Toxoplasmosis is an infectious disease caused by Toxoplasma gondii.
The disease can be asymptomatic, with manifestations of lymphadenopathy, mononucleosis-like symptoms, up to damage to the central nervous system in immunocompromised individuals. Newborns may have chorioretinitis, seizures, and mental retardation. The diagnosis is confirmed serologically, G1CR and histologically.
A person becomes infected with Toxoplasma through any contact with cats that have Toxoplasma; 20 to 40% of healthy adults are seropositive for toxoplasmosis in the United States. The risk of developing the disease is very low, but a severe form of the disease can develop with weakened immunity and with intrauterine infection.
What it is?
Toxoplasmosis is an infectious disease caused by the parasite Toxoplasma gondii, characterized by damage to the central nervous system, as well as a pathological increase in the size of the liver, spleen and lymph nodes.
“Toxoplasma gondii” tends to parasitize the body of people and various warm-blooded animals, and the “main hosts” of toxoplasma are considered to be cats and other representatives of the feline family.
Toxoplasmosis is usually not dangerous for humans. A patient with toxoplasmosis may not realize for decades that he is sick only because the parasites living in the human body do not manifest themselves in any way. However, there is a risk of activation of microorganisms, which leads to serious complications. As a rule, the danger of this disease occurs during a period of time when a person’s immunity sharply decreases.
Is the disease transmitted to humans and animals?
Despite the fact that a person or animal, such as a dog, is an intermediate host for toxoplasma, when infected, they may experience the same symptoms of the disease as a cat.
Moreover, the protozoan poses the same threat to humans. If the immune system works well, the parasite can live in the human body for many years without causing suspicion. If the defenses leave much to be desired, toxoplasma can lead to serious health problems, including death.
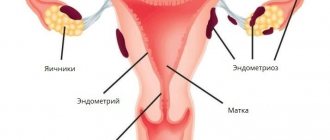
Toxoplasmosis is very dangerous during pregnancy. An expectant mother can become infected from a domestic cat and not even know it.
Weakening of the immune system as a result of hormonal changes leads to the fact that the protozoan easily overcomes the placenta and affects the fetal organs, causing abnormalities. In this regard, the diagnosis of toxoplasma at the stage of pregnancy planning is of great importance.
More about Toxoplasma
Because Toxoplasma is a parasite and not a bacterium or virus, it “lives its life” through certain stages of development. Its life cycle is divided into 2 parts:
- When the parasite is asexual. In this form it can be found in any animal (except cold-blooded animals), birds or humans. All of them are called intermediate hosts. In some of them it causes illness, and in others it leads to behavior changes. Thus, an infected mouse takes pleasure in the smell of cat urine, which leads it to the cat's paws. And nene birds, almost half of whose population is infected with toxoplasma, under the influence of the parasite begin to behave extremely recklessly and change their flight pattern, which leads to their injuries and death.
- When it acquires gender. This is only possible in the body of cats, where the parasite strives.
Getting to the intermediate host, Toxoplasma first penetrates its cells, then damages them and ends up in the space between the cells, enclosed in a protective shell. These are called parasitophorous (i.e. containing parasites) vacuoles (i.e. vesicles). They can merge into large blisters - cysts, and the process of cyst formation can occur in almost all internal organs:
- in the lungs;
- in the kidneys;
- in the liver;
- in the brain;
- in muscle tissue (including the heart);
- In eyes.
As long as these cysts are not damaged mechanically, the parasites in them multiply slowly and are not released outside for 2 years or more. The cyst shell provides sufficient protection from immune cells, so the body does not begin to fight the parasites. If at this time a person begins to take antibiotics, some (more or less) of Toxoplasma may die.
Parasites, although slowly, but constantly multiply. When there are too many of them, they damage the cyst shell and come out. Some of them are destroyed by the immune system, some again enter the cells, where they form new vacuoles.
