Meningitis is characterized by inflammation of the meninges of the spinal cord and brain. The disease is classified as infectious. Meningitis affects adults and children. In children, meningitis often occurs in a fulminant or acute form. Adults are more likely to suffer from meningitis caused by meningococcal infection; women are sick less often than men.
The Yusupov Hospital diagnoses and treats meningitis. In the laboratory you can undergo a number of tests for the causative agent of the disease, and experienced doctors provide consultations in the hospital. Meningitis can have a fulminant course, in which case qualified assistance should be provided immediately. With meningitis, it is very important that the diagnosis be made in the first days of the disease.
Types of meningitis
It is generally accepted that Hippocrates was the first to describe the symptoms of meningitis, and then medieval healers. So humanity has known about this disease for a very long time. But for many years, tuberculosis and consumption were mistakenly believed to be the cause of inflammation of the meninges, and before the discovery of antibiotics, 95 out of 100 patients died from meningitis. Nowadays, treating meningitis is also not easy, but thanks to modern knowledge, the survival rate is much higher than several centuries ago.
However, for therapy to be effective, you first need to understand what type of meningitis you will have to fight. And this disease is very “many-sided” in origin and nature, therefore, in the international classification of diseases (ICD 10), each type is assigned its own code and definition, and specialists use different methods to systematize the disease.
According to the nature of inflammation, meningitis occurs:
- purulent;
- serous.
In the first case, the disease is caused by meningococcal bacteria, is very severe, and is caused by a primary septic process. The second type is of viral origin. This variety is considered not as dangerous as purulent and is less likely to cause complications.
By origin, meningitis is divided into:
- primary (independent disease);
- secondary (appears as a complication of sinusitis, otitis, respiratory infections, osteomyelitis of the skull bones, caries, boils on the face or neck, tonsillitis, and sometimes occurs against the background of diseases such as tuberculosis, measles, mumps, syphilis).
Classification by pathogen:
- bacterial;
- fungal;
- viral;
- protozoan;
- mixed.
According to the nature of the flow:
- lightning (fulminant);
- spicy;
- subacute;
- chronic;
- recurrent.
By localization of inflammation:
- total;
- basal (affects the deep parts of the brain);
- spinal (affects the spinal cord);
- convexital (affects the superficial brain).
According to severity:
- mild;
- medium heavy;
- heavy.
In addition, there is also non-infectious meningitis. This is a type of aseptic meningitis, that is, a disease caused by anything other than bacteria that usually causes acute meningitis - non-infectious diseases, drugs or vaccines. Overall, these causes of meningitis are uncommon. Most often, doctors diagnose cases of viral, bacterial, secondary purulent and fungal meningitis. Moreover, the bacterial (meningococcal) variety of the disease is more common among children under 5 years of age, and the fungal type is more common among pregnant women, patients after chemotherapy, and patients with acquired immunodeficiency. Bacterial, also purulent, meningitis can affect even babies under one year old, and viral (serous) meningitis usually appears in children after mumps or due to Coxsackie and ECHO viruses. The viral form is not as dangerous for children as the purulent form, since it is easier to treat and less likely to cause complications.
Causes of infection
In many clinical cases, meningitis manifests itself as a seasonal disease. But contrary to popular belief, hypothermia cannot be considered its main cause. Statistics indicate that more cases of infection occur in the warm season, as well as in countries with temperate climates. However, experts also record surges in the spread of the disease in the off-season. This is facilitated by several factors: increased humidity and decreased air temperature outside, seasonal hypovitaminosis, as well as longer stays in poorly ventilated areas. Not long ago, scientists noticed another cyclical pattern: every 10-15 years, an epidemic of meningitis occurs in the world. For example, in 2021, an epidemic of serous meningitis was recorded in Russia, caused by the enterovirus ECHO30, which came from China.
