Pancreatic necrosis is one of the most severe diseases of the abdominal organs and in 1% of situations causes an acute abdomen. Pancreatic necrosis is more often (in 70% of cases) diagnosed in young people and can be either a separate nosological entity or act as a complication of acute pancreatitis.
The chances of surviving after destruction (destruction) of the pancreas are small and amount to 30–60% even with adequate and timely treatment, and in the case of total pancreatic necrosis they are zero. In recent years, there has been an increase in the incidence of the disease, which is 6–9%. Pancreatic necrosis is equally often diagnosed in both men and women.
General information
Pancreatic necrosis (necrosis of the pancreas) is a destructive disease of the pancreas, which is a serious complication of acute or chronic pancreatitis .
The ICD-10 code for pancreatic necrosis is K86.8.1. A characteristic feature of this formidable disease is the gradual necrosis of pancreatic tissue. This is a very dangerous diagnosis that poses a threat to human life. The death of this organ occurs due to the fact that the pancreatic tissue is dissolved by the enzymes that it itself produces. As a rule, this process is combined with other pathological phenomena - inflammatory processes, infection, etc.
This disease is the most severe complication of pancreatitis. As a rule, it affects young people of working age. According to medical statistics, this disease accounts for about 1% of all recorded cases of acute abdomen. However, the number of cases of this disease has been increasing recently. The high mortality rate with pancreatic necrosis is also alarming - it is 30-80%. Therefore, it is extremely important to diagnose the disease in a timely manner and begin adequate treatment immediately.
What is pancreatitis?
Pancreatitis is inflammation of the pancreas. The main causes [Official source] of the disease are considered to be excessive alcohol consumption and frequent consumption of fried, fatty foods. Adults are more susceptible to this pathology than children. It develops due to a violation of the outflow of pancreatic secretions.
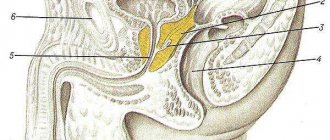
Pancreas
is one of the organs of the human digestive system that secretes enzymes for digesting food and hormones (insulin, glucagon) that regulate the metabolism of carbohydrates.
The waste products of the pancreas (juice and enzymes in it) enter the duodenum and participate in the process of digesting incoming food. However, during pancreatitis, all produced pancreatic juice is not removed from the gland, remaining inside the organ and destroying pancreatic tissue.
Pancreatitis comes in two types: chronic and acute. Each of them has its own causes, symptoms and treatment methods.
Pathogenesis
The basis of the pathogenesis of pancreatic necrosis is a failure in the mechanism of internal protection of the pancreas from the influence of pancreatic enzymes that destroy it. If a person drinks alcohol heavily and constantly overeats, external secretion increases significantly, the ducts of the gland are stretched, and the outflow of pancreatic juices is disrupted.
Necrosis of the pancreas develops against the background of pancreatitis - an inflammatory process of the pancreas, in which the death of part or the entire organ often occurs.
The pancreas is an organ important for the normal functioning of the body. Its main functions are the production of the main enzymes involved in digestion, as well as the regulation of blood sugar due to the production of the hormones insulin and glucagon . Accordingly, dysfunction of this organ leads to serious disturbances in the general condition of the body.
When a person feels hungry, juices and enzymes are transported through the connecting duct into the small intestine, which ensures enzymatic processing of food. Pancreatic fluid acts on the acidic environment of gastric juice, neutralizing it. In the intestines, digestive enzymes break down and process substances.
The pancreas produces the main digestive enzymes:
- lipase – breaks down fats;
- amylase – converts starch into sugar;
- chymotrypsin , trypsin - are involved in the breakdown of proteins;
- glucagon , insulin , polypeptide , etc.
If in healthy people the enzymes produced by the pancreas are active directly in the digestive tract, then in patients with damage to the ducts of the gland, the enzymes directly affect the pancreas. Against the background of increased pressure inside the ducts, edema of the parenchyma develops, the acini of the pancreas are destroyed, and proteolytic enzymes are activated prematurely. As a result, the gland “poisons” itself. Due to the activation of lipase, necrosis of fat cells occurs, under the influence of elastase, blood vessels are destroyed, and activated enzymes, as well as breakdown products, end up in the bloodstream. In this case, there is a toxic effect on all tissues and organs. First of all, damage occurs to the liver, kidneys, heart, and brain.
With pancreatic necrosis, three stages of tissue death are determined:
- Toxemic - toxins of bacterial origin appear in the blood, the gland actively produces enzymes.
- Development of an abscess - a purulent inflammatory process of tissues and organs that surround the pancreas develops.
- Purulent changes in tissues - if purulent sepsis develops, immediate surgical intervention is required, as this condition is life-threatening.
