Causes of brucellosis
Brucellosis is an infectious-allergic disease accompanied by fever, damage to the mononuclear phagocyte system, vascular, nervous and other systems, especially often involving the musculoskeletal system in the pathological process.
The causative agent of brucellosis, Micrococcus melitensis, was first discovered in 1886 by D. Bruce. Over time, Bact was isolated from cows and pigs in 1906 and 1914. abortus bovis and Bact. abortus suis. In 1920, all pathogens were included in the Brucella group, and the disease was named brucellosis. The problem of brucellosis has remained relevant to agriculture and healthcare for many years. Its socio-economic significance is determined by the characteristics of the course of this disease, as well as by the main contingent of the lesion, namely the working population, which is determined by both professional and social factors. One of the most striking clinical features of modern brucellosis is the presence of a pronounced tendency for the disease to become chronic with subsequent disability.
The causative agent of brucellosis belongs to the genus Brucella. Brucella has several types:
- Br. melitensis,
- Br. abortus
- Br. suis,
- Br. canis
- Br. ovis,
- Br. neotomae,
- Br. pinnipediae
- Br. cetaceae
The main hosts of Br. melitensis are sheep and goats. For Br. abortus is cattle, for Br. suis - pigs. The main host of Br. canis are dogs. Br. pinnipediae and Br. cetaceae are found in marine mammals; Isolated cases of the disease with a predominance of lesions of the nervous system have been described in humans. Two more species of Brucella (Br. Ovis and Br. Neotomae) are not pathogenic to humans.
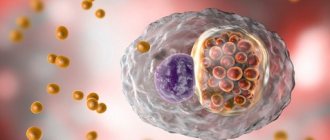
Brucella are gram-negative bacteria of small size, characterized by significant polymorphism (both rod-shaped and coccoid variants can be found in one preparation), do not form spores, are nonmotile, and are classified as intracellular parasites. They grow on many nutrient media, but very slowly (up to 3 weeks). Most laboratory animals (guinea pigs, rats, mice) are highly susceptible to Brucella. They are characterized by significant variability and the ability to transition from the S-form to the R- and L-forms. Resistant to external influences. They last for more than 1 month in water, for 2 months in feta cheese, and for up to 4 months in wool. They die quickly when boiled and exposed to disinfectants. Sensitive to antibiotics of the tetracycline group, streptomycin, rifampicin, fluoroquinolones, macrolides.
The main source of infection for humans is cattle and cattle, as well as pigs. A characteristic clinical sign of brucellosis in farm animals is abortion. The fetus, membranes, and amniotic fluid contain the causative agent of brucellosis in huge quantities. In animals that have had an abortion, Brucella can be detected within 15 months in pathological discharge from the birth canal, in milk, urine and feces. With secretions, pathogens get outside, contaminate bedding, food, and water in watering places, which causes other animals to become infected, which causes the occurrence of epizootic outbreaks.
Infection of people occurs through contact and nutritional routes . Infection by contact occurs especially often when amniotic fluid comes into contact with the skin (during calving, when caring for newborn calves, lambs). The highest incidence is observed among persons who have close contact with animals sick with brucellosis (shepherds, shepherds, veterinarians, livestock specialists). You can also become infected when processing raw meat, skin, and wool from animals with brucellosis (workers of meat processing plants, enterprises where wool is processed). Brunella penetrates through small breaks in the skin. Raw dairy products, sheep cheese, kumiss, etc. are dangerous.
Milk is the cause of infection for many people who are not professionally involved in animal husbandry. In this case, infection occurs through the mucous membrane of the mouth and throat, and not the stomach and intestines, since gastric juice has a detrimental effect on Brucella. Basically, brucellosis in humans is an occupational disease.
Once in the human body, Brucella does not leave any significant changes at the site of introduction. The first phase of regional infection, when Brucella reaches the lymph nodes through the lymphatic tract, corresponds to the incubation period. Reproduction and accumulation of Brucella occurs mainly in the lymph nodes.
In acute brucellosis, the clinical picture corresponds to primary bacteremia (hematogenous introduction). Subacute brucellosis is characterized by repeated and multiple bacteremia with signs of sensitization. With the bloodstream, the pathogen enters the organs of the mononuclear phagocyte system (liver, spleen, bone marrow), where new foci of infection are formed with the pathogen re-entering the blood, which determines the appearance of fever and general intoxication syndrome.