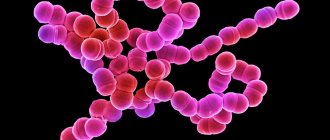
Viral meningitis can be caused by enteroviruses, measles, rubella, chickenpox, herpes or mumps viruses. The bacterial variety of the disease is caused by staphylococci, meningococci, streptococci, salmonella, klebsiella, tuberculosis, pseudomonas or hemophilus influenzae. The causative agents of the disease are fungal etiology, Candida and Cryptococcus. The cause of protozoal meningitis can be protozoan microorganisms (intracellular parasites), and a mixed type of disease occurs due to the complex influence of several factors at once. Carriers of any meningitis are infected people.
People with weakened immune systems and children under 5 years of age are most susceptible to the disease (their immune system is still developing, and the blood-brain barrier is characterized by increased permeability). If we analyze the prevalence of the disease between the sexes, then more cases of inflammation in the brain are diagnosed among men (usually at the age of 20-30 years). Also at risk are pregnant women, people with diabetes, gastrointestinal ulcers, AIDS, those suffering from chronic fatigue or people suffering from malnutrition. In the so-called “Third World” countries, the prevalence of meningitis is almost 40 times higher than the European average. It is also interesting that in Europe and Russia, diseases of bacterial etiology are approximately 3 times less common than viral ones. Doctors say the main reason for this is vaccination, which can help prevent the bacterial form of the disease. After vaccination, the body, when faced with a pathogen, will independently protect itself from it.
To protect yourself, first of all, you need to understand that meningitis is a contagious disease. Depending on the species, it can be transmitted in different ways:
- airborne (through saliva particles during coughing and sneezing);
- fecal-oral (through unwashed hands, fruits and vegetables, contaminated water);
- hemocontact (through blood);
- lymphogenous (through lymphatic fluid);
- placental (from pregnant women to the fetus);
- water (when swimming in open reservoirs or pools);
- contact and household (through household items, dishes, toys);
- through insect bites (mainly in African countries).
In children under 1 year of age, meningitis can be caused by the same reasons as in adults or have other causes. For example, be a consequence of birth trauma, prematurity, damage to the brain or spinal cord, sepsis, disease of the middle ear or nasopharynx. If a woman has meningitis during pregnancy, the risk of transmitting the infection to the fetus is very high, and this can lead to developmental disorders of the child. In most cases, meningitis during pregnancy ends in spontaneous abortion or intrauterine fetal death. But even if the fetus survives, doctors usually advise women to terminate their current pregnancy.
Variants of the course of meningitis
Meningitis is most dangerous for children under 5 years of age. Sadly, every 20 baby diagnosed with inflammation of the meninges dies. The most dangerous form of infant meningitis is considered to be a disease caused by streptococcal infection. Infection usually occurs during the baby's passage through the mother's birth canal. In this case, the disease develops at lightning speed and the child either dies within the first month of life or suffers serious developmental disorders. A complicated form of meningitis is no less dangerous for children. And already at the age of 1 to 5 years, children more often suffer from viral meningitis, which usually goes away more easily than bacterial meningitis.
The course of the disease consists of three periods: incubation, prodromal and the disease itself. The incubation period is the time from the moment the virus enters the body until the first symptoms of the disease appear. At this time, viruses or bacteria are contained in the body in small quantities, and therefore cause almost imperceptible harm. Depending on the type of disease, the incubation period can last from several minutes (rapid development) to several years (chronic inflammation). The duration of the incubation period also depends on the state of the patient’s immune system: the weaker it is, the faster the disease manifests itself. Most often, the incubation period lasts from 1 to 10 days. If the disease was diagnosed in the first two days after infection, then the chances of cure reach 95%.
The fulminant, or fulminant, form of meningitis is the most dangerous. With this form, all stages of the disease pass almost instantly, and death is possible within the first day. Acute meningitis also occurs according to an “accelerated” program: as a rule, 3 days are enough for the infection to reach its peak or even cause the death of the patient.
Purulent meningitis can enter the prodromal stage (the time when classic symptoms of the disease appear) within a few hours after bacteria enter the body. Acute bacterial inflammation progresses very quickly. If the disease was caused by Neisseria meningitidis, the patient may die within a few hours after infection. Against the background of this type of disease, bilateral hemorrhagic adrenal infarction (Waterhouse-Friderichsen syndrome) is possible. And the disease caused by the bacterium Haemophilus influenzae, or hemophilic meningitis, is more common in countries where vaccination against hemophilia is not carried out.
