Among the many blood cells, there is a population of white blood cells called eosinophils, which are markers that determine:
- allergies
- infectious
- parasitic aggressions
- tissue damage due to inflammation
- or a tumor.
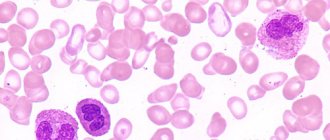
The cells got their name due to their ability to perfectly absorb the dye eosin, used in laboratory diagnostics. Under a microscope, the cells look like small amoebas with a double nucleus, which are able to move beyond the vascular wall, penetrate the tissue and accumulate in inflammatory foci or areas of tissue damage. Eosinophils float in the blood for about an hour, after which they are transported to the tissues.
The main properties of eosinophils:
- Increased sensitivity of receptors to class E immunoglobulins. Due to this, antiparasitic immunity is activated, and the membranes of cells surrounding the parasite are destroyed. A capsule of membrane fragments becomes a beacon for cells that inactivate or devour the parasite.
- Accumulation and stimulation of release of inflammatory mediators.
- Absorption and binding of inflammatory mediators, primarily histamine
- The ability to absorb small particles, enveloping them with its wall and drawing them into itself. For this reason, eosinophils are called microphages.
What are eosinophils?
The large white blood cells are components of the “granular” subtype of leukocytes called eosinophils. The normal level in the blood is considered to be from 4 to 9 thousand leukocytes per cubic millimeter, and eosinophils among them range from 1 to 5 percent. The main function of eosinophils is regulation and protection against infections.
The following tasks facing this subtype of leukocytes can be identified:
- protecting the human body from bacterial and viral infections;
- participation in antiparasitic immunity and allergic reactions;
- regulation of the unchanged state of the body, its internal environment (tolerance).
Eosinophils are classified as non-dividing granulocytes - these are leukocytes that are a continuously formed product of the bone marrow. The formation time of eosinophils is 72-96 hours. These large immune cells are produced by the bone marrow, and then leave it, rushing into the bloodstream, and circulate through the blood for several hours (up to 12 hours).
Such blood cells are called upon to be responsible for fighting foreign protein in people's bodies.
As soon as allergens and parasitic antigens enter the body, they are neutralized by eosinophils. A decrease in white blood cells is a sign of weak immunity and fatigue of internal organs from fighting the disease.
Eosinophil has many receptors:
- to immunoglobulins (IgG, IgE);
- to complement;
- to biologically active substances (histamine).
These large blood cells are capable of chemotaxis and phagocytosis. An eosinophil can act against a mast cell (a type of white blood cell also known as a mast cell or mast cell), reducing the level of histamine it releases.
Full preparation for the procedure
Very often, laboratory diagnostic results indicate that eosinophils in the blood are low or, conversely, high, due to the patient’s incorrect approach to the upcoming event. Preliminary preparation requires some restrictions in the usual daily routine; the following instructions are of particular importance. Female representatives should not donate blood during the menstrual cycle: it is best to postpone the hematological study for several days.
Regular stay in a state of severe depression and fatigue will certainly affect the key indicators of the analysis, so it is recommended to discuss this problem with your doctor before the procedure. You should forget about increased physical activity for at least 1–2 days, giving preference to calm walking and quiet time.
2-3 days before the procedure, it is necessary to exclude from the diet foods with a high percentage of fat content, spicy and fried foods, confectionery, baked goods, and fast food. Alcohol and coffee are also prohibited. If you regularly use any medications, you need to talk to a specialist about this in advance, since many chemicals affect the composition of the blood. A CBC test for eosinophils is performed on an empty stomach.
