Lymphoma is a cancer that affects lymphocytes (cells of the immune system). In some cases, it may be called cancer of the lymphatic system, but this is a misnomer, since cancer refers to tumors originating from epithelial tissues, and the term lymphoma is used for malignant neoplasms of the lymphatic system. There are many types of lymphoma, and their treatment depends on the type of disease, stage, response to previous therapy, if any, the patient's age and general health. That is, the approach can range from simple observation to high-dose chemotherapy and hematopoietic stem cell transplantation.
Types of lymphomas
All lymphomas are divided into two large groups - Hodgkin and non-Hodgkin. Hodgkin's lymphomas are characterized by the presence of special Berezovsky-Sternberg cells in the tumor tissue. Non-Hodgkin's lymphomas are a very heterogeneous group of tumors that are also divided into two large subgroups - T-cell and B-cell.
Based on the nature of their course, non-Hodgkin lymphomas are divided into the following types:
- Benign lymphomas, or indolent. They progress very slowly, but are very difficult to radically cure.
- Aggressive lymphomas. In this case, the disease inevitably progresses and, if left untreated, leads to the death of the patient. For such lymphomas, chemotherapy is mandatory.
- Super-aggressive forms. With such tumors, in the absence of treatment, the disease progresses very quickly and malignant cells spread almost like lightning throughout the body. Death may occur within several months or even weeks after the development of the disease. To defeat the disease, radical measures are needed, for example, high-dose chemotherapy with stem cell transplantation.
Folk remedies
Photo: wedding-dream.pl
A diagnosis such as lymphoma requires exclusively medical care. It is important to understand that without appropriate treatment, the disease will not miraculously disappear, but will only worsen. Therefore, in no case should you rely on various folk recipes that can “cure” cancer.
Traditional medicine can be used, for example, for nausea, which is a common side effect of radiation and chemotherapy. In this case, you can prepare a decoction of mint. To prepare it, you will need a large spoon of mint leaves, which are poured with one glass of boiling water and infused. You should drink 1 tablespoon three times a day. Melissa, which is also infused, has a good effect, after which it is ready for use. Many people use a decoction of dill seeds. To prepare it, you need to take a teaspoon of seeds and pour boiling water over it, let the broth sit for about 15 minutes, after which it is ready for use.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Symptoms of lymphoma
Signs of lymphoma can be very diverse, but they can all be combined into three large groups:
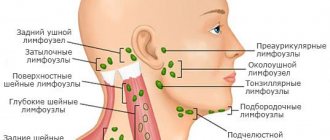
- Lymphadenopathy, or enlarged lymph nodes. Quite often there are situations where the first symptoms of lymphoma are painless enlargement of the lymph nodes. In this case, the patient consults a doctor and the diagnosis is established quite quickly. However, there are cases when lymphadenopathy affects internal lymph nodes that are not accessible to palpation or inspection. They can only be detected using ultrasound, CT or MRI and then this sign may not be detected.
- B-symptoms are a triad of symptoms that are the most specific sign of lymphoma. These include night sweats (sweating can be very severe, to the point that the patient wakes up on a pillow wet with sweat), unexplained weight loss and fever not associated with an infectious disease.
- Symptoms that develop when lymphoma spreads beyond the lymphatic system and spreads to internal organs. If the central nervous system is involved, this may include headaches, vomiting, and changes in vision. If the lungs are involved - cough, shortness of breath. Thus, the symptoms will depend on which organs or systems are affected.
Development in children
Newborns and children under 4 years of age usually do not develop this type of lymphatic cancer. The most common age of those affected is on average 14 years. But about 4 percent of primary and school-age children still get sick.
Children do not feel the onset of the disease. But later the following signs may appear:
- The child often gets tired, becomes lethargic and indifferent to everything.
- You may notice enlarged lymph nodes in the neck or groin, which do not go away for a long time.
- The child is rapidly losing weight and eats little.
- Symptoms of itchy dermatosis will appear.