If we are talking about the acute period of the disease, then it usually develops from several days to several weeks, and chronic meningitis manifests itself no earlier than 4 weeks after infection. In addition, while most forms of inflammation in the brain occur rather quickly, chronic meningitis can drag on for even more than 25 years. In this case, the disease develops gradually, and it is almost impossible to determine when the infection entered the body.
Sometimes inflammation of the meninges returns even after successful treatment. Relapse can be caused by viruses, bacteria or non-infectious factors. The most common cause of recurrent disease is herpes simplex virus type 2 (Mollare meningitis). Bacterial meningitis can recur due to congenital or acquired defects of the base of the skull or spine.
Reactive brain inflammation
An acute form of bacterial syndrome that develops at lightning speed. Purulent infections affecting the membranes of the “gray matter” cause a coma and death of the patient. The causes of the disease are meningococci, streptococci, pneumococci. The disease can manifest itself as a consequence of pneumonia or sinusitis.
The primary signs of meningitis are:
- High temperature, which is not knocked down by anything.
- Hardening in the neck and back of the head.
- Migraine attacks, sore throat.
- Constant vomiting.
Reactive meningitis can be fatal within 24 hours. In some cases, even correct diagnosis of the disease will not help to avoid negative consequences - aseptic shock.
Reactive meningitis can be fatal
Symptoms
The insidiousness of meningitis lies in its rapid development. Medicine knows of cases where death occurred just a few hours after the onset of the acute period of the disease. In the classic version, the incubation stage of meningitis in most cases lasts from 4 days to a week. If the disease is recognized in time, the patient has a chance of recovery. And for this you need to know the first symptoms of the disease. However, in most cases, the signs accompanying the onset of meningitis are not perceived by the patient as an alarming signal; the disease is manifested by general infectious symptoms: the patient experiences chills, fever, increased body temperature, and in some cases, skin rashes may appear.
The main symptom of meningitis is headache, which becomes more intense as the disease progresses. The nature of the pain is bursting, the pain can be very intense. In this case, the pain can be localized in the forehead and occipital region, radiating to the neck and spine. Bursting pain is associated with increased intracranial pressure as a result of the action of pathogen toxins. The pain syndrome intensifies when moving the head, as well as due to loud sounds and bright lights. Another sign important for differentiating the nature of a headache is rigidity (strong tension) of the neck muscles. Patients with meningitis (adults and children) do not lie in the usual position on their back. To ease the pain, they turn on their side, tuck their knees to their stomach and instinctively throw their head back.
Inflammation of the membranes of the brain is in many cases accompanied by nausea and severe vomiting. Moreover, the gag reflex does not stop even with a complete refusal of food. In addition, the patient’s body temperature rises (intermittently or remains consistently high at 39-40 degrees) and is not controlled by traditional antipyretics, severe weakness and sweating appear. The patient complains of intolerance to bright light, which worsens the headache. The presence of meningitis can also be suspected in cases where a bursting headache is accompanied by a disturbance of consciousness (a person answers questions slowly and with difficulty or does not respond to requests at all). Mental disorders indicating inflammation of the membranes of the brain can manifest as hallucinations, apathy or aggression. The patient may experience leg and/or arm cramps, muscle pain, and squint (if the inflammation has spread to the optic nerves).
In addition to the classic ones, specific signs will help to recognize meningitis in young children: Kernig's sign and the upper Brudzinski's sign. In the first case, a child lying on his back with his legs raised will not be able to straighten them at the knee joints. The second symptom is also determined in the supine position. If the baby, raising his head, involuntarily bends his knees, this may also indicate inflammation in the meninges. To identify the disease in infants, the fontanel is examined: its swelling and tension are an alarming signal. Another sign of inflammation of the meninges in children is a rash, which is then replaced by specific bright burgundy spots that appear all over the baby’s body.