General information about the disease
Pancreatic necrosis is a complication of acute pancreatitis (inflammation of the pancreas), consisting in varying degrees of death of cells in this organ and the development of severe clinical symptoms.
Pancreatic necrosis is not a disease of alcoholics! As a rule, with chronic alcohol consumption, chronic pancreatitis develops with a gradual loss of exocrine pancreatic function. Pancreatic necrosis, most often, occurs with occasional intake of large volumes of ethanol-containing drinks and animal fats.
Etiology
- Consumption of significant amounts of alcohol and fatty foods (more than 95% of all pancreatic necrosis).
- Gallstone disease, decompensation of biliary dyskinesia.
- Acute surgical pathology of another organ (penetration due to gastric ulcer, etc.)
- Acute poisoning by chemicals.
- Traumatic injury to the pancreas.
- Congenital malformations of the pancreas.
- Shock (septic, hemorrhagic, traumatic - a condition leading to multiple organ failure).
- History of surgical interventions (adhesive disease).
- Iatrogenic pancreatic necrosis (a rare phenomenon when acute pancreatitis and pancreatic necrosis develop after endoscopic examination of the gland).
Pathogenesis
A significant intake of ethyl alcohol and animal fats into the digestive tract leads to hyperfunction of the pancreas. If a person has problems with the outflow of pancreatic juice from the gland, a huge number of highly active pancreatic enzymes (phospholipase, trypsin, chymotrypsin, elastase and others) are suddenly activated.
First, trypsinogen is released from damaged cells, transforming into trypsin, and kallikrein and kallidin are activated. When exposed to these enzymes, histamine and serotoxin are released, which activate blood protein factors (Hageman and plasminogen).
Due to damage to the microvasculature of the pancreas, all enzymes penetrate into the general bloodstream and cause general vascular spasm (for a short period), after which dilatation (expansion) of blood vessels occurs, the permeability of the vascular walls increases, blood plasma freely leaves the vascular bed, and edema develops pancreas (at this stage, internal bleeding often occurs in the retroperitoneal space). As in any organ system, a slowdown in blood flow (stasis) leads to the formation of blood clots - thrombi.
Vascular thrombosis leads to dysmetabolic disorders in cells (hypoxia, acidosis), and areas of necrosis form in the pancreatic parenchyma. Lipases (enzymes that break down fat molecules) are released from dying cells. A large number of lipases can provoke necrosis not only in the pancreas, but also in the omentum, fatty tissue of the retroperitoneal space, etc.
In addition to local damage, general intoxication develops due to the effect of pancreas enzymes on systemic vessels. Inadequate vascular tone leads to circulatory disorders in other organs, cellular and organ degeneration, acid-base, water-electrolyte disorders develop, protein synthesis, carbohydrate and fat metabolism slow down. Without pathogenetic correction with pharmacological drugs, multiple organ failure develops
An important link in the development and severity of pancreatic necrosis are protease inhibitors - special blood proteins that protect against the effects of one’s own and foreign proteolytic enzymes (including the pancreas) on cellular metabolism. The greater the concentration of protease inhibitors and their binding capacity, the less pronounced the development of pancreatic necrosis will be. This function is individual for each organism and is determined genetically, which is why the clinical picture of pancreatitis is so varied.
Classification
According to the prevalence of necrosis:
- focal - necrosis of one anatomical area of the pancreas: head, body, tail or parts thereof;
- diffuse (segmental) - all parts of the pancreas are affected (not only the parenchyma, but also the vessels, ducts, and nerves).
According to the depth of the lesion:
- superficial - necrosis of the outer layers of the gland. Usually ruptures when the superficial pancreatic ducts rupture, when juices containing proteolytic enzymes accumulate between the outer surface of the pancreas and its capsule;
- deep - necrosis of more than half of the pancreas, part of the tissue remains viable;
- total - death of the entire organ. Often the process moves to the omentum and retroperitoneal fatty tissue.
According to the nature of the clinical course:
- abortive course - a moderate form of pancreatic necrosis. Tissue (interstitial) edema develops around the foci of necrosis. Compensatory inhibitory systems cope with the amount of vasoactive enzymes released from the gland, spontaneous recovery occurs (subject to drug treatment);
- progressive course - the concentration of vasoactive enzymes in the blood exceeds the compensatory abilities of the body. Deep or total necrosis of the gland develops, hemodynamic disturbances, multiple organ failure, there is a high probability of sudden pancreatogenic shock, spontaneous internal bleeding and further infection of the pancreas;
- regressive course - the clinical symptoms of pancreatic necrosis gradually “fade away” within 20 - 30 days. Against the background of pancreatic edema, pseudocysts (connective tissue capsules with pancreatic fluid) form. Sometimes pseudocysts reach significant sizes, which leads to displacement of the stomach, gall bladder, and liver with disruption of their functions;
- relapsing course - typical for people suffering from alcoholism. A special clinical form that develops against the background of chronic dystrophic changes in the pancreas with periods of sudden exacerbation. Relapses in this case are repeated several times during a lifetime and become more and more severe, often leading to death;
- fulminant pancreatic necrosis is the most dangerous form. Necrosis of the gland and the clinical picture develop over several hours. Hemodynamic disturbances, multiple organ failure and shock develop rapidly. Mortality rate is about 90%.