- Fluctuations in body temperature, appearing and then disappearing again.
- There may be heavy sweating, especially at night.
- All this does not bother the child. However, later, very slowly, the symptoms increase, changes begin in the liver and spleen.
Attention! In children under three years of age, the lymph nodes are always slightly enlarged. They are also always increased in ARVI and other infectious diseases. Therefore, only a doctor can distinguish one disease from another.
If the doctor suspects lymphogranulomatosis, the child is given the same diagnosis as an adult . And if concerns are confirmed, they are sent to a hospital.
Methods for diagnosing lymphoma
There are no screening tests to diagnose lymphoma. Typically, the diagnosis is established based on the results of an examination that the doctor prescribes for the patient after he has presented with complaints of symptoms of a “viral infection.”
Blood tests and lymph node biopsy (carried out in different ways: using a needle, removing the entire lymph node or part of it) help to establish the correct diagnosis. In some cases, a red bone marrow biopsy is required.
Lesions can be detected using CT, MRI, ultrasound, and positron emission tomography (PET).
Leading clinics in Israel
Assuta
Israel, Tel Aviv
Ikhilov
Israel, Tel Aviv
Hadassah
Israel, Jerusalem
In medical practice, there are five types of Hodgkin lymphoma, four of which are included in the group called “classical lymphogranulomatosis”:
- Nodular category with lymphoid dominance. Of the total number of forms of this disease, this type of Hodgkin lymphoma accounts for 5% of patients. The predominant category consists of young men and those over forty years old. A distinctive feature of this type of Hodgkin lymphoma from classic lymphogranulomatosis is the histological picture and course of the disease. The affected area is the lymph nodes in the armpits, neck and, less commonly, the groin. With this form, the clinical course of the disease is weak, with periodic relapses, but negative development of the disease and unfavorable outcome are extremely rare (5%);
- Classic lymphogranulomatosis includes:
- Classic Hodgkin's lymphoma with an excess of lymphocytes (lymphoid predominance). With this form, a reduced number of Reed-Sternberg cells and an increased number of B-lymphocytes (cells that secrete antibodies and provide immunity) are observed. The number of annual diseases with the classic type of Hodgkin lymphoma is 95%. People with acute viral disease and human immunodeficiency virus are especially susceptible to the disease. The predominant location of lesions is in the lymph nodes: mesenteric, mediastinal, neck, axillary, groin, retroperitoneal space;
- Nodular Hodgkin's lymphoma (a variant of nodular sclerosis). This form occurs in 65% of people, with localization of the formation in the middle part of the chest (heart, aorta, bronchi), affecting the lymph nodes and thymus gland. As a result, 20% of patients suffer from damage to the spleen with further spread to the liver and bone marrow. This type of development of Hodgkin's lymphoma has a slow course, in which it affects: at stage I, groups of lymph nodes and lymphoid tissue, at stage II - several groups of nodes and one side of the diaphragm, at stage III - the lymphoid structure on both sides of the diaphragm, at stage IV - the liver and Bone marrow. Sclerosing nodular Hodgkin lymphoma is characterized by such symptoms as: increased sweating at night, chills and weight loss;
- Hodgkin's lymphoma of mixed cell type. Identification of this type of disease is carried out by diagnosing the cells that form the follicles. With a sluggish nature, lymphogranulomatosis can appear several years after diagnosis, however, it happens that lymphadenopathy has transient manifestations, which requires immediate treatment. Practice shows that the follicular form of Hodgkin's lymphoma, which by its nature has a low probability of developing into malignant neoplasia, has recently increasingly transformed into a heterogeneous abnormal cellular lymphoma of enormous size. Treatment, as a rule, leads to long-term remission and significantly increases the chances of recovery;
- Hodgkin's lymphoma with lymphocyte deficiency (lymphoid depletion) is the rarest form of the disease in question (5%) and is observed mainly in patients over the age of 50 years. The tumor consists predominantly of Rydsternberg cells with small streaks of lymphocytes.