Conclusion
Meningitis is a dangerous disease that leads to the death of the patient due to lightning-fast development and a sharp increase in temperature to critical levels. To prevent death and other unfortunate complications (loss of vision and coordination in space, neurological and mental problems), you should pay attention to the symptoms in time. Fever is one such sign. If you experience severe headaches, repeated vomiting with a strong jump in temperature, you should urgently consult a doctor. These symptoms often indicate meningitis.
Diagnostics
An experienced doctor can suspect a patient has meningitis based on external clinical signs. But it is too early to make an accurate diagnosis based only on symptoms. Moreover, it is important not only to confirm or deny the presence of the disease, but also to determine its type and stage of development. To do this, the patient will have to undergo a comprehensive examination. In such cases, patients donate blood for a general analysis (CBC), a general urinalysis and a smear from the pharynx mucosa. One of the main confirmatory tests is spinal cord puncture and laboratory diagnosis of cerebrospinal fluid (CSF). Since the brain and spinal cord are in constant contact, clouded cerebrospinal fluid is always considered as the main marker of meningitis.
If during a puncture there are signs of increased cerebrospinal fluid pressure (cerebrospinal fluid flows out in a trickle or in frequent drops), experts regard this as one of the laboratory signs of meningitis. In addition, the color of the cerebrospinal fluid in a sick person changes: it becomes cloudy white or yellowish-green. Not only a cerebrospinal fluid analysis, but also a blood test can also tell about the disease. In the presence of the disease, an increased amount of protein, lymphocytes or neutrophils is observed. The patient's sugar and chloride levels also typically increase.
Differential diagnosis of the disease is based on biochemical analysis of the cellular composition of the cerebrospinal fluid.
To establish the causative agent of the disease, they resort to bacteriological and bacterioscopic examination of the cerebrospinal fluid to determine the causative agent of the disease. Using serodiagnosis, the presence of antigens and antibodies to various pathogens in the patient’s body is determined. Approximate test results for meningitis
| Indicators | Liquor is normal | Viral meningitis | Bacterial | Purulent |
| Color/transparency | No color/transparent | Colorless/transparent or opalescent | Colorless/transparent or opalescent | Whitish or greenish-brown/cloudy |
| Pressure | 130-180 mm water. Art. | 200-300 mm water. Art. | 250-500 mm water. Art. | Increased |
| Rate of cerebrospinal fluid flow during puncture (drops/min.) | 40-60 | 60-90 | Trickle | Rare viscous drops |
| Cytosis (cells/µl) | 2-8 | 20-800 | 200-700 (sometimes 800-1000) | More than 1000 |
| Lymphocytes | 90-95% | 80-100% | 40-60% | 0-60% |
| Neutrophils | 3-5% | 0-20% | 20-40% | 40-100% |
| Sedimentary reactions | – | + (++) | +++ (++++) | +++ (++++) |
| Dissociation | No | Low cell-protein (protein-cell after 8-10 days) | Moderately high cytosis and protein (then protein-cell dissociation) | High cellular protein |
| Glucose | 1,83-3,89 | More than 3.89 | Significantly reduced | Moderately reduced |
| Chlorides (mmol/l) | 120-130 | More than 130 | Significantly reduced | Moderately reduced |
| Fibrin film | Not formed | In 3-5% | In 30-40% | Coarse, often in the form of sediment |
| Reaction to puncture | Causes headache and vomiting | Causes relief, turning point of the disease | Causes significant but short-term relief | Moderate short-term relief |
The results of a blood test will reveal neutrophilia or lymphocytosis, indicating the nature of the disease, as well as the ESR indicator - erythrocyte sedimentation rate, which in high values indicates the presence of an inflammatory process. In addition to laboratory examination of the cerebrospinal fluid and blood, the doctor will definitely need the patient’s medical history, he will conduct a thorough neurological examination, and suggest a computer or magnetic resonance imaging scan. Using an MRI or CT scan, a specialist will be able to examine the condition of the meninges and find the source of inflammation. During a conversation with the patient, the doctor will ask how long ago the headaches began, and whether the patient has been bitten by ticks or mosquitoes (carriers of the pathogen, particularly in Africa and Central Asia).