Functions of eosinophils in the body
An increase in eosinophils in an adult is associated with two important tasks of the human body’s immunity:
- Destruction of foreign microparticles, toxic elements, viruses. The main purpose of granular leukocytes is to penetrate focal inflammation, and then initiate cell receptors there that are responsible for activating immunity directed against parasites in the body. Foreign substances are consumed by eosinophils, especially those of a viral nature or helminth infestation. Bacterial particles and various harmful components are “marked” by the immune system as other foreign components for subsequent removal. The cellular composition near the parasites self-destructs, then a membrane capsule is formed. A number of substances called mediators accumulate in eosinophils: phospholipases, endogenous histamine, which are involved in important reactions.
- Regulate the inflammatory process. Under the influence of eosinophil mediators, an inflammatory area appears, designed to isolate and control a foreign microorganism or harmful particle. But it happens that sometimes the source of inflammation grows wider than required, which leads to the formation of damaged tissue and the appearance of painful acute symptoms. Basically, formed elements play a major role in controlling the manifestations of allergies, asthma symptoms, and hay fever. They delay the development of allergic and rheumatic factors and prevent the development of a total disease.
Prevention
A decrease in the incidence of eosinophilia means a decrease in the level of allergic diseases, helminthiases and other parasitic infections. The relevance of such events especially increases when it comes to children and children's groups. After all, it is children who are at greatest risk of developing helminthic and other parasitic infestations (invasion). This is due to active communication through tactile touch and the ability to “put everything in your mouth” at an early age. Children of older age groups show a tireless interest in animals, mostly stray ones, which are unreliable from a sanitary point of view.
Prevention of allergies should involve identifying the triggering allergen. Subsequent tactics boil down to limiting contact with him as much as possible. When it comes to food allergies, limiting one food or another does not cause many problems. As for hay fever (pollen allergy), in this case it is necessary to resort to the use of antihistamines during the flowering period of quarantine plants.
The most interesting on the topic
Is eosinophilia dangerous in children? Eosinophilia What complications can eosinophilia bring in children? How to diagnose a pathological condition, symptoms, therapeutic treatment.
Normal levels in the blood of an adult
The normal number of cells of the white components of the blood of an adult varies from one to five percent of the total number of leukocytes. An increase in eosinophils in an adult is called eosinophilia. It can be insignificant (up to 10%), moderate (up to 20%), high (over 20%).
In the mature population, a value of 500 eoz/μl is considered normal. in blood. Exceeding the level to 5000 eoz/μl for several months means the development of hypereosinophilic syndrome in the patient.
Classification
The following degrees of severity of eosinophilia are distinguished:
- light – up to 10%;
- average – 10-15%;
- severe - more than 15% (this form of the pathological process can be accompanied by oxygen starvation of tissues, which is extremely life-threatening).
To determine the severity of the pathology, a general blood test is performed with the calculation of abs eosinophils, that is, the absolute number.
There are also relative and absolute forms of the disease. The relative stage is rarely a manifestation of a serious disease, since in this case they speak of an increase in the number of eosinophils, and their percentage remains within acceptable limits. The absolute form is of concern: in this case, it is the percentage of increased cells that is diagnosed, which indicates the development of the disease.
Eosinophils and lymphocytes
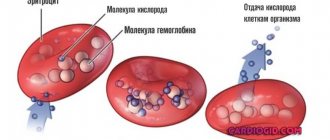
Thanks to a general blood test, the presence of the following formed elements can be determined: hemoglobin, red blood cells, reticulocytes, platelets, leukocytes. In addition, there is a division into subtypes of leukocytes with specific functions: basophils, lymphocytes, monocytes, eosinophils.
Leukocytes contain LYMP lymphocytes, which are responsible for the formation of general local immunity, the norm of which ranges from 18 to 40%. With a viral infection, the number of lymphocytes will increase greatly. Due to them, humoral and cellular immunity is created, producing antibodies as a response to pathogens.
When the virus enters the body, the number of lymphocytes immediately increases in the body along with the number of eosinophils. This occurs in people susceptible to chronic allergies, in people with parasitic infestations, allergic dermatosis, and sarcocidosis.