Treatment of Hodgkin's lymphoma in Moscow and Krasnodar
For Hodgkin's lymphoma in the early stages, treatment is carried out according to the ABVD regimen. This is a combination of chemotherapy drugs:
- adriamycin (doxorubicin),
- bleomycin,
- vinblastine
- dacarbazine.
All of them are administered using a dropper. Each course takes 4 weeks. The patient may require 4–6 courses, meaning treatment for lymphoma will last 4–6 months.
Chemotherapy according to the ABCD regimen leads to immunodeficiency and susceptibility to infections, fatigue, weakness, multiple bruises, skin reactions (redness, darkening, etc.), hair loss, infertility, sensitivity to light, etc. In addition to chemotherapy, patients with Hodgkin lymphoma must radiation therapy is needed.
The prognosis in the early stages is good; many people manage to go into long-term remission, that is, essentially recover. Only a doctor who takes into account the patient’s age, hemoglobin levels, lymphocytes, albumin, etc. can give a more accurate forecast.
At stages III–IV (they are called late), a different chemotherapy regimen is needed. It's called BEACOPP . These are bleomycin, etoposide, doxorubicin, cyclophosphamide, vincristine, procarbazine and prednisolone. Some of these drugs are taken in the form of capsules and tablets, while others are administered through a dropper.
Side effects from BEACOPP are quite common for chemotherapy: decreased immunity, fatigue, weakness, shortness of breath, hair loss, multiple bruises, nosebleeds, infertility, etc. One course lasts 3 weeks, the patient may need up to 8 courses, which will take a total of six months . Radiation therapy in this case is not always necessary - it is carried out only if the full effect of chemotherapy has not been achieved and there are residual formations. The prognosis for stage III–IV Hodgkin lymphoma depends on the same factors as in the early stages.
Unfortunately, due to the toxicity of the drugs used, the consequences of treatment (malignant neoplasms, heart disease, etc.) may appear years later.
According to statistics, the disease can return in 10-15 percent of patients who initially had Hodgkin lymphoma in the early stages, and in 20-40 percent in the later stages. Also, 10–15 percent of patients will be resistant to first-line chemotherapy (the one given first). In all these cases, second-line chemotherapy is quite effective. It can be different:
- GEM-P (gemcitabine, cisplatin, methylprednisolone);
- GDP (gemcitabine, dexamethasone, cisplatin);
- GVD (gemcitabine, vinorelbine, pegylated liposomal doxorubicin);
- IGEV (ifosfamide, mesna, gemcitabine, vinorelbine, prednisolone);
- mini-BEAM (carmustine, etoposide, cytarabine, melphalan);
- ESHAP (etoposide, steroid, cytarabine, cisplatin);
- ICE (ifosfamide, carboplatin, etoposide);
- DHAP (dexamethasone, cytarabine, cisplatin).
Unfortunately, until now there have not been enough studies to answer the question: which of these treatment regimens is most effective. Usually two courses of this chemotherapy are sufficient, but some patients require longer treatment.
If the lymphoma is localized, that is, the affected area is limited, then radiation therapy is also performed.
After this course of treatment, the patient undergoes high-dose chemotherapy and autologous transplantation of hematopoietic stem cells (pre-selected own bone marrow cells, from which all blood cells are formed). After this, 40–60 percent go into remission. The chances are higher for those who have had a good response to second-line therapy.
If a relapse occurs after transplantation of your own cells, then there are two options:
A) palliative care, that is, improving the quality of life, but not leading to recovery;
B) high-dose chemotherapy and transplantation of hematopoietic stem cells from a donor.
In the West, some monoclonal antibodies are also used (for example, brentuximab vedotin). However, these drugs are not registered in Russia. The choice in favor of one or another type of treatment is made depending on the general condition of the person and the aggressiveness of the disease.
Get a treatment program
Forecast
Malignant granuloma responds well to treatment and a person can completely get rid of this disease. The main thing is to detect the disease in time. Then the chances are high - more than 85 percent of patients diagnosed with Hodgkin lymphoma are completely cured .