According to the mechanism of occurrence:
- hypersecretory is the most common form. It is formed against the background of excessive release of pancreatic enzymes due to consumption of alcohol and fatty foods;
- traumatic - develops against the background of blunt abdominal trauma, surgical interventions, diagnostic procedures;
- biliary - against the background of a violation of the outflow of bile from the liver (cysts, tumors, developmental abnormalities). With this option, pancreatic necrosis is often complicated by the addition of a bacterial infection and the development of phlegmon of the fatty tissue of the retroperitoneal space;
- mechanical - due to obstruction of the common bile duct and disruption of the flow of bile into the duodenum, the pancreas begins to produce an increased amount of pancreatic juice, which destroys it;
- immune - autoimmune inflammation of the pancreas (destruction of pancreas cells by its own lymphocytes) gradually leads to its death;
- contact - develops against the background of a complicated peptic ulcer of the stomach or duodenum (penetration of the ulcer);
- vascular - this form is typical for people suffering from atherosclerosis and other vascular diseases (usually the elderly). Gradual vascular stenosis leads to blood stasis and the development of dysmetabolic disorders in the pancreas.
According to clinical form:
- hemorrhagic pancreatic necrosis - large-focal or total necrosis of the pancreas. It develops extremely quickly and is accompanied by a pronounced clinical picture (multiple organ failure). High lethality;
- fatty pancreatic necrosis - the formation of foci of necrosis that merge with each other, a connective tissue capsule is formed around it. Without drug therapy, it becomes hemorrhagic;
- mixed pancreatic necrosis.
According to the presence of complications:
- uncomplicated;
- complicated (infection, bleeding, shock, etc.).
According to severity:
- mild degree - isolated foci of necrosis in the gland;
- medium degree - large foci of necrosis without fusion;
- severe degree - total necrosis of the pancreas;
- extremely severe degree - complicated total necrosis.
Classification
Depending on the predominance of damaging mechanisms, three forms of the disease are determined:
- Adipose – with increased lipase activity, pancreatic adipose tissue is destroyed. After lipase appears outside the pancreatic capsule, it acts, provoking the appearance of areas of necrosis in the layers of the peritoneum, the greater and lesser omentum, the mesentery, and internal organs. aseptic peritonitis and multiple organ failure subsequently develop .
- Hemorrhagic - with increased elastase activity, microcirculatory disorders predominantly develop, resulting in vasospasm . For a short time - several days, and sometimes hours - toxemia provokes paresis of the vascular wall, vasodilation, and blood flow in the gland tissues slows down. This leads to a sharp increase in the likelihood of blood clots and, later, ischemic necrosis . Initially, the vascular wall is destroyed thicker than the pancreas, and later in other organs. The consequence of all these processes is hemorrhage into the retroperitoneal tissue and internal organs. The main symptom that characterizes hemorrhagic pancreatic necrosis is effusion into the abdominal cavity with the presence of blood in it. The disease develops rapidly, so in doctors’ reports you can often see the conclusion: “The cause of death is hemorrhagic pancreatic necrosis.”
- Mixed - with approximately the same activity of elastase and lipase, the signs of fat necrosis and hemorrhagic imbibition are equally pronounced.
Depending on the prevalence of pathological manifestations, two forms are defined:
- local (one area affected);
- diffuse (two or more areas are affected).
Depending on the rate of progression:
- progressive;
- sluggish.
Depending on the depth of the lesion:
- surface;
- deep;
- total.
Depending on the course of the disease:
- recurrent;
- progressive;
- retrogressive;
- fulminant;
- abortive.
Depending on the severity of the manifestations of the disease, several of its degrees are determined:
- Mild degree - as a rule, this is edematous or diffuse necrosis with small foci.
- Medium degree - diffuse or local with more pronounced foci.
- Severe degree - diffuse or total with large foci.
- An extremely severe stage - pancreatic necrosis is accompanied by complications leading to irreversible consequences and death.