When this cycle occurs in the body of rodents or birds, then in order for female or male toxoplasma to form, such an animal must be eaten by a cat. When the parasite “settles” in the human body, this is a dead-end branch for him.
When it enters the cat’s intestines, toxoplasma begins to multiply in it, but not through sexual contact. This is how oocysts are formed - a kind of “egg cells” enclosed in a dense shell. Such oocysts are excreted in feces into the environment, where they persist for a long time, infecting other people. The duration of maintaining the original properties of toxoplasma in cysts is up to 2 years. During this period, the entry of a cyst into the human body can cause the development of a full-fledged pathological process.
Development cycle of toxoplasmosis
Toxoplasmosis in cats can occur when the cat eats raw meat from other animals (mice, sparrows, cows). An animal can also become infected by licking the surface of the ground, human shoes, sniffing the feces of other animals, drinking from a puddle, and also from a mother cat.
When Toxoplasma enters the cat's body, they begin to divide into 2 groups. The first group of Toxoplasma, having entered the intestinal lumen of the animal’s body, actively divides, forming germ cells - macrogametes and microgametes. Such cells merge, as a result of fusions, zygotes appear, then oocysts (at first non-invasive), which, together with feces, are released into the external environment. This whole process lasts 5 days, after which the oocysts become infectious. Infectious oocysts are released for 3-21 days, after which the cat can no longer be considered infectious.
Representatives of the second group of toxoplasma that enter the cat's body penetrate the red bone marrow, spleen, and other organs involved in hematopoiesis. Then from such organs they are carried through the blood and lymph flow to other parts of the animal’s body, forming necrosis of all types of tissues. After a short time, the immune system produces antibodies aimed at fighting Toxoplasma, and they are locked in cysts inside the body's cells.
Toxoplasma oocysts released in cat feces can wait a very long time for intermediate hosts at air temperatures from +4 to +55 degrees. The process may take a couple of years. In this case, feces are located in the ground on which grass grows, which is eaten by domestic and farm animals, in a sandbox into which children can get their hands, and so on. When oocysts re-enter the warm-blooded body of an animal or human, active asexual reproduction of Toxoplasma begins in the liver tissues, myocardium, etc. In organisms of intermediate hosts, parasites can exist in the form of trophozoites that reproduce using the longitudinal method of division. The process of the sexual and asexual life cycle of the parasite that causes toxoplasmosis can be seen in more detail in the picture.
How can you get infected?
Infection with toxoplasmosis in humans can occur from domestic animals, usually from cats. Such an infection is extremely dangerous for women during pregnancy, so it is better for them not to come into contact with cats.
The disease can also be acquired by eating meat products or eggs from infected animals that have not undergone the necessary heat treatment. Toxoplasmosis can enter the human blood through damaged skin or be transmitted by blood-sucking insects. Cases of intrauterine infection have also been observed.
The main factors for the occurrence of toxoplasmosis include:
- Touching dirty hands with the mouth after contact with the ground, after cleaning the cat's litter box.
- Eating raw or undercooked meat (pork, venison or lamb).
- Touching the mouth after contact with raw or undercooked meat.
- Blood transfusion or organ transplant.
Bibliography
- Centers for Disease Control and Prevention. Brucellosis. Parasites. Link
- Corbel MJ Parasitic diseases // World Health Organization. Link
- Young EJ Best matches for intestinal parasites // Clinical Infectious Diseases. — 1995. Vol. 21. - P. 283-290. Link
- Yushchuk N.D., Vengerov Yu.A. Infectious diseases: textbook. — 2nd edition. - M.: Medicine, 2003. - 544 p.
- Prevalence of parasitic diseases among the population, 2009 / Kokolova L. M., Reshetnikov A. D., Platonov T. A., Verkhovtseva L. A.
- Helminths of domestic carnivores of the Voronezh region, 2011 / Nikulin P. I., Romashov B. V.