The forecast depends on several factors:
- Stage of the disease. Patients with stage 2 achieve remission in 90 percent of cases. From 3-4 – in 80 percent.
- Presence of metastases . Many organs and systems can be affected in such a way that their recovery is no longer possible.
- Risk of relapse . After treatment, the disease may return in 15 to 25 percent of patients. In this case, the prognosis is disappointing.
- Sometimes Hodgkin's disease simply does not respond to any type of therapy. However, this is rare.
If you do encounter this disease, do not think about how long people with Hodgkin lymphoma live. With successful treatment, life expectancy will not decrease.
Pregnancy and Hodgkin's lymphoma
Of course, during treatment for Hodgkin's lymphoma, a woman should take precautions to avoid becoming pregnant. However, if the disease was diagnosed when she was already expecting a child, then the decision on further treatment is made based on the severity of her condition. If lymphoma is found during the first trimester, then it is better to postpone treatment at least until the second or third, since chemotherapy is quite toxic, and in the first trimester it can have a particularly bad effect on the development of the fetus and cause various defects. In the future, at 32–36 weeks, labor can be induced to begin treatment faster.
If the disease right now threatens the health and life of the mother, then combination chemotherapy ABVD (doxorubicin, bleomycin, vinblastine and dacarbazine) is used in any trimester. As a last resort, radiation therapy is used, but only above the diaphragm. What risks does such treatment pose to a child in the second and third trimesters? Low weight, intrauterine growth restriction, premature birth, stillbirth, mental retardation and learning disabilities. Steroids may be used along with chemotherapy to reduce the toxicity of the drugs and speed up the development of the baby's lungs, making premature birth less dangerous.
If Hodgkin's lymphoma recurred during pregnancy and was not discovered for the first time, then it is better to have an abortion, and then undergo high-dose chemotherapy and hematopoietic stem cell transplantation.
Radiation therapy
The final stage of treatment for Hodgkin lymphoma is irradiation of all affected areas of the lymph nodes. As a rule, radiation therapy begins 2 weeks after the end of drug therapy when blood counts are normalized.
The radiation dose depends on the completeness of remission after drug therapy: upon achieving complete remission (disappearance of all clinical and radiological signs of the disease) in the lymphatic zone, according to PET-CT data, the radiation dose is 20 Gy. If the size of the tumor after polychemotherapy has decreased by 75% or more from the original tumor and/or there is a decrease in radiopharmaceutical hyperfixation according to PET-CT to 2-3 according to Deauville, then the radiation dose is 25 Gy. If tumor formations are reduced by less than 75% and/or radiopharmaceutical hyperfixation persists according to PET-CT 4-5 according to Deauville, the radiation dose is increased to 30 Gy.
Fig. 5 Radiation treatment plan. Patient I., 4 years 6 months. Hodgkin's lymphoma stage II. with damage to the cervical, supraclavicular, subclavian lymph nodes on the left, the thymus gland, and the nasopharynx. Condition after 4 courses of PCT, remission. Irradiation of the cervical-supraclavicular lymph nodes on the left with a consolidating purpose, SOD 20 Gy.
Fig.6 Patient M., 11 years old. Hodgkin's lymphoma stage II. with damage to the soft tissues of the neck, lymph nodes of the neck. Condition after 2 courses of chemotherapy. According to the control PET/CT data, no metabolically significant lesions were identified, remission. Conducting radiation therapy of the primary involved areas with a total focal dose of 20.0 Gy for the purpose of consolidation.
Non-Hodgkin's lymphoma
Non-Hodgkin's lymphomas can be divided into three groups: indolent, aggressive and highly aggressive.