Correction of necrotic changes
At the first signs of pancreatic necrosis, the patient is hospitalized. Due to the high risk of death, treatment is carried out in the intensive care unit. Treatment is selected by several specialists at once:
- gastroenterologist;
- endocrinologist;
- surgeon;
- resuscitator.
Therapy begins with ensuring complete rest for the pancreas. Strict bed rest is prescribed, the consumption of any food is completely excluded (life functions are supported parenterally). If there is no vomiting, remove remaining food from the stomach by lavage. To reduce reflex irritation of the gland, the stomach can be washed several times with cool sterile solutions.
At the initial stages, conservative treatment is carried out. It implies the purpose:
- painkillers (including narcotic analgesics);
- anti-inflammatory;
- suppressing the secretion and activity of enzymes;
- antishock therapy;
- diuretics (to relieve swelling of pancreatic tissue);
- broad-spectrum antibiotics (for stopping and preventing the spread of purulent-necrotic processes);
- detoxification measures (large amounts of infusion solutions);
- hemosorption (hardware purification of blood in case of severe intoxication);
- correction of identified violations in the functioning of organs.
In severe cases and pronounced areas of necrosis of the gland, the patient immediately undergoes surgical treatment. If the localization of necrosis is difficult to identify, the operation is performed on days 4-5. The difficulty of surgical treatment lies in the increased risk of infectious complications. During the operation the following is carried out:
- laparoscopic examination of the gland ducts;
- removing the cause of congestion;
- excision of areas of necrosis;
- removal of exudate;
- installation of drainage devices.
Inpatient treatment lasts up to 2 months. After discharge, the patient must remain in bed for another 2 weeks. Afterwards, short walks are allowed. An important aspect of recovery is diet. The diet consists exclusively of boiled and steamed dishes of homogeneous consistency. You can eat chicken, turkey, and low-fat fish. The diet is based on cereal dishes, protein omelettes, and boiled vegetables. Any secretion stimulants (fatty, fried foods, mushrooms, industrial products, raw vegetables and fruits) are excluded from the menu. All food should be eaten warm.
Causes
A number of factors that provoke necrotic processes in pancreatic tissues are determined:
- regular excessive consumption of alcohol;
- constant overeating, abuse of smoked, fried and fatty foods;
- peptic ulcer;
- gallstones;
- the presence of abdominal injuries and previous surgical interventions in this area;
- severe infectious diseases.
Under the influence of these factors, pancreatic dysfunction can develop, which leads to pancreatitis and pancreatic necrosis. But, as a rule, pancreatic necrosis manifests itself against the background of occasional alcohol intake. Studies have confirmed that in most cases, pancreatic necrosis developed after an episode of drinking alcohol in very large quantities.
Etiology
- Consumption of significant amounts of alcohol and fatty foods (more than 95% of all pancreatic necrosis).
- Gallstone disease, decompensation of biliary dyskinesia. Acute surgical pathology of another organ (penetration due to gastric ulcer, etc.)
- Acute poisoning by chemicals.
- Traumatic injury to the pancreas.
- Congenital malformations of the pancreas.
- Shock (septic, hemorrhagic, traumatic - a condition leading to multiple organ failure).
- History of surgical interventions (adhesive disease).
- Iatrogenic pancreatic necrosis (a rare phenomenon when acute pancreatitis and pancreatic necrosis develop after endoscopic examination of the gland).
Symptoms of pancreatic necrosis
Signs of this disease may appear several hours or days after the influence of factors provoking the disease has been noted.
The main symptom is pain manifested in the left hypochondrium. Also, pain can radiate to the sides, back, and be felt in the pit of the stomach. The pain is constant, quite intense or moderate. It can be encircling, radiating to the shoulder, scapula, so a person may have the impression that a heart attack . The pain becomes stronger after the patient eats. This may cause nausea and repeated vomiting. Pancreatic necrosis without pain is impossible.
The following symptoms of pancreatic necrosis are also likely:
- redness of the skin, as due to damage to the pancreas substances that dilate blood vessels enter the blood;
- flatulence is a consequence of rotting and fermentation in the intestines;
- bluish or purple spots on the abdomen, buttocks and sides - the so-called Gray-Turner symptom ;
- gastrointestinal bleeding is a consequence of the destructive effect of enzymes on the walls of blood vessels;
- temperature increase;
- tension of the anterior abdominal wall, pain on palpation;
- dry mucous membranes, skin, thirst are a consequence of dehydration;
- decreased blood pressure ;
- confusion, delirium.
The disease, as a rule, begins acutely, and most often patients associate its first signs with excessive alcohol consumption and a significant violation of the diet. Doctors testify that most of these patients are admitted to hospitals while still intoxicated, which confirms the rapid development of pathological changes in the gland. There is a direct relationship between the severity of pain and the severity of necrosis. If destructive changes spread to the nerve endings, this leads to a gradual decrease in the severity of pain. But this sign, combined with intoxication, is quite alarming in terms of prognosis.