In chronic brucellosis, the pathogen enters various organs and systems (central nervous system, reproductive system, musculoskeletal system). Brucellosis is characterized by an allergic restructuring of the body - a pronounced delayed-type hypersensitivity persists for a long time even after the body is freed from the pathogen.
It should be noted that the transition from acute to chronic brucellosis is completely optional, and the development of chronic brucellosis is not always preceded by acute brucellosis. The duration of the disease with brucellosis does not exceed 2-3 years. Subsequently, as a result of sclerotic changes in organs and tissues, clinical manifestations (residual brucellosis) are observed.
The long-term recurrent course of the disease over years is associated with reinfection. The manifestations of the disease are significantly influenced by the type of Brucella that caused the disease. Pathomorphological changes in brucellosis are polymorphic. Changes are predominantly found in the connective tissue of various organs; their nature and severity depend on the stage of development of the pathological process. In the acute stage, exudative-inflammatory changes of a serous nature occur in the lymph nodes and internal organs (liver, spleen). Infectious-reactive vasculitis develops. In the subacute and chronic stages, productive-inflammatory changes predominate with the formation of specific brucellosis granulomas, mainly in the musculoskeletal system, nervous and reproductive systems.
Brucellosis is characterized by polymorphism of clinical manifestations. Therefore, many clinical classifications have been proposed. According to the most successful clinical classification, the following variants of the course of brucellosis are distinguished:
- subclinical,
- spicy,
- subacute,
- chronic,
- residual.
The subclinical course is characterized by a satisfactory condition of patients. Upon careful examination, mild enlargement of the peripheral lymph nodes may be detected in some individuals. This course is often characteristic of brucellosis caused by Bg. abortus.
The acute version of the course develops after an incubation period lasting from 1 week to 2 months. The disease begins with an increase in body temperature to high numbers. This course is typical for brucellosis caused by Br. melitensis. The temperature curve can be of different types: wavy, relapsing, and in some patients low-grade. An increase in body temperature is accompanied by chills and severe sweating. It is noteworthy that even if the patient has a high fever, his general condition is better than what happens with other infections (influenza, typhoid fever, etc.). Patients tolerate high body temperature satisfactorily, one might even say relatively well. There are no other signs of intoxication. By the end of the 1st week, an enlarged liver and spleen and generalized lymphadenopathy are detected (lymph nodes are moderately enlarged, some of them are sensitive to palpation). The main symptom at this stage is the absence of clear focal changes. Acute brucellosis can occasionally end in recovery, but, as a rule, it develops into subacute and chronic processes.
In the subacute version of the course of brucellosis, in addition to moderate symptoms of intoxication and attacks of moderate fever, focal lesions appear in the form of arthritis, plexitis, neuritis, lesions of the gonads, etc. A characteristic early symptom of damage to the musculoskeletal system is considered to be a pathological process in the sacroiliac joints. Asymmetrical arthritis is also possible in other joints. Most often, neuritis of the sciatic nerve occurs. Neuritis and plexitis are also characterized by asymmetrical lesions. Orchitis, orchiepididymitis, and adnexitis occur very often.
The chronic version of the course in some cases develops immediately, bypassing the acute stage, in other cases, signs of chronic brucellosis appear some time after the acute version. Chronic brucellosis is characterized by the involvement of more and more new organs and systems in the pathological process. Symptoms of general intoxication fade into the background. Body temperature is often low-grade or normal for weeks and months (remission period). Patients complain of increased irritability, depressive symptoms, poor sleep, asthenia, and decreased performance. Lymph nodes may be enlarged, including deep ones (mediastinal, mesenteric). When the mesenteric lymph nodes are enlarged, patients complain of pain along the intestines; if the nerve plexuses are damaged (solaritis), they complain of pain in the epigastric region. Damage to the musculoskeletal system is a common manifestation of chronic brucellosis. Patients complain of pain in muscles and joints.
In the clinical picture of the consequences of brucellosis (residual brucellosis), the first place is occupied by complaints of increased fatigue, general weakness, and irritability. Patients are concerned about sleep disturbances, memory loss, increased sweating, vascular disorders - cold extremities, rapid formation of bruises. At this stage, the pathogen is no longer in the patient’s body.
Risk factors
In the United States, brucellosis is more common in men. Usually these are people who work or have once worked in the livestock sector. The disease is rare in children.
