.
Speech disorders are manifested by incoherent speech, repetition of the same phrases or words. In left-handed people they are observed with pathology of the right hemisphere.
In approximately 10% of cases, victims develop epilepsy. There is often a risk of a second strike.
Surgery
If we talk about the surgical type of treatment for ischemic stroke, then first of all, it includes surgical decompression, which implies a decrease in intracranial pressure and at the same time an increase in perfusion pressure against the background of preserved cerebral blood flow. According to statistics, the mortality rate from ischemic stroke has now been reduced to 30%.
The rehabilitation period after an ischemic stroke will be aimed at restoring previously lost motor and speech functions of the patient. This is the main task of neurologists who perform electromyostimulation, exercise therapy, regular massage of paretic limbs or mechanotherapy. To correct the patient’s speech, he is also referred to a speech therapist.
Rehabilitation
Not everyone knows what to do after an ischemic stroke. During the recovery period, the first three months after the disease are most important. Rehabilitation must be comprehensive. This may include:
- restoration of musculoskeletal functions;
- restoration of speech and swallowing functions;
- proper diet that meets the requirements;
- regular blood pressure monitoring and drug therapy;
- symptomatic treatment;
- returning control to the pelvic organs;
- treatment of depression with the help of an experienced psychologist.
Massage, manual therapy and passive exercises
These auxiliary measures are aimed primarily at restoring the musculoskeletal system and the functioning of internal organs. Regular sessions will help relieve headaches, dizziness and problems with the gastrointestinal tract.
Therapeutic exercises
Therapeutic exercise is effective in the rehabilitation of sick and disabled people, as well as in preventing the recurrence of the disease. Exercises are carried out under the supervision of the attending physician.
Physiotherapy
Physiotherapy involves the therapeutic use of various physical means: movement, heat, fluids, etc. The method has a gentle effect on the body, stimulating recovery processes. Thanks to a combination of techniques, tight muscles are relaxed, vertebral mobility is restored and the condition of the intervertebral discs is normalized.
Prevention
To avoid recurrent strokes, you should lead a healthy lifestyle and limit fatty and fried foods in your diet. For prevention purposes, it is recommended to use antiarrhythmic drugs, and to prevent the formation of blood clots, the use of anticoagulants is prescribed. Only the attending physician can prescribe medications; self-medication in this case is unacceptable.
Prevention will help reduce the risk of disease to a minimum.
It is better to know everything about ischemic stroke in advance in order to avoid it. It is also important to study the symptoms of ischemic stroke well in order to begin treatment on time.
Prognosis for ischemic stroke
The prognosis in the case of ischemic stroke will be determined by the location and area of brain damage. In addition, important indicators here will be the patient’s age and the severity of concurrent diseases. The most difficult period for ischemic stroke is the first 5 days. It is at this time that there is an increase in cerebral edema in the area of its damage, after which a time of stabilization begins, when the impaired functions of the central nervous system gradually return to normal. To date, the percentage of deaths in patients with ischemic stroke is no more than 20%.
Survival Statistics
Cerebral infarction ranks third in mortality in the world (after heart disease and malignant tumors). According to research, 12-25% of patients die in the first weeks of the disease. The main cause of death is cerebral edema. In second and third place are pneumonia, pulmonary artery blockage, followed by blood poisoning, respiratory tract dysfunction and kidney failure.
About 40% of deaths occurring in the first three days are associated with extensive necrosis of brain tissue. Among patients who survive the disease, about 70% become incapacitated and disabled due to neurological disorders. Over time, these disorders fade away, due to which six months after rehabilitation the disorders remain in 40% of patients, and after a year – in 25%.
Prevention of ischemic stroke
The most important thing in the prevention of ischemic stroke is considered to be measures to prevent thrombosis of blood vessels, which is formed when cholesterol plaques appear in the blood. For this purpose, doctors prescribe a set of procedures to maintain a healthy lifestyle, eliminating smoking, alcohol and fatty foods. As is known, those at risk of developing ischemic stroke are primarily those patients who suffer from chronic diseases of the cardiovascular system, diabetes mellitus or arterial hypertension.
Secondary prevention of ischemic stroke includes the implementation of a comprehensive program in the form of: antihypertensive therapy with the use of inhibitors, diuretics; lipid-lowering therapy with statins; surgical intervention (carotid endatherectomy is performed); antithrombotic therapy (antiplatelet agents and indirect anticoagulants).
Causes
The “trigger” for an ischemic stroke is the cessation of blood flow to one or more areas of the brain. It is a consequence of impaired vascular patency or disruptions in the general hemodynamics of the body. Preceding factors include:
- coronary heart disease;
- diabetes;
- migraines in the temporal, parietal and occipital areas of the head;
- heart disease;
- hormonal contraception;
- excessive consumption of fatty foods,
- bad habits;
- increased blood viscosity;
- heredity.
The combination of two or more factors increases the risk of ischemic stroke.
8 out of 10 people who have suffered an ischemic stroke remain disabled for life.
Literature
- Edward C Jauch, MD, MS, FAHA, FACEP. Ischemic Stroke, 2018
- Jennifer Berry. Ischemic stroke: Causes, symptoms, and risk factors, 2017
- Seunggu Han, MD. Understanding complementary and alternative treatments for stroke, 2018
- Oluwayomi Aoko. What are major Factors in Stroke Recovery and Future Directions of Therapy., 2015
- Ministry of Health of the Russian Federation. Principles of diagnosis and treatment of patients with acute cerebrovascular accidents, 2000.
- Denisov I. N., Kandyba D. V., Kuznetsova O. Yu. Diagnosis and tactics for stroke in general medical practice, including primary and secondary prevention
Why does a stroke occur?
Ischemic stroke (ischemia is a decrease in blood flow) develops due to blockage of a vessel that supplies blood to an area of the brain. Most often, the vessel is blocked by a blood clot that formed locally or was brought by the blood flow from another organ. A thrombus is a blood clot, the formation of which the coagulation system responds to damage to the vascular wall. In order for a blood clot to occur, there must be prerequisites - atherosclerosis, diabetes mellitus, varicose veins, hypertension or other conditions in which the inner wall of the vessel is damaged. Massive thrombus formation begins only on the vessel wall, which has lost its smoothness, is pitted and ulcerated. Most often, blood clots form in the cerebral arteries, namely the middle cerebral artery, and in the vessels and cavities of the heart. Not only a blood clot can come off, but also a piece of atherosclerotic plaque (microembolism). A blood clot never forms in a healthy vessel.
At CELT you can get advice from a neurologist.
- Initial consultation – 3,200
- Repeated consultation – 2,000
Make an appointment
Types of cerebral stroke and its consequences
It causes extensive changes that depend on the severity of the attack. The most common:
| with hemorrhagic | with ischemic | with spinal |
|
|
|