Indolent lymphomas
Indolent lymphomas progress slowly, and it is almost impossible to cure them completely: they constantly recur. The World Health Organization classifies the following diseases as indolent lymphomas:
- lymphocytic lymphoma;
- lymphoplasmacytic lymphoma (Waldenström macroglobulinemia);
- plasma cell myeloma (plasmocytoma);
- hairy cell leukemia;
- follicular lymphoma (stages I and II);
- B-cell marginal zone lymphoma;
- lymphoma from mantle cells (such lymphoma can be aggressive);
- T-cell leukemia of large granular lymphocytes;
- mycosis fungoides;
- T-cell prolymphocytic leukemia;
- NK cell leukemia of large granular lymphocytes.
If the doctor did a biopsy (took a tissue sample) of the lymph node and found that the lymphoma is indolent, then the lymph node is simply removed, and the patient periodically comes to the hematologist, talks about his symptoms, if any, undergoes an examination and takes tests. This tactic is called “watch and wait.”
Quite often, without treatment, a person may not feel sick for a long time (months or even years). Therefore, therapy is delayed until symptoms appear that impair quality of life.
Starting chemotherapy right away does not make much sense, since it will not increase life expectancy, but one line of therapy will already be used, and doctors have a limited number of them at their disposal. Therefore, for example, if indolent lymphoma is diagnosed during pregnancy, treatment can usually be delayed until after delivery.
When a person with indolent lymphoma goes into remission, they may be given the drug rituximab as maintenance therapy so they are more likely to relapse later.
Aggressive and highly aggressive lymphomas
Aggressive lymphomas are:
- follicular lymphoma (stage III);
- diffuse large B-cell lymphoma;
- lymphoma from mantle cells;
- peripheral T-cell lymphoma;
- anaplastic large cell lymphoma.
Highly aggressive lymphomas:
- Burkitt's lymphoma;
- B-lymphoblastic leukemia/lymphoma and B-cell precursors;
- T-cell leukemia/lymphoma;
- T-lymphoblastic leukemia/lymphoma from T-cell precursors.
If the lymphoma is aggressive or highly aggressive, it is best to start chemotherapy right away, even if the patient is pregnant. The treatment regimen for such lymphomas is approximately the same: first, several courses of chemotherapy are given, often with rituximab, and remission is achieved. Rituximab (MabThera) is a drug that came out in the late 1990s and has greatly improved survival in lymphomas. It belongs to a group of substances called monoclonal antibodies. They are made up of immune cells that recognize cancer cells, attach to them and block their growth or kill them.
Radiation therapy for aggressive lymphomas can be used if the affected area is limited. Then combination treatment gives better results than chemotherapy alone.
It is impossible to say how many people will avoid relapse, even if we talk about one type of lymphoma. Only a doctor can give a prognosis, having calculated everything taking into account the characteristics of a particular patient.
Get a treatment program
If remission ultimately cannot be achieved or if a relapse occurs, then second-line chemotherapy is used - with those drugs that have not yet been used, then high-dose chemotherapy and autologous transplantation of hematopoietic stem cells, that is, restoration of bone marrow killed by drugs using pre-saved own cells. As such, autologous transplantation does not have a curative function. It is needed only so that a person’s hematopoiesis is restored and he survives after such therapy. If after this the disease returns, then high-dose chemotherapy is carried out followed by an allogeneic transplantation of hematopoietic stem cells from a donor. The donor can be a brother or sister, if there is tissue compatibility with them, or a suitable person from the database of potential donors. Such transplantation also plays a therapeutic role. Hematopoietic stem cells form the human bone marrow, which ensures the functioning of the immune system. In other words, after such a transplantation, the patient’s immunity is no longer his own, but from the donor. And new lymphocytes destroy residual tumor cells. But at the same time, cells arising from donor hematopoietic stem cells can attack other organs of the patient - this graft-versus-host reaction is deadly. The doctor must recognize it as quickly as possible and begin treatment with hormones or cyclosporine, that is, immunosuppressive therapy - suppressing the immune system. Transplantation of donor hematopoietic stem cells is a last resort, as the mortality rate from such treatment is 30 percent.