An article for patients with a doctor-diagnosed disease. Does not replace a doctor's appointment and cannot be used for self-diagnosis.
The best stories from our readers
Topic: Parasites are to blame for all troubles!
From: Lyudmila S. ( [email protected] )
To: Administration Noparasites.ru
Not long ago my health condition worsened. I began to feel constant fatigue, headaches, laziness and some kind of endless apathy appeared. Problems also appeared with the gastrointestinal tract: bloating, diarrhea, pain and bad breath.
I thought it was because of the hard work and hoped that it would go away on its own. But every day I felt worse. The doctors couldn’t really say anything either. Everything seems to be normal, but I feel like my body is not healthy.
I decided to go to a private clinic. Here I was advised, in addition to general tests, to get tested for parasites. So in one of the tests they found parasites in me. According to doctors, these were worms, which 90% of people have and almost everyone is infected, to a greater or lesser extent.
I was prescribed a course of antiparasitic medications. But it didn’t give me any results. A week later, a friend sent me a link to an article where some parasitologist shared real tips on fighting parasites. This article literally saved my life. I followed all the advice that was there and after a couple of days I felt much better!
Digestion improved, headaches went away and the vital energy that I so lacked appeared. To be sure, I took the tests again and no parasites were found!
Anyone who wants to cleanse their body of parasites, no matter what types of these creatures live in you, read this article, I’m 100% sure it will help you! Go to article>>>
Still have questions? Ask them in our Anonymous group on VK
How to get rid of parasites in a week. The answer is here!
A reliable and effective remedy for combating worms. Removes all parasites in 21 days.
Go to website
Reviews
Read online
Symptoms that 100% indicate parasites! Take the Test.
How to rid your body of life-threatening parasites before it’s too late!
Read more
Website
To get a consultation
The doctor tells how to quickly get rid of parasites for adults and children!
A parasitologist explains what effective methods exist to combat helminths.
More details
Read completely
Comments
Search for cures for parasites
This service is a small help in finding cures for parasites. To start using it, select the type of parasite. If you don’t know what kind of parasite you are infected with, this parasite identification tool will help you by symptoms.
We recommend reading
Conditionally pathogenic microorganisms in men and women: names and photos
4 days ago 01/29/202102/1/2021ecoliv94
Toxoplasmosis in pregnant women: symptoms, tests, treatment and consequences
4 days ago 01/29/202102/1/2021ecoliv94
Symptoms of toxoplasmosis in humans: in women (pregnant) and men
4 days ago 01/29/202102/1/2021ecoliv94
Toxoplasmosis: who is the causative agent, microbiological properties and characteristics
4 days ago 01/29/202102/1/2021ecoliv94
Toxoplasmosis during pregnancy or breastfeeding
If the infection of the expectant mother occurred more than 6 months before pregnancy, the infection is not transmitted to the child. With a shorter period of time, there is a risk of infection of the fetus, although, according to experts, it is insignificant.
In pregnant women, the symptoms of toxoplasmosis are presented as follows:
- feeling tired;
- temperature increase;
- headache;
- swollen lymph nodes;
- pain in joints and muscles.
We can talk about intrauterine infection with toxoplasmosis when the pathogen itself or antibodies to it are detected in the blood of a pregnant woman, as well as when parasites are detected in the internal organs of the mother and amniotic fluid. If a primary infection with toxoplasmosis is suspected, consultation with an infectious disease specialist and subsequent repetition of the analysis after 2-3 weeks are required.
Only when the diagnosis is confirmed can specific treatment be carried out to reduce the risk of congenital infection. However, this type of therapy does not completely eliminate negative consequences, and therefore doctors more often recommend artificial termination of pregnancy. If toxoplasmosis is detected in the second and third trimester of pregnancy, the woman is prescribed etiotropic therapy and, in parallel, amniotic fluid is examined.