Risk factors for developing brucellosis include:
- Consumption of unpasteurized dairy products, including cheeses called “country”, especially those brought from endemic regions (Mediterranean)
- Travel or business trips to areas with high incidence
- Working in a meat processing plant or slaughterhouse
- Working in agriculture, living in rural areas
Also at high risk are veterinarians working with brucellosis vaccines and hunters.
How to treat brucellosis?
The choice of strategy in the treatment of brucellosis is determined by the form of the disease. In acute forms of brucellosis, it is necessary to prescribe antibiotics in fairly high course doses. Insufficient doses and premature discontinuation of drugs cause the development of chronic brucellosis. WHO currently recommends the simultaneous use of doxycycline 0.1 g per day in adults in combination with rifampicin 0.6-0.9 g per day for 6 weeks. It is possible to prescribe doxycycline 0.1 g per day for 6 weeks in combination with streptomycin 1 g per day intramuscularly for 2-3 weeks. The latter option of antibiotic therapy is considered effective in preventing relapse; it is possible to replace doxycycline with ciprofloxacin or streptomycin with gentamicin or amikacin in appropriate doses.
Complex therapy for brucellosis does not exclude relapses of the disease. Relapses often occur 7-8 months later, and sometimes 1-2 years after the course of treatment.
Pathogenetic therapy is also carried out, which includes the use of detoxifying and anti-inflammatory drugs. For severe inflammatory changes (orchitis, neuritis, etc.), GCS is prescribed for 2-3 weeks.
In chronic forms, the use of antibiotics is justified only in the presence of fever. The most effective is vaccine therapy, which not only provides a desensitizing effect, but also stimulates immunogenesis. The vaccine is administered subcutaneously, intramuscularly, intravenously. The method of administration, as well as the dose of the vaccine, is determined in each case individually.
To stimulate the body's resistance, methyluracil, sodium nucleinate and other drugs are used, physiotherapy is carried out: electrophoresis, paraffin baths, therapeutic exercises, therapeutic massage, hydrogen sulfide and radon baths, mud therapy.
Medicines
Photo: img.thedailybeast.com
The most commonly used antibacterial drugs are:
- doxycycline. The drug is active against gram-positive and gram-negative microflora. Penetrates well into most internal organs and tissues of the body, but is not able to penetrate the blood-brain barrier. While taking doxycycline, the following side effects may develop: tinnitus, nausea, vomiting, stool upset, arthralgia, myalgia, and so on;
- ofloxacin. The drug affects the synthesis of the cell wall of the microorganism, thereby achieving a bacteriostatic effect. While taking this drug, side effects such as headache, dizziness, sleep disturbance, blurred vision, ringing in the ears, hearing loss, periodic cough, and palpitations may occur. It is also worth noting that while taking ofloxacin, it is recommended to avoid prolonged exposure to the sun, as there is increased sensitivity to sunlight, which can lead to burns;
- rifampicin. This drug is a broad-spectrum antibiotic, that is, it affects both gram-positive and gram-negative microflora and has a bactericidal effect. While taking rifampicin, in some cases the following side effects occur: headache, blurred vision, ataxia, oral candidiasis, nausea, vomiting, abdominal pain, diarrhea, menstrual irregularities.
In most cases, it is not monotherapy that is used, but a combination of rifampicin with doxycycline or ofloxacin.
As is known, nonsteroidal anti-inflammatory drugs (NSAIDs) have antipyretic, analgesic and anti-inflammatory effects, which play an important role in the treatment of brucellosis. To eliminate existing fever, drugs from the group of NSAIDs are used, which have a pronounced antipyretic effect, for example, paracetamol, ibuprofen and others. In the presence of pain, it is rational to prescribe painkillers (analgin, ketorolac, diclofenac). It is worth noting that long-term use of non-steroidal anti-inflammatory drugs can lead to the development of problems with the gastrointestinal tract, which is why it is important to carefully follow all the recommendations of your doctor and not adjust the dosage of the drug and duration of use yourself.
If there are symptoms of joint damage, glucocorticosteroids, which have a pronounced anti-inflammatory effect, can be prescribed. In most cases, prednisolone is preferred. The form of administration of the drug and its dosage are determined by the doctor strictly individually. In addition, you should remember about the side effects that occur while taking glucocorticosteroids (increased blood pressure, suppression of the immune system, increased blood glucose levels, development of osteoporosis), which often develop with long-term use of the drug.
Immunostimulating agents are used to enhance the body's protective properties, which is especially important for chronic brucellosis.
What diseases can it be associated with?