If a relapse occurs after such a transplantation or if for some reason it cannot be carried out (for example, due to the person’s severe physical condition or old age - over 65 years old), then the patient receives maintenance treatment - tablet chemotherapy. These are standard cytostatics (drugs that block the division of tumor cells) in a small dose. It is also very important that the person receives palliative care: lymphoma in this situation can worsen the quality of life, so doctors fight the symptoms. For example, with pain, nausea, loss of appetite, shortness of breath, etc.
Active treatment for lymphoma may stop earlier, even after first-line therapy. This happens if, due to treatment, a person has a stroke, heart attack or other complication. Over time, some patients find it harder and harder to endure chemotherapy, the person recovers longer than necessary, and the lymphoma grows without treatment in time. Then the person is prescribed maintenance chemotherapy, which will not cure the disease, but will somewhat inhibit the growth of tumor cells.
Even before treatment, you need to discuss possible infertility with your doctor, since chemotherapy drugs can deprive a woman of the opportunity to become pregnant and a man to become the biological father of his child. Therefore, it is generally recommended that women freeze their eggs and men freeze their sperm. However, in Russia, women will have problems with this, since reproductive specialists usually have no experience in caring for patients with lymphoma, and they do not undertake to carry out hormonal stimulation of superovulation, which is necessary before retrieving a large number of eggs.
If, after treatment for lymphoma, you are in remission, the doctor will want to see you once every few months, then less and less often, as the likelihood of relapse decreases over time.
Causes
The reasons for the development of lymphogranulomatosis are not fully understood. There is a possibility that the disease is associated with the Epstein-Barr herpesvirus. The assumption of its involvement is based on special studies, according to which the virus gene is detected in 20% of biopsies.
Lymphoma often occurs due to a deficiency of the immune system (HIV)
According to statistics, regions with a high incidence of Hodgkin lymphoma include African countries, the USA, and Japan. It can occur at any age, but the peak of the disease occurs in two periods: from 15 to 35 years, or after 50 years. With the exception of children under 10 years of age, who are predominantly boys, the distribution of cases by gender is almost the same.
Lymphogranulomatosis in children accounts for almost 10% of the total number of cases. Hodgkin's lymphoma in adults over 50 years of age usually occurs with complications.
Risk factors for the disease:
- among the sick, 60-70% are men from 15 to 35 years old, or from 50 years old;
- burdened heredity: Cases of the disease occur three times more often in families where relatives have already had the disease, which suggests a genetic predisposition. However, children born to a sick mother do not develop the disease;
- conscious (for example, due to antitumor chemotherapy) or acquired (HIV) immunosuppression;
- Hodgkin's lymphoma in adults who work with radiation (eg, health care workers) or carcinogens.
Diffuse large B-cell lymphoma
This aggressive type of lymphoma is the most common among non-Hodgkin lymphomas. If the disease is detected early, most patients are better off with a shortened course of R-CHOP chemotherapy (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone). Radiation therapy is also necessary, but if it has the potential to worsen the quality of life in the future, it is better to do without it. If large cell lymphoma affects the testicle, epidural space (outside the dura mater of the spinal cord), or paranasal sinuses, the risk of damage to the central nervous system increases. Therefore, in such cases, it is necessary to carry out intrathecal chemotherapy, that is, inject the drug into the cerebrospinal fluid. Also, if the lymphoma has touched the testicle, it is necessary to remove it and irradiate this and the adjacent area.
In case of relapse or if the lymphoma is resistant to first-line therapy, it is recommended to use the GDP regimen (gemcitabine, dexamethasone, cisplatin). An alternative may be ICE (ifosfamide, carboplatin, etoposide) or DHAP (dexamethasone, high dose cytarabine, cisplatin). In all these cases, rituximab should also be added if it was not used the first time. This is followed by first high-dose chemotherapy and then autologous hematopoietic stem cell transplantation (BMT). If the disease returns after this, then the only option is allogeneic hematopoietic stem cell transplantation, that is, from a donor.