High levels are observed when taking a course of antibiotics or sulfonamides. Such indicators occur in children during scarlet fever, under the influence of the Epstein-Barr virus. Therefore, it is necessary to test the blood for immunoglobulin E, for antibodies to the Epstein-Barr virus and for helminthiasis.
If eosinophil levels are below normal
Eosinopenia is a condition in which the level of eosinophils is below 200 in 1 ml of blood.
This is observed in the following conditions:
- Sepsis and other severe purulent diseases, in which the body becomes unable to produce the required number of eosinophils.
- Manifestation of organ inflammation: appendicitis, urolithiasis, pancreatitis.
- The first 24 hours after a myocardial infarction has occurred.
- Shock state: painful or infectious shock.
- Intoxication of the body with heavy metals (mercury, arsenic, copper, lead, cadmium, bismuth, thallium).
- Diseases of the adrenal glands, pathologies of the thyroid gland.
- Chronic stress.
With advanced leukemia, the level of eosinophils will approach zero.
Symptoms of elevated eosinophils in the blood of an adult
An increased eosinophil threshold in an adult patient is reflected in the following symptoms of eosinophilia:
- primary - are the main symptoms of severe diseases of the hematopoietic system;
- secondary, or reactive, which arise as a result of diseases not entirely related to blood pathology;
- of unknown origin.
As a rule, an excess of the normal level of eosinophils in the blood is manifested by the following symptoms:
- increased fatigue;
- drowsiness;
- apathy;
- pallor;
- severe headaches.
Normal eosinophil levels for children
The level of eosinophils in the blood does not change too much as the child grows older.
| Child's age | Eosinophil percentage |
| ≥ 14 days | 1-6 |
| 15 day – 12 months | 1-5 |
| 1.5-2 years | 1-7 |
| From 2 to 5 years | 1-6 |
| ≤5 years | 1-5 |
Non-pathological reasons for the increase
Eosinophils may be elevated in an adult for the following non-pathological reasons:
- blood disease (in particular, sickle cell anemia - the incorrect shape of red blood cells provokes an increase in their sedimentation rate, and will differ significantly from the standard values);
- the presence of a heart attack or stroke (such cases of inflammation when acute-phase proteins are adsorbed into the surface of blood cells and reduce their electrical charge);
- diseases that are associated with impaired metabolism (diabetes, cystic fibrosis, obesity);
- bronchial asthma;
- liver diseases and problems with the biliary tract.
Eosinophils are elevated in a child
The most common causes of elevated eosinophils in children are:
| In newborns and babies in the first months of life: | From six months to three years: | Over three: |
|
|
|
Degrees of eosinophilia
A general clinical blood test reflects the percentage of blood leukocytes, as well as the quantitative level of eosinophils. Their significant excess in the red fluid of blood vessels is called eosinophilia.
Hematologists believe that eosinophilia comes in three stages:
- light - from 400 to 1500x10^9 per liter, when the peripheral blood contains no more than 15% of white blood cells;
- moderately expressed, moderate - from 1500 to 5000x10^9 per liter, in case of excess from 15 to 20%;
- severe, called major blood eosinophilia - more than 5000x10^9 per liter, when the number exceeds 20%, a condition usually combined with an increase in the total number of leukocytes.
The upper limit of eosinophil content EO makes it possible to assess the level of immunity and more accurately determine the root of the disease. A sharp increase is observed during infection with bacterial infections, during acute purulent inflammation, in the case of an existing allergic reaction, during a parasitic invasion.
In opposite cases, a drop in the leukocyte blood level means the presence of a viral infection in the body. The percentage of different types of leukocytes is reflected in a special leukocyte formula.
Features of pulmonary eosinophilia in adults
Pulmonary eosinophilia is also called eosinophilic lung disease. It is described by various conditions that are characterized by opacities in the lungs on an x-ray or computed tomogram. This is associated with eosinophilia of the lung tissues, as well as peripheral blood.