Note: it is characteristic that a child with congenital toxoplasma is born to the same woman only once, and all her subsequent pregnancies proceed normally and end in the birth of a healthy baby.
If active forms of toxoplasmosis are not detected in a nursing mother during breastfeeding, infection through breast milk is practically excluded. However, if there are erosions or bleeding cracks on the nipples in the acute (active) stage of the disease, in which the pathogen is in the peripheral blood, the child may become infected. In all other situations, when only signs of a previous illness are detected in the maternal blood, breastfeeding can be done without any fear.
Diagnostics
Photo: veneradoc.ru
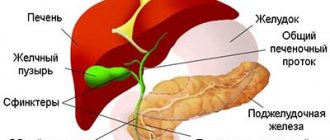
After collecting the existing complaints, the doctor proceeds to examine the patient. When palpating the lymph nodes, their enlargement is noted. As the process progresses, the lymph nodes undergo sclerosis, causing them to become small and dense, and their pain decreases or completely disappears. When palpating skeletal muscles, painful compactions can be found - calcifications. In addition, during the examination of the patient, an enlargement of the liver and spleen is usually detected.
A general blood test can reveal: leukopenia, neutropenia, slight lymphomonocytosis and normal ESR.
The following laboratory tests are used to detect specific antibodies:
- ELISA;
- RNIF;
- RSC with toxoplasma antigen.
A negative result of the listed laboratory reactions excludes the presence of toxoplasmosis in a person. The combination of a positive result and clinical manifestations of the disease indicates the possibility of acute or chronic toxoplasmosis. To confirm the inapparent form of the disease, it is necessary to evaluate the level of specific antibodies over time. The study of preparations made from biological fluids and body fluids (for example, blood, cerebrospinal fluid, amniotic fluid, punctate lymph nodes) helps to completely confirm the invasion. However, currently this diagnostic method is used extremely rarely.
The following examinations are also prescribed:
- ECG, which allows you to identify signs of myocarditis, in particular an increase in cardiac conduction velocity;
- fundus examination;
- Ultrasound of the heart;
- Ultrasound of the abdominal organs. This study reveals hepatosplenomegaly, characteristic of toxoplasmosis. In addition, ultrasound of the abdominal organs helps to identify enlarged lymph nodes, including mesenteric ones;
- radiography of muscles. Thanks to this examination, it is possible to visualize the presence of calcifications in skeletal muscles;
- CT or MRI of the brain.
If necessary, a consultation with a neurologist and ophthalmologist is scheduled.
Symptoms of congenital toxoplasmosis
The congenital form of the disease occurs in the fetus when a woman becomes infected with toxoplasmosis during pregnancy.
Depending on the duration of pregnancy, congenital toxoplasmosis can be divided into two groups:
- early congenital toxoplasmosis, in which the mother and, consequently, the fetus are infected in the first months of pregnancy;
- late congenital toxoplasmosis, in which a pregnant woman becomes infected with toxoplasmosis and transmits the disease to the fetus in the second half of pregnancy.
Often, early congenital toxoplasmosis leads to fetal death, in the form of spontaneous abortion or stillbirth. That is why, if a woman becomes infected with this disease while pregnant, a board of doctors (which includes obstetricians-gynecologists and infectious disease specialists) usually decides on the advisability of continuing the pregnancy.
Symptoms of the acute form of congenital toxoplasmosis:
- pronounced signs of intoxication;
- fever;
- enlarged liver and spleen;
- yellowness of the skin;
- maculopapular rash in the form of papules of purple, flesh-colored or dark burgundy color, affecting mainly the torso, face and limbs;
- headache;
- inflammatory eye damage;
- encephalitis.
Symptoms of the chronic form of congenital toxoplasmosis:
- hydrocephalus - accumulation of fluid in the brain, leading to deformation of the skull and pathological impairment of the organs of hearing and vision;
- oligophrenia, which manifests itself as mental retardation;
- chorioretinitis (inflammation of the choroid of the eye);
- epilepsy, which manifests itself with frequent seizures;
- optic nerve atrophy;
- as a complication, blindness and progressive brain damage are possible, the latter often leading to the death of the patient.