If for some reason TCM cannot be performed or a person does not respond to second-line therapy, then all he can do is fight the symptoms.
Criteria for assessing the completeness of remission
Criteria for assessing remission are needed by the doctor to determine the need to continue treatment or intensify therapy programs, or transfer the patient under dynamic observation.
- Complete remission - complete regression of all signs of the disease (clinical, hematological and other manifestations of the disease) according to imaging tests, determined twice with an interval of at least 4 weeks.
- Partial remission is a reduction in the size of tumor formations by at least 50% for a period of 4 weeks in the absence of new lesions.
- Stabilization of the disease is a reduction in the size of tumor formations by less than 50% or an increase in them by no more than 25% of the original volume in the absence of new lesions.
- Progression is the appearance of new lesions during treatment or an increase in previously existing ones by more than 25%, as well as the appearance of symptoms of intoxication.
- Relapse is the appearance of new lesions after achieving complete remission.
Peripheral T-cell lymphoma
This group of predominantly aggressive lymphomas is treated according to the standard regimen: first, combination chemotherapy is carried out - most often according to the CHOP regimen (cyclophosphamide, doxorubicin, vincristine and prednisone). If the patient is under 60 years of age, then etoposide is added to these drugs. Sometimes radiation therapy is also performed. If a relapse occurs later and the person responds to second-line chemotherapy, he may be eligible for a hematopoietic stem cell transplant. However, in the case of peripheral T-cell lymphoma, this approach is less likely to produce good results. If treatment for lymphoma does not help, the doctor will most likely prescribe supportive care, and palliative care will also be needed in the future.
Stages
Stage is the stage of development of a tumor neoplasm. All stages of lymphoma have specific characteristics that indicate how old the tumor is, how far the tumor process has spread, and to what extent the body is affected. Determining the stage helps doctors select the optimal treatment tactics and make a prognosis for the patient’s life. In total, the disease has four stages.
- The first stage is the initial one. During it, one lymph node is affected (less often several located in the same area, for example, cervical or inguinal lymph nodes). Also, a tumor that affects one organ and does not affect the lymph nodes belongs to the first stage. Such tumors are local; they do not metastasize to other human systems, tissues and organs.
- At stage 2, the tumor process affects two or more lymph nodes located on one side of the diaphragm, with which doctors “divide” the human body into two halves horizontally. At this stage, the clinical picture begins to appear more clearly, forcing the person to see a doctor and undergo an examination.
- In stage 3 lymphoma, the oncological process affects two or more lymph nodes, which are located on opposite sides of the diaphragm. It is also possible that several lymph nodes and one organ or tissue area may be affected. Stage 3 is characterized by severe symptoms.
- Stage 4 lymphoma is a disseminated tumor, that is, one that has spread massively throughout the body. The last and most severe degree can be spoken of when the tumor affects several organs located far from the primary site of the oncological process.
Treatment of follicular lymphoma
If the disease is detected at stages I–II, then such lymphoma is classified as indolent and, if necessary, is treated with radiation therapy. But the likelihood of the disease returning is extremely high.
If follicular lymphoma was first diagnosed at stage III–IV, it is recommended to be treated with rituximab in combination with chemotherapy. For example, according to the regimen R-CVP (rituximab, cyclophosphamide, vincristine and prednisone), R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone) or BR (bendamustine and rituximab). In some cases, the doctor may prescribe long-term use of rituximab after complex treatment.
But if, despite sensitivity to chemotherapy, a rapid relapse occurs, then a person who is able to withstand high-dose chemotherapy undergoes autologous hematopoietic stem cell transplantation. If this does not help, they resort to donor cell transplantation.
The prognosis for follicular lymphoma is determined by the special FLIPI index (Follicular Lymphoma International Prognostic Index). Risk factors such as the patient’s age over 60 years, elevated LDH levels, late stage of the disease (III–IV), decreased hemoglobin levels less than 120 g/l, and more than 5 areas of nodal lesions are taken into account. For each risk factor, 1 point is added. The survival prognosis depends on the score.