After pain appears, after some time the patient begins to experience vomiting. She is difficult to tame and does not bring relief. The vomit contains blood clots and bile. Due to constant vomiting, dehydration develops, which leads to dry skin and a coated tongue. Diuresis gradually slows down. Flatulence, stool and gas retention are noted. These symptoms are accompanied by fever .
Due to fluctuations in glucose levels, toxemia and hyperfermentemia, the brain is affected and encephalopathy .
If the inflammatory process progresses, the pancreas increases significantly in size. An infiltrate forms in the abdominal cavity. This condition is life-threatening for the patient.
Signs of intoxication
Bacterial toxins (bacteria themselves may not be present in the blood) circulating in the bloodstream cause intoxication of the body. The temperature rises (up to 38 and above), general weakness occurs, the heartbeat and breathing become more frequent, shortness of breath appears, and blood pressure decreases. The effect of toxins on the brain leads to encephalopathy. The patient's consciousness is confused, the patient is excited or inhibited, disoriented. With severe toxemia, coma may develop.
Hyperemia or pale skin
During the toxemia phase, the pancreas releases vasoactive substances into the blood (dilate blood vessels), which is manifested by redness of the skin. Later, as intoxication develops, the skin turns pale, becomes sallow, marbled or icteric and becomes cold to the touch. Blue-violet spots appear on the sides of the abdomen, on the back, buttocks and in the navel area as a result of internal hematomas and hemorrhages into the soft tissues. Subcutaneous hemorrhages are not observed in all cases of pancreatic necrosis.
Internal bleeding
An increase in the level of elastase contributes to the destruction of blood vessels and the formation of hemorrhagic effusion in the abdominal, pleural and pericardial cavities.
Tests and diagnostics
If you suspect the development of necrosis, you should immediately consult a general practitioner. The specialist conducts an examination and determines the circumstances surrounding the development of the disease. He must palpate and determine the presence, nature and location of pain. If a pathology of the gland is suspected, the patient is examined by an endocrinologist. If tumors are detected on the gland, an oncologist is also involved in the treatment process.
To establish a diagnosis, instrumental and laboratory examinations are prescribed.
Laboratory studies include an extensive blood test, since with necrosis the following pathological changes are noted:
- Increased sugar levels, increased granularity of leukocytes , neutrophils.
- Increased ESR .
- Increased levels of elastase, trypsin, hematocrit as a result of dehydration.
- Increased liver enzymes due to inflammation.
- The development of necrosis is also indicated by an increased level of amylase in the urine.
- In the process of laboratory tests, the state of hormones and digestive enzymes is determined.
Also during the diagnostic process, the following studies may be prescribed:
- Ultrasound examination - to determine the uneven structure of gland tissue, identify cysts, abscesses, fluid in the abdominal cavity, stones in the bile ducts. Ultrasound also makes it possible to analyze the condition of the ducts.
- Magnetic resonance imaging, computed tomography - allow you to determine the foci of disease development, the size of the organ, and also find out whether inflammation is developing, whether there are swelling, abscesses, neoplasms, deformities.
- Angiography of gland vessels.
- Diagnostic laparoscopy.
- Puncture.
A specialist will be able to make a final diagnosis only after receiving data from all prescribed studies.
Clinical picture
The disease is characterized by bright and rapidly increasing symptoms. Here are the most expressive ones:
- Pain syndrome of a sudden and encircling nature, appearing in the left hypochondrium and radiating to the shoulder, under the shoulder blades, to the heart area after a heavy feast. The pain is so intense that it can cause shock. It is slightly reduced in a position in which the knees are pressed to the stomach.
- Frequently repeated and dehydrating vomiting, which can injure blood vessels, resulting in the release of bloody impurities.
- Bloating, flatulence.
In addition to these signs, the following manifestations are possible:
- yellowness of the skin, characteristic of hepatitis (lack of treatment for acute pancreatitis provokes liver failure and degeneration of its tissues);
- increased heart rate;
- dyspnea;
- problems with urination caused by kidney dysfunction;
- deviations in the functioning of the nervous system, accompanied by inappropriate behavior and even in many cases (about 30%) a coma.
The symptoms, for all their expressiveness, are not characteristic exclusively of destructive pancreatitis, therefore, to make an accurate diagnosis, a thorough examination of the patient is carried out.
Treatment with folk remedies
When a patient's pancreatic necrosis worsens, he experiences severe pain. Folk remedies that are used in parallel with the main treatment can help improve the condition a little. But, before practicing such methods, it is necessary to visit a doctor, establish a diagnosis and begin practicing the correct treatment regimen.