Brucellosis is an infectious disease against which various organ lesions develop:
- myositis - during palpation, painful areas are often identified in the muscles of the extremities; compactions are felt in the thickness of the muscles. Nodules or cords can be found in the subcutaneous fatty tissue of the lumbosacral, femoral and other areas. These are so-called fibrositis, resulting from inflammatory irritation of connective tissue;
- fibrositis - the size of fibrositis varies (from a pea to a bean, in some patients they have a diameter of 5 to 10 cm). With brucellosis, only one joint is very rarely involved in the pathological process. Large joints are predominantly affected (shoulder, knee, ankle-tibia). The function of the joints is limited due to pain, but the configuration changes little;
- bursitis - most often of the elbow joints, tendovaginitis, arthrosis-arthritis. Gradually, patients may develop ankylosis and contractures. Movements in the joints are significantly limited or completely absent; joints are enlarged and deformed. Damage to the iliosacral joints and spine is considered typical;
- sacroiliitis is a rare disease for which a number of diagnostic criteria are used. Eriksson's symptom is informative, the essence of which is that the patient is placed on a dressing table and the iliac crest is pressed in a lateral position or the anterior superior iliac crests are compressed with both hands in a supine position. With unilateral sacroiliitis, pain occurs on the affected side, with bilateral sacroiliitis, pain appears on both sides. The Nakhlas symptom is also used: the patient is placed on his stomach and the legs are bent at the knee joints. When lifting a limb, pain appears in the affected iliosacral joint;
- lesions of the peripheral nervous system (radiculitis, neuritis), the autonomic nervous system in the form of adynamia, sweating;
- psychoses - last a long time, with exacerbations;
- from the cardiovascular system - vasculitis, heart rhythm disturbances.
- lesions of the genital organs: in men - orchitis, epididymitis, decreased sexual function (orchitis is often unilateral, accompanied by severe pain and significant enlargement of the testicle); in women - adnexitis, salpingitis, endometritis, premature birth, spontaneous abortion, infertility are possible.
Complications
Brucellosis can affect almost any part of the patient's body, including the reproductive system, liver, heart and central nervous system. Possible complications include:
- Endocarditis. This is one of the most serious conditions that can lead to disruption of the heart valves. Endocarditis is the main cause of death in patients with brucellosis;
- Arthritis. A joint infection is characterized by pain, stiffness, and swelling in the affected area (usually the knees, ankles, hips, wrists, and spine);
- Infectious inflammation of the testicles (epididymo-orchitis). Brucella can invade the epididymis, the tube connecting the vas deferens and the testes. From there, the infection can spread further into the testicles, causing swelling and pain;
- Infectious inflammation of the liver and spleen. With the development of this complication, the patient experiences an increase in these organs in size and pain in the epigastric area;
- Infections of the central nervous system: meningitis (inflammation of the membranes surrounding the brain) and encephalitis (inflammation of the brain itself).
Brucellosis in pregnant women can cause miscarriage and fetal development abnormalities.
Deaths from brucellosis are rarely reported. Most of them are the result of cardiac dysfunction after the development of endocarditis.
Treating brucellosis at home
Treatment of brucellosis at home is inferior in effectiveness to measures used in a hospital. Therefore, the acute form of brucellosis requires hospitalization; relapse or chronic brucellosis can be treated at home, but under the close supervision of a physician, and if necessary, outpatient treatment, visits to clinics, and special infectious diseases departments are indicated. Under no circumstances should you self-medicate, adjust the dosages of medications prescribed by the doctor, or change the duration of the course of treatment.
Prevention of brucellosis is aimed at reducing the incidence among farm animals. The basis of prevention should be a set of sanitary and veterinary measures. When working with sick animals, use protective clothing and disinfectants.
A live anti-brucellosis vaccine has been developed, but immunization with this vaccine provides only short-term immunity. A vaccine based on the Bg strain. abortus is used exclusively for vaccination of farm animals. The administration of a live anti-brucellosis vaccine to a person should be treated with great caution, since after vaccination, patients often complain of deterioration in health, which is manifested by arthralgia, neuralgia, and lymphadenopathy. Today, scientists are working on the creation of chemical and inactivated corpuscular vaccines against brucellosis.
Features of bacteria
The causative agents of the disease are gram-negative bacteria of the genus Brucella. The parasite lives inside the cell. These microorganisms have a high survival rate and are quite pathogenic. They are classified as aerobic because they require oxygen to survive. In the absence of CO2, bacteria stop growing and reproducing. Under ideal conditions, the development of microorganisms occurs in 2-4 weeks.