If suspicions of meningitis were detected in a child, then before sending the baby for a puncture, he should be examined by an ENT specialist, a neurologist, a neurosurgeon and a hematologist in order to exclude other possible causes of the malaise.
Infusion therapy
Infusion therapy is a course of droppers prescribed to patients with purulent meningitis. This method is used when it is necessary to normalize the water-salt balance, to alleviate the patient’s condition with fever and vomiting. In children, infusions are usually given along with diuretics, corticosteroids, and antipyretics. Meanwhile, this method requires special caution, since it increases the risk of hypervolemia (an increase in blood volume in the vessels).
First aid for purulent meningitis is intravenous drip administration of glucose (5-10%) with potassium chloride and saline solution with ascorbic acid. If the patient has high blood pressure and decreased diuresis, 3rd generation HES (hydroethyl starch) is used as a starting solution, and after stabilization of blood pressure and diuresis, glucose-saline solutions are administered intravenously.
The daily volume of intravenous infusions is usually 30-50 ml per kilogram of body weight (provided that this amount does not exceed daily diuresis). If infusion therapy gives a positive result, the solution is administered every 6-8 hours.
For patients with cerebral edema or increased intracranial pressure, a bolus of mannitol is administered as a starting solution (if necessary, 2-4 times a day). After infusion - furosemide, and then dexamethasone.
The standard maintenance infusion regimen for adults consists of glucose solution and saline solution in a 1:1 ratio. Children under one year of age are given the same drugs, but in a 3:1 ratio.
Treatment
Any inflammatory processes in the body are very serious. And if the inflammation occurs in the brain, then there can be no talk of any self-medication at home. Neither traditional methods nor alternative medicine can replace the necessary drug therapy. Meningitis should only be treated by a doctor and only in a hospital. The sooner a patient seeks help from a specialist, the higher his chances of survival.
Medical products (drugs, medicines, vitamins, medicines) are mentioned for informational purposes. We do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
The doctor can draw up a comprehensive treatment program only after receiving the results of the patient’s examinations. Meanwhile, in the case of meningitis, when the clock is ticking, not a minute can be lost. As an emergency treatment, all patients with suspected meningitis are prescribed broad-spectrum antibiotics. At the beginning of treatment, the doctor may prescribe drugs from the group of penicillins, cephalosporins, and macrolides. This will neutralize the bacteria that cause purulent meningitis. For antibiotics to start working immediately, the medicine is usually administered intravenously (drip), and in very severe cases, directly into the cerebrospinal fluid. Treatment of serous meningitis is carried out with the additional use of antiviral drugs. In addition to specific antibacterial or antiviral therapy selected for sensitivity, patients are prescribed nootropic and vascular drugs - Nootropil, Piracetam or their analogues are taken to restore nerve cells and the condition of blood vessels. As anti-inflammatory drugs, doctors provide hormonal therapy to patients with drugs such as Prednisolone, Dexamethasone, Methylprednisolone or Hydrocortisone.
Diuretic therapy is also used in the treatment regimen for meningitis. Diuretic medications are needed to relieve brain swelling.
Regardless of the form and stage of meningitis, children and adults are always prescribed vitamins and minerals. These substances are necessary to maintain immunity, which is always reduced during brain inflammation, as well as to restore the supply of nutrients necessary for the proper functioning of the patient’s systems and organs.
The use of folk remedies
Folk remedies and medicinal herbs can be used in the form of auxiliary therapy aimed at strengthening the body's defenses, relieving anxiety and psychomotor agitation:
- infusions of lavender and peppermint leaves are used as a sedative and analgesic;
- linden leaves, pine needles and rose hips help increase immunity and strengthen blood vessels;
- Decoctions of corn silk and echinacea have a diuretic effect, which prevents the development of cerebral edema.
ATTENTION! Treatment with folk remedies is permissible only in combination with etiotropic and symptomatic therapy.