Possible complications
Lymphoma (symptoms in adults and children may not be suspicious at first) is a fatal disease. Without timely treatment and ignoring symptoms, it progresses, and eventually death occurs. Also, self-medication with folk remedies can greatly aggravate the picture.
It is possible to cure lymphoma if you start timely treatment and pay attention to the symptoms in both adults and children. However, it all depends on the person's immune system, age and response to treatment.
Article design: Oleg Lozinsky
Burkitt's lymphoma
After removing a lymph node containing tumor cells, a person with Burkitt's lymphoma must undergo 4-6 courses of chemotherapy to prevent progression of the disease and early relapse (up to a year). Treatment regimens commonly used are CODOX-M (cyclophosphamide, vincristine, doxorubicin, high-dose methotrexate) combined with IVAC (ifosfamide, cytarabine, etoposide, and methotrexate injected into the cerebrospinal fluid). Injecting the drug into the cerebrospinal fluid (intrathecal chemotherapy) is very important because Burkitt's lymphoma is fraught with complications in the central nervous system.
The CALGB 9251 protocol is also sometimes used. This is a highly toxic combination chemotherapy that causes a person to end up in the hospital for a long time. If the body cannot withstand such aggressive treatment for Burkitt's lymphoma, then the EPOCH regimen (etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin) with rituximab is used.
During treatment of Burkitt's lymphoma, tumor disintegration (lysis) syndrome often develops. This is a dangerous condition in which, due to the destruction of tumor cells, various substances enter the blood in large volumes, causing metabolic disorders and leading to kidney failure. To prevent this syndrome from occurring, you need constant monitoring by a competent specialist, active fluid infusion through a vein, as well as constant correction of electrolytic imbalance.
If Burkitt's lymphoma returns or is resistant to treatment, there are no treatment options other than clinical trials - the person is given palliative care to improve their quality of life.
Prevention
Lymphoma, symptoms in adults in which can occur for various reasons, will be avoided if you follow some recommendations and exclude these causes. Prevention will help reduce the risk of damage to the body to zero.
To exclude the possibility of lymphoma, you should:
- less contact with toxic substances;
- do not neglect contraceptives during sexual intercourse with a casual partner;
- undergoes a course of vitamin therapy at least 2 times a year;
- maintain hygiene (do not use other people’s toothbrushes or towels);
- exercise regularly (moderately, at least 10-15 minutes will be enough).
Special attention is paid to hygiene and sexual relations due to the possibility of infection with the Epstein-Barr virus.
Treatment of lymphoplasmacytic lymphoma
Lymphoplasmacytic lymphoma is an uncommon type of B-cell non-Hodgkin lymphoma. It got its name because, under a microscope, its cells resemble both lymphocytes and plasma cells. Most often it occurs in people over 60 years of age, it grows slowly, but sometimes there is rapid aggressive growth. For many patients, doctors adhere to active surveillance tactics. If signs of rapid growth appear, chemotherapy drugs in combination with prednisone and dexamethasone, targeted drugs, and immunotherapy are prescribed. In rare cases, for extranodal lesions, radiation therapy is used.
When to see a doctor
Of course, if fatigue and some other symptoms occur separately, you should not immediately attribute this to the onset of oncology. It is necessary to undergo tests in order to understand the cause of the malaise.
Before taking the tests, you need to prepare. A day before all procedures, a person eliminates alcohol and tobacco. The stomach should be empty. The time of the last meal is at least 12 hours. It is forbidden to drink tea, juices (natural and purchased), and chew chewing gum. Only drinking water is allowed.
Another important condition is that you should not worry before the procedures. Sometimes it is difficult to prevent absolutely all factors that provoke stress. The most common cause of anxiety is waiting for a bad test result.
If a person is taking any medications, the doctor should be informed.
If the diagnosis is confirmed, then the next person the patient is referred to is an oncologist. After the examination, therapy, diet and prognosis for recovery are prescribed.