Bacteria have the ability to suppress phagocytosis, which makes them invulnerable to antibacterial drugs and antibodies. Even if brucellae lose their cell wall, their pathogenicity remains, and they are able to attack the body when favorable conditions occur. This parasite has a high ability to penetrate into the intracellular space of phagocytes and lymphocytes - this causes disturbances in the functioning of the body’s immune system.
A secondary infection occurs, affecting internal organs, and brucellosis itself takes a chronic course. Brucella secretes endotoxin, which is accompanied by corresponding reactions of the sick animal or person. Under the influence of microorganisms in tissues, the structure of connective cells is disrupted, which leads to malfunctions of various organs.
What drugs are used to treat brucellosis?
- Doxycycline - 0.1 g per day for 6 weeks in combination with rifampicin or streptomycin;
- Rifampicin - 0.6-0.9 g per day for 6 weeks;
- Streptomycin - 1 g per day intramuscularly for 2-3 weeks;
- Ciprofloxacin - as an alternative to doxycycline (in combination with streptomycin).
Can you get infected from your dog?
Dogs can become carriers of B. canis. There are several confirmed cases where symptoms characteristic of brucellosis developed in owners of infected dogs, but the course of the disease in these cases was not severe and the patients were quickly cured without serious consequences.
It is very difficult to become infected with brucellosis from a dog, since the main route of infection is food. The only exception is veterinarians who are constantly in contact with biological fluids of animals (blood, saliva).
Treatment of brucellosis with traditional methods
Treatment of brucellosis with folk remedies demonstrates questionable effectiveness and is unlikely to be able to overcome the infection without combination with pharmaceuticals. At the same time, in the treatment of recurrent forms of brucellosis or its relapses, it is possible to use the following herbal preparations, each of which would be useful to discuss with your doctor:
- combine one tablespoon of stinging nettle leaves, black elderberry flowers, willow bark, garden parsley root, pour in half a liter of water, strain after 30 minutes; take a hot glass of infusion every two hours;
- connect 4 tbsp. spoons of birch leaves, 1 tbsp. alder buckthorn leaves, 5 tbsp. spoons of willow bark, 3 tbsp. pour the resulting collection with a liter of boiling water, simmer over low heat for 20 minutes, strain; Take the decoction hot, take a glass every two hours;
- combine 1 tbsp. stinging nettle leaves, black elderberry flowers, bean pods, 1 tbsp. pour half a liter of boiling water over the resulting collection, leave for 45 minutes, strain; Take half a glass of infusion several times a day.
Persistence and spread
Brucella lasts for a long time in the cold, but does not tolerate boiling, which kills the bacteria instantly. It takes about 30 minutes for parasites to die at a temperature of 60 degrees. They are also sensitive to disinfectants. Food products retain brucella for the following time:
- kefir - 11 days;
- salted meat - up to 30 days;
- milk - up to 40 days;
- feta cheese - up to 2 months;
- butter - up to 5 months;
- hard cheese - up to 1 year.
Bacteria can live in animal fur for up to 4 months, and in water for up to 2 months. Up to half a million cases of brucellosis are detected annually in the world. Areas with developed livestock farming are considered potentially dangerous. In Russia, these are Dagestan, the Southern Urals, Krasnodar Territory and some other areas. Susceptibility to the disease does not depend on gender and age and is considered high. For infection to occur, one or several dozen microbial bodies are sufficient.
Treatment of other diseases starting with the letter - b
| Treatment of Graves' disease |
| Treatment of bacterial vaginosis |
| Treatment of balanoposthitis |
| Treatment of bartholinitis |
| Treatment of rabies |
| Treatment of biliary cirrhosis |
| Treatment of amyotrophic lateral sclerosis |
| Treatment of Alzheimer's disease |
| Treatment of ankylosing spondylitis |
| Treatment of Wilson-Konovalov disease |
| Treatment of Koenig's disease of the knee joint |
| Treatment of Crohn's disease |
| Lyme disease treatment |
| Treatment of Parkinson's disease |
| Treatment of Peyronie's disease |
| Treatment of Fabry disease |
| Treatment of warts |
| Treatment of botulism |
| Treatment of bronchial asthma |
| Treatment of bronchitis |
| Treatment of bronchiectasis |
| Treatment of typhoid fever |
| Treatment of knee bursitis |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.