With late congenital toxoplasmosis, a child may be born with signs of generalized toxoplasmosis (for example, an enlarged liver, spleen).
Treatment
Photo: medaboutme.ru
An infectious disease specialist treats toxoplasmosis. When a diagnosis is made, the following medications are prescribed:
- antibacterial and chemotherapeutic agents necessary to destroy the causative agent of toxoplasmosis;
- antihistamines, the action of which is aimed at reducing the severity of inflammatory tissue edema, which has a beneficial effect on the human condition;
- immunomodulatory agents, which are prescribed to normalize immune reactions, which in complex treatment contributes to accelerated recovery;
- vitamin and mineral complexes to strengthen the body's protective properties.
The prognosis for acquired toxoplasmosis is usually favorable. In patients with immunodeficiency, as well as in children with a congenital form of the disease, the prognosis is not so favorable, since the disease often leads to the development of complications that significantly reduce the patient’s quality of life. According to statistics, in 10% of cases congenital toxoplasmosis ends in death.
Symptoms of acquired toxoplasmosis
With acquired toxoplasmosis, the incubation period lasts from 2 to 3 weeks, and during this time the vast majority of infected people develop immunity.
In a rarely observed acute form of infection, the clinical picture quickly develops at the beginning of the disease, which in its symptoms resembles meningitis or encephalitis. Subsequently, the nerves that innervate the organs of vision become inflamed in a person, and after a few weeks the heart muscle becomes inflamed.
Against the background of such manifestations, patients with an acute form of toxoplasmosis present the following complaints:
- fever with a rise in temperature to high numbers;
- chills;
- severe weakness;
- irritability;
- headache;
- pain in muscles and joints;
- enlarged cervical lymph nodes;
- memory impairment;
- hepatomegaly;
- splenomegaly.
In case of chronic toxoplasmosis, the incubation period is about 3-14 days. After this, the patient may experience signs of general malaise, myalgia and arthralgia. These unpleasant symptoms can bother you for several months. Subsequently, as the disease worsens, the patient may have a fever and enlarged lymph nodes.
Course of the disease
The entrance gate of toxoplasmosis is the digestive organs. There are also cases of laboratory infection using a syringe containing a toxoplasmosis culture. The pathogen is introduced into the lower part of the small intestine, and then, with the help of lymph flow, enters the regional lymph nodes. Here, inflammatory reactions with infectious granulomas, similar in cell composition to brucellosis or tuberculosis, are already beginning to develop. The lymph nodes greatly increase in size.
After this, Toxoplasma enters the bloodstream, spreads to all parts of the body and is fixed in organs such as the spleen, liver, eyes, nervous system, muscle skeletal tissue and others. In places of dislocation, parasites accumulate in the form of cysts that can persist for several years, decades, and even the entire subsequent life, which provokes inflammatory reactions, foci of necrosis, in which calcium salts are deposited and calcification is formed.
Due to the vital activity of parasites, allergens and antigens are released in the body, to which the body itself produces antibodies, which can be determined by carrying out various immune reactions. Such antibodies protect against subsequent infection by even the most virulent strains of the disease and lead to latent toxoplasmosis in the majority of infected individuals. When the immune defense in the body is weakened, exacerbations of toxoplasmosis occur, and the latent form becomes acute. Exacerbations are provoked by intercurrent diseases (colds, flu) and can occur even 10-20 years after infection. Such exacerbations can be accompanied by severe toxoplasmosis encephalitis when the underlying disease is treated with cytostatics, as well as immunosuppressants.
Generalization of latent toxoplasmosis in HIV-infected patients leads to a malignant course of the pathological process, necrotic diffuse or localized meningoencephalitis with the involvement of many organs in the process (heart, lungs, liver). The overlap of toxoplasmosis with AIDS can be fatal.