- The fruits of Japanese Sophora - a decoction is prepared from them. A spoonful of raw materials should be filled with 1 tbsp. boiling water and leave for 5 hours. Drink warm before every meal. The course of treatment is 10 days.
- Blueberry berries and leaves - a decoction is prepared from them by pouring boiling water over dried or fresh raw materials and boiling for 5 minutes. (2 tbsp. raw materials per 250 ml of water). Drink instead of tea.
- Immortelle herb - a decoction helps relieve pain and inflammation. To prepare the decoction, take 1 tbsp. l. dry herbs and a glass of water, cook for 5 minutes. Strain the resulting broth and drink throughout the day.
- Oat decoction helps relieve irritation and restore organ cells. To prepare the product, you need to soak the grains and wait a few days for them to sprout. Sprouted grains need to be dried and ground. Pour the mixture with cold water (1 tablespoon of oats per 1 glass of water) and leave for about half an hour. You need to drink 2 glasses of this product a day.
- Lemon – helps reduce pain. To do this, boil the lemon in water for 5 minutes, then squeeze the juice out of it and mix with raw yolk. Drink the product on an empty stomach and do not eat for three hours after it. Take it five times a day, once every three days. The course of treatment lasts several months.
- Licorice root - to prepare it you need to take 1 tbsp. l. chopped dry licorice root, the same amount of dandelion and burdock leaves. Pour the mixture with 2 cups of boiling water, drink the infusion hot, half a glass 3-4 times a day.
There are also special herbal mixtures used to treat the pancreas. But it is important to take into account that they bring benefits to the body if such preparations are taken regularly and according to the scheme approved by the doctor. Under no circumstances should you practice self-medication with folk remedies for such a terrible diagnosis as pancreatic necrosis.
Which famous people died from pancreatic necrosis?
The root of all diseases of the gastrointestinal tract lies in people’s careless attitude towards their diet . A person does not care about taking food on time, eats fast food, eats on the run, or, conversely, goes hungry most of the day.
Reference! Often, this attitude towards food culture is caused by too fast a pace of life: there is no time to leisurely have breakfast, prepare first courses, or go shopping in search of healthy foods.
Many famous, public people suffer from chronic abdominal pain . Due to their busy work schedule, they cannot find time for a full medical examination. The consequences of this are quite sad.
American musician David Alexander, who was at the peak of his popularity in the 1970s. g., died at the age of 27 years from pulmonary edema. An attack of acute pancreatitis brought him to a hospital bed. For the same reason, the German composer Paul Hindemith passed away. Acute pancreatitis also led to the death of the Swedish writer Per Fredrik Wahl. 28-year-old Russian world boxing champion Elena Sabitova died of pancreatic necrosis.
Which artist died from pancreatic necrosis? Russian actor Vladislav Galkin was hospitalized in a Moscow clinic with an attack of pancreatitis . When heart failure added to the disease, he died.
Popular American actor Patrick Swayze died at the age of 57 from pancreatic cancer.
Who survived after severe pancreatic necrosis? Russian showman Valdis Pelsh at the age of 40 almost died due to an attack of acute pancreatitis . He spent some time in intensive care. Doctors managed to stabilize his condition without surgery.
As can be seen from the statistics, problems with the pancreas occur in young people no less often than in older people. And the high mortality rate indicates that the disease develops rapidly, and in just a year or two the organ may lose the ability to function normally. This means that the issue of proper nutrition remains relevant for people of all ages .
A healthy lifestyle is the only preventative measure for gastrointestinal diseases. Completely giving up alcohol and switching to simpler and healthier foods will reduce the load on the digestive organs and improve the health of the body.
It is recommended to undergo preventive examinations to identify diseases at an early stage. For example, an ultrasound of the pancreas can reveal diffuse focal changes in its structure. These changes in themselves are not considered an independent diagnosis, but serve as a reason for further examination.
Prevention
To prevent pancreatic necrosis, you need to follow some simple recommendations:
- Limit the amount and frequency of alcohol consumption.
- Avoid junk food – fast food, processed foods, soda, and minimize the consumption of fatty and fried foods.
- Do not take medications without a doctor’s prescription, especially do not abuse them.
- Try to create a diet based on natural products, try to practice split meals in small portions.
- Treat cholelithiasis in a timely manner.
- At the first symptoms indicating problems with the pancreas, consult a doctor immediately.
- Follow the principles of a healthy lifestyle.