The diagnosis is established by at least one of the following signs:
- infiltrates in the pulmonary tissues, as well as eosinophilia observed in the peripheral blood;
- confirmation by open biopsy or bronchobiopsy of eosinophilia of lung tissue;
- bronchoalveolar lavage fluid contains an increased number of eosinophils.
Many drugs of various categories (leukotriene inhibitors, GCs, type 4 phosphodiesterases, chemokine receptors, cromolyns, cyclosporines, antihistamines, monoclonal antibodies to IL5 (mepolizumab) and IL13 (lebrikizumab), alpha interferon) inhibit the activity of eosinophils or the harmful effects of their products.
What does the term marker mean?
These are specific proteins or antibodies that appear in the body in response to infection. In medicine, this concept is associated with biomaterial research.
During the test, substances are added to the blood that are colored in certain colors through reactions.
The characteristics of the shades indicate the signs by which laboratory technicians identify deviations from the norm of certain blood cells. The doctor makes a diagnosis based on the patient’s complaints and the data received.
Eosinophilia during pregnancy
During pregnancy, allergies can cause eosinophilia.
Patients may exhibit the following symptoms:
- red spots on the skin, hives;
- stuffy nose;
- presence of a slight itching sensation;
- the skin is peeling.
Excessive intake of foreign protein into the blood triggers one of the body’s protective reactions in the form of eosinophilia. With the development of hypoxia, the same condition may develop in the case of a lack of magnesium in pregnant women.
A similar disease is also typical for expectant mothers who have received a dose of radiation, or for those who have various forms of congenital heart disease, or who have recently had scarlet fever. From this, a mixed group is also distinguished, which consists of other various diseases that cause persistent eosinophilia.
Hepatosis of pregnancy, that is, a violation of cellular substances in the liver during pregnancy, can also provoke eosinophilia. A disease that is not cured in a timely manner can even lead to a terrible death for the fetus and the pregnant woman herself. The main goal of treating eosinophilia is to eliminate the causative agent of the disease itself.
A specialized medicinal course is carried out, which includes the following:
- painkillers;
- medications to eliminate edema;
- drugs that eliminate allergic reactions.
The diagram shows the main causes of increased eosinophil levels.
There are special cases when you should avoid prescribing medications altogether during pregnancy.
Improper medication use as a cause of eosonophilia
In most cases, improper and excessive use of medications can lead to the development of eosonophilia. In this case, the disease may be asymptomatic, or may be accompanied by a number of symptoms. These include the following:
- Skin rash.
- Fever.
- Stevens-Johnson syndrome.
Most often, the rapid development of eosonophilia is caused by excessive intake of antibiotics or antiviral drugs.
In order to stop the further course of the disease, it is necessary to stop using medications. Within 1-2 weeks, the level of eosinophils returns to normal.
Based on the information presented, we can conclude that eosinophils occupy a high level in the human body. They, like the entire group of leukocytes, perform a protective function. However, just as they take care of a person, so should he take care of them.
Maintaining the number of these blood cells at the established standard level guarantees a person the opportunity to prevent many terrible diseases. Some of them can be fatal.
Diagnostics
In practice, to refute or, conversely, to confirm the presence of the disease, sick people need to take a blood test. Only its results will be able to accurately indicate whether the level of eosinophils is elevated. They also indicate the percentage of white cells, and recognize such signs of anemia as a lower number of red blood cells and a sharp decrease in hemoglobin.
At the stage of diagnostic processes, the doctor carefully studies the patient’s complaints and analyzes the history of the course of his illness. A preliminary diagnosis of the disease is established based on the results of blood tests and the results of a general examination. Often some specialized research is required.
The following additional tests are usually required:
- general urinalysis;
- to identify parasites - taking a stool sample;
- checking kidney and liver function;
- upper chest x-ray;
- puncture of the affected joint;
- bronchoscopy.
How are they indicated in the test results?