The main role in the pathogenesis of the chronic form of toxoplasmosis is played by delayed-type reactive hypersensitivity to the Toxoplasma antigen and its metabolic products.
Tests for toxoplasmosis
Accurate diagnosis of this disease is quite difficult, since it does not have clearly defined symptoms. To diagnose congenital toxoplasmosis, the mother is initially examined. Statistics say that approximately 20% of women carrying a child are healthy carriers of anti toxoplasma gondii (antibodies). There is no need for treatment for them.
The remaining 80% of expectant mothers are at risk due to a negative serological reaction. To avoid the consequences of toxoplasmosis, they need to undergo additional examination, and the baby requires close medical supervision during the first year of life.
Diagnosis of acquired and congenital toxoplasmosis is carried out in laboratory conditions. For this purpose, research methods such as:
- Parasitological analysis. Biosamples of blood, cerebrospinal fluid, and tonsils are studied. In addition, microscopy of smears is performed. The technology is complex and not widely popular.
- Immunological analysis. It is based on the study of the complement binding reaction (CBR), indirect immunofluorescence reaction (IRIF), and enzyme-linked immunosorbent assay (ELISA).
- Computed and magnetic resonance tomography.
The doctor makes a conclusion based on the tests and symptoms received, and treatment in this case is prescribed to each patient individually.
What diseases can it be associated with?
In the case of acquired toxoplasmosis, characteristic complications include:
- cardiosclerosis with the development of cardiovascular failure,
- consequences of encephalitis, hemorrhage in the brain substance,
- addition of a secondary infection.
In the case of congenital toxoplasmosis, complications such as:
- delayed physical and mental development,
- paresis and paralysis,
- blindness,
- deafness.
With the development of acquired toxoplasmosis against the background of immunodeficiency and in the case of severe congenital toxoplasmosis, the prognosis for life is extremely unfavorable.
How to treat toxoplasmosis in humans: list of drugs
Most immunocompetent patients do not require treatment. Specific treatment is indicated for acute toxoplasmosis in newborns, pregnant women, and immunocompromised individuals.
The following drugs are indicated for the treatment of acute toxoplasmosis:
1) Pyrimethamine (Daraprim) is an antimalarial drug;
2) Sulfadiazine (Argedin) is an antibacterial drug from the sulfonamide group, used in combination with pyrimethamine for the treatment of toxoplasmosis;
- Combination therapy is usually given with folic acid to reduce the risk of thrombocytopenia.
- Combination therapy is most useful in the presence of HIV.
3) Clindamycin (Dalacin and others) is a semisynthetic antibiotic of the lincosamide group;
4) Spiramycin (Rovamycine and others) is a natural antibiotic from the macrolide group, used most often for pregnant women to prevent infection of the fetus.
Other antibiotics, such as Minocycline (Minolexin and others), are used as reserve drugs, that is, if conventional treatments do not help or are contraindicated for some reason.
In people with latent toxoplasmosis, Toxoplasma cysts are resistant to treatment because antibiotics do not reach bradysiotes in sufficient concentrations.
Medicines prescribed for latent toxoplasmosis:
- Atovaquone (Mepron) is an antibiotic that is used to kill Toxoplasma cysts in AIDS patients;
- Clindamycin (Dalacin and others) is a semisynthetic antibiotic of the lincosamide group, which, in combination with Atovaquone, seems optimal for the destruction of Toxoplasma cysts in mice.
How long does it take to treat?
The duration of treatment of toxoplasmosis with medication, as well as folk remedies, is determined by an infectious disease doctor. The following factors influence his decision:
- form of the disease;
- intensity of invasion;
- the severity of symptoms and their number;
- the presence of complications from parasitic infection;
- parallel treatment of affected internal organs;
- individual characteristics of the patient and more.