First aid
If symptoms of a pathological condition appear, it is necessary to call emergency doctors, since therapy for pancreatic necrosis should be carried out in a hospital setting. Before doctors arrive, it is necessary to measure the patient’s temperature and blood pressure. A heating pad with cold water should be applied to the area of the right hypochondrium. The person must be ensured complete rest, as sudden movements can worsen the condition. You need to open the windows to allow air flow.
The patient should breathe shallowly without taking sharp breaths. This will reduce the intensity of pain. It is advisable to perform a gastric lavage and an enema to free the rectum from feces. The patient should completely refuse food. Water can be consumed in small portions not exceeding 50 ml. To reduce the intensity of pain, you can use No-shpu, Papaverine and Drotaverine. It is better not to use other medications until doctors arrive.
Diet for pancreatic necrosis
Diet for pancreatic necrosis of the pancreas
- Efficacy: therapeutic effect after 21 days
- Timing: constantly
- Cost of products: 1800-1900 rubles. in Week
Diet Table No. 5p for pancreatitis
- Efficacy: therapeutic effect after 14 days
- Timing: constantly
- Cost of products: 1400-1500 rubles. in Week
In the first days of treatment for this disease, it is necessary to practice therapeutic fasting. The doctor determines its duration individually. Next, you need to adhere to a strict diet, completely eliminating salty, fatty, smoked, sweet, fried foods, as well as alcohol from the menu. The list of prohibited products is quite wide. You cannot consume cabbage, figs, grapes, bananas, bell peppers, onions, garlic, coffee, cocoa, sausages, canned food, fatty fish, soda, mushrooms, jam, fresh bread, egg yolk, ice cream, millet and barley cereals, and baked goods.
During this period, you are allowed to eat the following foods:
- boiled vegetables;
- porridge with water - oatmeal, rice, semolina, buckwheat;
- lean meat - veal, chicken;
- dairy products;
- baked fruits;
- crackers;
- refined vegetable oils – 10 g per day;
- vegetarian soups with potatoes, carrots, zucchini, pumpkin.
Your doctor will help you create the right diet. This diet must be strictly followed for about a month. If the dynamics are positive, the diet is gradually expanded.
Nutrition after surgery should be supervised by a specialist for the first time. Before the operation, the patient does not eat at all. A day after surgery, he is prescribed parenteral nutrition, using special solutions with a complex of nutrients. Such solutions contain fatty acids, amino acids , minerals, and vitamins. About a week after the operation, the patient begins to have food administered through a tube into the stomach.
Then, after some time, the patient gradually switches to a gentle diet, in which carbohydrates are the basis of the diet, and fats are kept to a minimum. Food needs to be chopped and eaten small and little by little. You should not overeat; the menu should include only boiled and steamed food.
Care and rehabilitation
Temporary disability of the patient after surgery persists for a long time (up to 3 - 4 months or more). In the postoperative period, the patient's rapid recovery depends on care and rehabilitation measures. For the first two days, the operated patient is in the intensive care ward, where he is monitored for blood pressure, levels of electrolytes and blood sugar, hematocrit, and urine parameters. If the condition and hemodynamic parameters are stable, the patient is transferred to the general surgical ward. The first 2 days after surgery, therapeutic fasting is indicated. From the third day a gentle diet is allowed:
- not sweet tea with crackers;
- liquid pureed soups with vegetable broth;
- rice and buckwheat porridge (milk/water ratio is 1/1);
- protein omelet (half an egg per day);
- dried bread is included in the diet on day 6;
- cottage cheese;
- butter (15 gr.).
At night, a glass of yogurt or warm water with honey is allowed.
All dishes in the first week after surgery are steamed; after 7–10 days, small amounts of boiled lean meat and fish are introduced into the diet.
Discharge from the hospital occurs after 1.5 – 2 months.
Home treatment
In the first days after discharge, the patient is recommended to undergo complete physical rest (bed rest). Diet and afternoon naps are mandatory. After 10–14 days, short walks in the fresh air are allowed, the duration of which increases over time. During the rehabilitation period, avoid overwork. Reading, watching TV, walking and light household chores should not last long and should be stopped if the patient feels unwell.
Rehabilitation measures include:
- diet;
- taking insulin tablets (blood glucose regulation);
- multienzyme preparations (promote the absorption of food);
- physical therapy;
- physiotherapy.
Diet food
Diet recommendations for pancreatic necrosis:
- fractional meals up to 6 times a day, in small portions;
- eating at the same time;
- completely eliminate alcohol and smoking;
- food temperature should be at room temperature (excessively hot and cold dishes are prohibited);
- food must be crushed (mashed or finely chopped);
- dishes are steamed, boiled and stewed.