Prevention
The question of whether it is possible to become infected with meningitis interests many. But other problems are no less pressing: how to protect yourself from the disease and are there any vaccinations against brain inflammation? Meningitis is a contagious disease. But even if a child or adult is surrounded by a patient with inflammation of the meninges, one should not take this fact as a sentence of imminent infection. Meanwhile, protection should be taken care of in advance.
One of the most effective measures to prevent bacterial meningitis is vaccination against pathogens. Nowadays, vaccines against meningitis come in three types: protein, polysaccharide and conjugate. In each group of vaccines, there are drugs that are most suitable for different age categories. Which vaccine to choose for an adult or a child, and how often to vaccinate, should be determined by the attending physician.
Vaccination is, although not 100 percent, still a good guarantee that a healthy person will not become infected.
To protect yourself or your child from infection with viral meningitis, it is also important to follow the rules of hygiene and Sanitary Regulations, eat only clean fruits and vegetables, and wash your hands thoroughly with soap before each meal. The most common source of meningitis infection in the summer is polluted water bodies. To protect yourself from problems, it is important to avoid swimming and especially not to drink water from them.
An excellent way to prevent meningitis is to avoid contact with an infected person. But if this has already happened, you should undergo a course of chemoprophylaxis. It is also mandatory to disinfect the room where the patient was, and monitor contact persons. If contact with a carrier of infection is inevitable (for example, someone in the household is sick), respirators or gauze dressings must be used to prevent infection by airborne droplets. Remember: the infection first enters the upper respiratory tract of a person, settling on the mucous membranes, and then spreads throughout the body. But infection by airborne droplets does not always occur, but only in cases of reduced immunity and impaired functionality of the blood-brain barrier, which protects the brain from harmful substances. To prevent infection, family members are prescribed a course of rifampicin and vaccination using a conjugate vaccine. By the way, many people are interested in whether it is possible to get meningitis again. As a rule, this does not happen, but the possibility cannot be completely ruled out.
Recommendations and contraindications
If meningitis was diagnosed on time and treatment was successful, a person has a chance to live a long, fulfilling life. But for everything to be exactly like this, after completing treatment in a hospital, you will have to follow the doctor’s recommendations.
After suffering from meningitis, it is important to continue monitoring with a doctor: it is important to be examined by a neurologist every three months. And so on for at least 2 years. In addition, some restrictions are temporarily imposed on the regime and way of life. It is forbidden to fly on airplanes for at least 6 months after illness. Flight during this period is dangerous because intracranial pressure changes sharply during the flight, which can negatively affect the restoration of liquor dynamics after inflammation of the meninges. Also, doctors do not advise going to the seaside immediately after an illness, especially for children. The temporary ban also applies to sports: after illness, heavy physical activity should be avoided for about 2 years.
You will also have to reconsider your usual diet: give up fatty and fried foods in favor of boiled, stewed, baked or steamed. For meat, give preference to dietary varieties: rabbit, veal, poultry, and fish. It is useful to eat boiled porridge as a side dish, and heat-treat fruits and vegetables before eating. It is useful to eat low-fat dairy foods; the best drinks are jelly and compotes, if tea is not strong. The diet after meningitis completely excludes alcohol.
Physical exercises and massages are presented for informational purposes. We do not recommend using them without a doctor's advice. We recommend reading: “When can physical exercise and massage pose a threat to health?”
Physiotherapy during the rehabilitation period should consist of a course of massage, electrophoresis with the use of medications. To restore cognitive functions and coordination, they resort to magnetic and magnetic laser therapy, and use electrosleep. A course of physical therapy will help restore motor function. But for this you need to exercise under the supervision of a physical therapy specialist. To restore range of motion, strength and coordination, occupational therapy is used, and a cognitive program is necessary to restore memory, attention and logical thinking.
Possible complications
Inflammation of the meninges itself is a serious problem. But against the background of this disease, other, no less complex complications are possible.