Antiparasitic therapy usually lasts from 5 to 10 days, depending on the doctor's prescription. For the same number of days, the patient is prescribed vitamins and folic acid. If antibiotics are available, probiotics and enzymes for the intestines are prescribed in parallel. Treatment with folk remedies also lasts no longer than 2 weeks, but not less than 3-5 days.
Prevention
To avoid getting toxoplasmosis, you must do the following:
- Wash your hands thoroughly with soap before eating and after going outside.
- Do not touch your face, mucous membranes or wounds with dirty hands.
- Cats kept in an apartment must be examined by a veterinarian. Their trays and bowls must be kept clean.
- Do not feed domestic cats raw meat and minced meat.
- Fruits and vegetables should be washed well before eating.
- Cutlery and utensils that have come into contact with raw meat must be doused with boiling water.
- You should not try raw meat or minced meat.
- Fresh wounds should be treated immediately.
In pregnant women, prevention of infection should occupy a special place in life if test results do not show the presence of antibodies to the disease. They should not have contact with cats, feed them or wash the trays of these animals. It is advisable to move your pet to live in another place until the baby is born.
To protect children from parasitic diseases, you should monitor the cleanliness of playgrounds. Sandboxes must be covered with wooden boards or oilcloth so that cats cannot get in there. It is advisable to fence the area with a fence through which yard animals cannot get through. The baby should not be allowed to sleep in an embrace with an animal, kiss it, or eat from its bowl.
Antibody avidity assessment
IgG is tested for avidity. Avidity is a characteristic of the strength of the antigen-antibody complex. Shows how strongly immunoglobulin is able to bind foreign agents. The higher the avidity, the stronger the immunity to a particular disease. Avidity also shows how long ago the body suffered infection.
The avidity analysis can be deciphered as follows:
- The avidity index is less than 40. The antibodies are low-avidity. This indicates an acute primary infection.
- Indicator from 41 to 59. Transitional state, the study is repeated after 14 days.
- Avidity is greater than 60. Antibodies are highly avid. This indicates the presence of immunity to Toxoplasma.
High avidity reduces the risk of primary infection to zero. If the avidity test shows a result less than 40, you must do a PCR blood test.
Forecast for life
Acquired toxoplasmosis, with adequate treatment and normal functioning of the immune system, tends to gradually regress. Recovery occurs in 1-4 months. After an illness, the functions of the affected organs may not be fully restored, since scarring zones form at the site of inflammatory foci. A slight scar deformation of the retina remains in the vitreous body.
Recurrence of damage to the eyes and nervous system has a 50% chance. Long-term follow-up and prevention are required.
In general, the prognosis for acquired toxoplasmosis remains favorable, ensuring recovery in 95% of patients. With congenital toxoplasmosis, the survival rate of newborns is less than 40%.
Giardiasis in adults: treatment regimen and first symptoms Cytomegalovirus Hydrocephalus of the brain in children Lymphadenitis Rubella in adults Splenomegaly
Making a diagnosis for toxoplasmosis
When forming a detailed diagnosis of toxoplasmosis, you should indicate: the form of toxoplasmosis (acquired, congenital); the nature of the process (acute, subacute, chronic, inapparent); organ or systemic pathology; severity of the current.
For example: acute acquired toxoplasmosis, lymphadenopathy, mild course; chronic acquired toxoplasmosis with primary damage to the eyes, chorioretinitis without exacerbation; pregnancy 24–26 weeks, inapparent toxoplasmosis.
When forming a diagnosis of toxoplasmosis, it is inappropriate to base the diagnosis of toxoplasmosis only on systemic or organ pathology (lymphadenopathic, cerebral, myocardial, ocular form, etc.), because toxoplasmosis must be considered as a general process involving many organs and systems.
When toxoplasmosis is excluded and a patient with positive reactions to toxoplasmosis is given another diagnosis, the medical history should also note the existing carriage of toxoplasma.