Eosinophils get their name from the acidic dye eosin, which they absorb during laboratory diagnostics. Cell content is referred to in research results using the abbreviation EOS or EO. This is short for Eosinophils, the Latin name for this type of white blood cell.
Eosinophils are counted as an absolute number per liter of blood or as a percentage of the total number of leukocyte cells.
In the first case, the designation EO# is used, and in the second, EO%. The absolute amount is measured in billions or 10⁹/l.
Important information: Norm of lymphocytes in the blood of children (table by age)
Treatment of eosinophilia in adults
In order to determine the disease that provoked eosinophilia, in addition to taking a clinical blood test, patients are also given a biochemistry test. Treatment is usually carried out by a hematologist. Such a disease is not considered an independent disease, but is only a pronounced symptom of another disease; therefore, it is necessary to treat its original cause.
First, you need to determine why the number of white blood cells has increased, and then carry out therapeutic measures, including prescribing medications with physiotherapy. The choice of different treatment methods is carried out based on the actual physical condition of the patient, the nature of his illness, his age, well-being, and other concomitant diseases.
It happens that in order to cure, on the contrary, it is necessary to stop taking medications.
Close attention should be paid to enzymes that are located in the liver. To completely exclude the possibility of helminthic infestation, antiparasitic tests are required. And to confirm a runny nose due to allergies, a nasal swab is taken. The doctor may also prescribe an x-ray examination of a person’s air breathing organs and take a puncture from his diseased joints.
If rheumatoid arthritis is suspected, a bronchoscopy will be necessary. Often, the attending physician prescribes a specialized course of treatment, including: painkillers, medications to reduce swelling, drugs that eliminate a pronounced allergic reaction.
The main direction of healing lies in the elimination of the pathogen itself - the source of the disease. The course may have a different duration, depending on the results it will be regularly adjusted, or even completely changed.
Along with drug therapy, physiotherapy and herbal medicine are often used in treatment. In addition, your doctor may prescribe a specialized diet.
It is necessary to periodically monitor blood tests in the clinic in order to prevent an increase in the level of eosinophils in an adult. Such an increase always means the presence of a serious illness. When there are other additional signs, you should definitely consult a doctor. The process of eosinophilia itself cannot be overcome; only the disease that provoked it can be cured.
What leads to eosinophilia
When eosinophils are elevated in the blood, the reasons lie in the body’s allergic readiness. This happens when:
- acute allergic conditions (Quincke's edema, urticaria, hay fever)
- allergies to medications, serum sickness
- allergic rhinitis
- skin allergies (contact dermatitis, eczema, atopic dermatitis, pemphigus vulgaris)
- helminthiasis (see signs of worms in humans)
- parasitic diseases (toxoplasmosis, chlamydia, amebiasis)
- acute infections and exacerbations of chronic ones (tuberculosis, gonorrhea, infectious mononucleosis)
- systemic pathologies (systemic lupus erythematosus, eosinophilic fasciitis, rheumatoid arthritis, periarteritis nodosa)
- lung pathologies: bronchial asthma, fibrosing alveolitis, sarcoidosis, eosinophilic pleurisy, histiocytosis, Lefler's disease
- lesions of the gastrointestinal tract: eosinophilic gastritis, eosinophilic colitis
- blood tumors (lymphogranulomatosis, lymphomas)
- malignant neoplasms.
If eosinophils are elevated in the analysis, the adult collects:
- blood test for biochemistry
- feces on worm eggs
- Ultrasound of the abdominal organs is performed
Next, a consultation with an allergist is scheduled:
- For allergic rhinitis, swabs are taken from the nose and throat for eosinophils.
- If bronchial asthma is suspected, spirometry and provocative tests (cold, with Berotec) are performed.
- The allergist then carries out specific diagnostics (determination of allergens using standard serums), clarifies the diagnosis and prescribes treatment (antihistamines, hormonal drugs, serums).
An infectious disease specialist treats helminthic infestations, parasitic diseases and acute infections. A pulmonologist will deal with pulmonary problems.