One of the most common is cerebral edema. As a rule, a critical excess of cerebrospinal fluid accumulates already on the second day of the disease. A complication can be suspected based on several external signs. The patient suddenly loses consciousness, develops shortness of breath, and blood pressure readings either sharply decrease or increase. There are also jumps in heart rate: from severe bradycardia (slow) to tachycardia (rapid). If cerebral edema is not removed in time, death is possible, which usually occurs due to paralysis of the respiratory center.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
The second common danger is infectious-toxic shock. It occurs as a result of poisoning of the body by decay products of pathogenic microorganisms. Against the background of this process, the patient’s body temperature usually drops, but intolerance to light and loud sounds increases, and shortness of breath appears. In many cases, infectious-toxic shock occurs along with cerebral edema. The result is coma and death within a few hours.
After suffering from meningitis, the body will need time to recover. Sometimes quite long. If the inflammatory process was caused by meningococcal infection, then there remains a high risk of damage to other organs or entire body systems. Only timely seeking medical help can prevent serious consequences.
Meningitis can cause deafness, paralysis, epilepsy, and hormonal disorders. In children, hydrocephalus, complete deafness or blindness, acute renal failure, developmental delays, and cerebroasthenia are possible. Often, inflammation of the membranes of the brain in children ends in death.
Risk group
Children and the elderly are at risk for meningitis. In addition, this disease is often diagnosed in people with an absent spleen and immunodeficiency.
The spread of meningitis, like all other infectious diseases, is more active in crowded places, closed groups, for example, in kindergartens, schools, student dormitories, barracks, since it is easier to get meningitis if you are in the company of asymptomatic carriers.
Most often, meningitis is transmitted by airborne droplets. This mechanism of infection transmission is considered the most common and characteristic of meningitis of viral origin. The infectious agent is transmitted through coughing, sneezing, kissing and sexual contact.
Newborn babies can become infected from an infected mother through the birth canal. The likelihood of infection is especially high in children born by caesarean section. Bacterial and viral meningitis can be transmitted this way.
Infection with meningitis can occur through the oral-fecal route: through dirty food or untreated water.
In addition, meningitis can develop as a result of the bite of an insect or animal that carries an infectious agent.
Expert opinion
Andrey Igorevich Volkov
Neurologist, Candidate of Medical Sciences
Meningitis of any origin is a dangerous infectious disease that affects adults and children. Without timely treatment, death occurs in 80% of cases. It has been proven that, despite the initiation of therapy, 10% of patients die within the first day from the onset of pathological symptoms. Meningitis most often affects children. Viral etiology accounts for 60–70% of cases. Fungal meningitis accounts for 1–3%. It is not possible to diagnose and treat an infectious disease at home. Therefore, it is necessary to seek medical help soon after the first signs of the disease appear.
The most informative method for diagnosing meningitis is lumbar puncture. The causative agent of the disease is sown in the cerebrospinal fluid. To identify the localization of the pathological focus in the brain area, neurologists at the Yusupov Hospital prescribe MRI and CT. Etiotropic therapy is selected depending on the results obtained. Symptomatic treatment is aimed at alleviating the general condition. Vaccination is considered the only reliable means of preventing meningitis.
We answer your questions
Do they take you into the army after meningitis?
The question of whether people with meningitis are accepted into the army is of interest to many. Let us say right away that no one with an illness will be taken to the barracks directly, since any inflammation (especially the meninges) should be hospitalized. Workers diagnosed with meningitis are unconditionally given sick leave. If cases of the disease are recorded in a school or kindergarten, the educational institution is closed for quarantine. But what awaits the young man who suffered from meningitis several years ago? If there is documentary evidence of illness, the conscript automatically enters the reserve.
Meanwhile, the issue of compatibility between the army and meningitis is of interest not only to those who have had the disease, but also to healthy conscripts. Can you get meningitis in the army? Theoretically, such a risk exists, as, indeed, in boarding schools, schools, kindergartens, sanatoriums or children's camps. Therefore, to avoid an epidemic, vaccination is carried out. Conscripts should be vaccinated against meningitis approximately 75-80 days before conscription.