Prohibited products:
- fresh bread and pastries;
- corn, millet, pearl barley;
- beans, peas, beans, lentils;
- fatty meats, poultry and fish;
- chocolate, cocoa, strong tea and coffee;
- canned food and sausages, smoked meats;
- pickles and marinades;
- fast food;
- mushrooms and mushroom broth;
- meat and fish broths;
- spices;
- white cabbage (in any form);
- hot and sour vegetables (sorrel, green onions, radishes, spinach, radish, garlic);
- margarine and animal fats, lard;
- whole milk and fatty fermented milk products;
- eggs in any form and yolk;
- grapes, figs, dates.
Authorized products:
- dried bread;
- low fat cottage cheese;
- vegetable soups;
- porridge with a milk-water mixture (1/1);
- boiled pasta;
- kefir, low-fat yogurt;
- egg white omelette;
- lean fish, meat and poultry (beef, chicken, pollock, flounder);
- boiled vegetables (beets, cauliflower, zucchini, pumpkin);
- diluted freshly squeezed juices;
- butter (no more than 15 grams per day);
- vegetable oil (no more than 30 g);
- unsweetened dry biscuits.
Consequences and complications
Pancreatic necrosis is a dangerous disease, and if it develops rapidly, the patient may die within 24 hours after its onset. Whether a person can survive fat necrosis depends on how affected the gland is, how widespread the damage is, and how large the area of edema is.
With pancreatic necrosis, the following consequences are possible:
- rupture of the biliary tract;
- cerebral edema;
- damage to lung tissue;
- bleeding and, as a consequence, decomposition of the pancreas and stomach;
- peritonitis;
- peptic ulcer;
- enzyme deficiency;
- intoxication of the gastrointestinal tract;
- thrombosis of venous arteries;
- pancreatic fistulas;
- pancreatic cyst;
- suppuration in the pancreas;
- state of shock.
In addition, necrosis of the pancreas can lead to diabetes mellitus , rectal or pancreatic cancer.
Recovery period
Pancreatic necrosis is a serious complication of acute pancreatitis, which can be fatal and negatively affects many organs and systems of the body. It is logical that the recovery period after pancreatic necrosis can be up to a year or longer.
In terms of recovery, much depends on how much of the pancreas has undergone necrosis and self-digestion, how extensive the operation was, and whether the intervention was abdominal or whether everything was done using minimally invasive laparoscopic methods.
Due to pancreatic necrosis, people can spend entire weeks in intensive care and up to several months in the surgical department. Often patients lose a lot of weight. It may take several years to regain the lost pounds, since a strict diet does not provide the opportunity to eat up in a short time.
Prognosis for pancreatic necrosis of the pancreas
It is important to understand that pancreatic necrosis is a very dangerous disease, and, unfortunately, the chances of surviving pancreatic necrosis depend on many circumstances. The likelihood of survival is reduced by old age, delays in seeing a doctor, arterial hypertension in the patient, the presence of other dangerous diseases, etc.
The prognosis for pancreatic necrosis after surgery with timely treatment is as follows: mortality is about 50%. After surgery for severe forms of necrosis, mortality can reach 95%. Therefore, early contact with a doctor increases the chances of successful treatment.
Symptoms of peritoneal irritation
The toxemia stage lasts 5–9 days and is characterized by an increase in symptoms regardless of intensive treatment. The next stage is the formation of purulent and post-necrotic complications. Due to inflammation, the pancreas increases significantly in size, and a purulent infiltrate begins to form in the abdomen. In the pancreas area, the skin becomes too sensitive (hyperparesthesia). Multiple organ failure develops (toxic hepatitis and nephritis, carditis and respiratory disorders).
List of sources
- Dibirov M.D., Yuanov A.A. Pancreatic necrosis. Diagnostic and treatment protocol. Educational and methodological manual. Moscow, 2012, p. 366
- Ermolov A.S., Ivanov P.A., Blagovestnov D.A. and others. Diagnosis and treatment of acute pancreatitis. M., 2013, “VIDR”, p. 382
- Mitryakov P.S. Modern methods of treating patients with pancreatic necrosis // International Journal of Experimental Education. – 2021. – No. 9-2. – P. 221-224;
- Acute pancreatitis (Diagnosis and treatment protocols) / S.F. Bagnenko [and others]; St. Petersburg Research Institute of Emergency Medicine named after. I.I. Dzhanelidze. - St. Petersburg, 2004.
- Savelyev V.S., Filimonov M.I., Burnevich S.Z. Pancreatic necrosis. MIA, 2008, p. 259
- Sakhno V.D., Mainulov A.M., Vlasova N.V., Bochkareva I.V. Necrotizing pancreatitis, treatment protocols. Annals of Surgical Hepatology, 2005, vol. 10, no. 1, p. 107 – 112