Osteochondropathy is provoked by excessive loads and frequent injuries (playing professional sports, etc.). Modern research also confirms a genetic factor in the inheritance of the disease. Osteochondropathy itself does not have specific symptoms, and its manifestations can only be detected in advanced stages of the necrotic process. At the same time, the disease responds well to conservative treatment, during which the patient is prescribed rest, physiotherapeutic procedures and therapeutic exercises.
What is osteochondropathy?
Osteochondropathy is a complex term that includes a whole group of diseases that lead to malnutrition of bones and their subsequent necrosis (death).
There is little statistical data on the incidence of osteochondropathy. However, many researchers note that children (especially boys) from 10 to 18 years old are susceptible to the disease, which is associated with congenital circulatory disorders in bone tissue.
Today, osteochondropathy has a favorable prognosis. However, it is almost impossible to diagnose necrotic disorders in the early stages. Therefore, treatment of the disease begins in the later stages, when there is a significant weakening of the bone skeleton. The latter is fraught with frequent fractures, which can be caused by muscle strain, body weight, cramps, vomiting and even coughing.
Similar drugs
In addition to Osteovit, there are other drugs on the market whose effects are similar to those of this dietary supplement:
- Chondromax Herbal. This homeopathic remedy is recommended to be used to relieve inflammation in the joints, as well as to treat diseases of the spine. The drug is also used for preventive purposes. Chondromax Herbal has a positive effect on the functioning of the cardiovascular, nervous and digestive systems. The price of the drug is slightly higher compared to the cost of Osteovit.
- Artikon. A drug prescribed for people doing heavy physical work. The calcium contained in this medicine strengthens the skeletal system.
- Sabelnik capsules. This is a cheaper analogue of a dietary supplement, widely used to treat diseases of the skeletal system associated with age-related changes. This remedy has a good effect on the well-being of people suffering from changes in weather conditions. In addition, cinquefoil is used during rehabilitation (after fractures, muscle sprains, ligament ruptures, etc.).
- Karipain plus. A medication that has shown its effectiveness in the treatment of osteochondrosis, radiculitis, intervertebral hernia, arthritis and arthrosis.
- Diclovit. The remedy is prescribed for joint diseases, neuralgia, sciatica, gout, and spinal diseases. Diclovit is widely used to reduce pain in the postoperative period.
- Revmalgon. A drug used to prevent age-related changes in the musculoskeletal system. Revmalgon prevents the development of osteochondrosis and osteoporosis.
- Arnisin. A medicine that is used to treat the musculoskeletal system.
- Artiflex Plus. Indications for the use of this drug are diseases of the joints and spine. Artiflex also helps patients undergoing a recovery course after undergoing operations.
- Chondromazine. The product is used to treat ailments of the hip joint and knees. In addition, this drug is effective in the fight against osteochondrosis.
- Structuvite. The medicine is recommended for athletes who have received injuries of varying severity during training or competition.
The modern pharmaceutical market is overflowing with drugs that have a positive effect on the functioning of the skeletal system. But there are no worthy analogues of Osteovit yet.
This opinion is shared by leading experts involved in the development of therapeutic drugs.
Causes of the disease
The etiology of osteochondropathy remains a “blank spot” in medical science. It is believed that the development of the disease is facilitated by frequent trauma to the skeletal system and excessive physical activity.
Risk factors for osteochondropathy include:
- genetic predisposition (for example, the incidence of osteochondropathy in children of sick parents is several times higher than in healthy families);
- congenital disorders of blood supply to bone tissue;
- metabolic disorders (metabolic syndrome X with disorders of carbohydrate, fat and purine metabolism);
- poor nutrition with a deficiency of vitamins and microelements (calcium, phosphorus, magnesium, etc.);
- long-term eating disorders (anorexia, bulimia);
- nutritional (nutritional) or hormonal obesity;
- bacterial and viral infections;
- professional sports activities associated with constant trauma and being in non-anatomical positions (gymnastics, figure skating, circus acrobatics, fencing, etc.).
Composition of the drug
The therapeutic and preventive effect of Osteovit is due to the microelements that make up this medicine:
- Vitamin D3. This element is necessary to maintain the integrity of bones, because it restores the balance of calcium in the body. Calcium is better absorbed, preventing the rapid destruction of the skeletal system. In addition, vitamin D3 is involved in metabolic processes and stimulates the growth of cells necessary for the health of the central nervous system.
- Vitamin B6. A trace element that helps the absorption of magnesium by bone tissue. In addition, B6 improves digestion and has a beneficial effect on the liver. Thanks to the presence of this vitamin, Osteovit is considered a beneficial remedy for joints.
- Drone homogenate. This is a unique component that is the larvae of male bees. They are preserved in a special way, thanks to which all useful microelements are preserved in them: phosphorus, calcium, magnesium, iron and potassium. And the combination of drone brood and vitamin D3 helps to successfully fight viral and respiratory diseases. The body produces its own antibiotics that fight infections.
How does the disease develop?
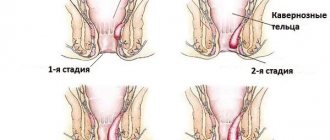
The course of osteochondropathy is chronic and staged. The first stage is the initial non-purulent necrosis of the bone (lasts up to six months), caused by the above etiological factors. Patients complain of constant pain in the area of necrosis, aggravated by palpation; impaired mobility of the limbs appears. However, no abnormalities in the bone tissue are observed on the x-ray.
The second stage manifests itself as an impression fracture due to “indentation” under the weight of one’s own body or during muscle tension. The stage lasts from several weeks to a year. There is a “subsidence” of the bones and their wedging into each other. Changes appear on the x-ray: the bone structure is blurred, the affected areas are darkened, and the joint spaces are widened.
The beginning of the third stage of pathology development (lasts about three years) is indicated by a decrease in bone density: fragmentation of bone tissue, resorption of necrotic zones and their replacement with new (granulation) tissue are noted. When X-rayed, the bone resembles a chessboard with a random alternation of darkening and clearing.
The fourth stage is recovery and lasts up to one and a half years. Usually there is a restoration of the usual shape of the bone with the development of residual deformations (curvatures). The structure of the bone tissue also returns to normal, which can be observed on the next x-ray.
As a rule, the total duration of the stages does not exceed 4 years. In this case, the course of the disease is benign, but in the absence of treatment, not only residual curvature of the bones may appear, but also complications of the process in the form of fractures and deforming arthrosis.
Types of pathology
The modern classification identifies four categories of osteochondropathy of childhood and puberty (adolescence):
- Necrotic processes in the epiphyseal parts - the expanded end sections of tubular bones. This group includes pathologies of the femoral heads and metatarsal bones, the thoracic part of the clavicle, and the phalanges of the fingers.
- Dystrophic disorders of tubular bones: scaphoid feet, lunate and scaphoid carpals, vertebral bodies.
- Degenerative processes in bone outgrowths - apophyses: tubercles of the tibia and calcaneus, as well as in the apophyseal rings of the vertebrae.
- Incomplete osteochondropathy with damage to the articular structures of the elbow, knee and ankle joints.
Symptoms
Each of the noted osteochondropathy has its own characteristic features of localization, manifestation and course.
Perthes disease
Dystrophic disorders occur in the femoral head with partial involvement of the hip joint in the pathological process. The disease usually manifests itself at 5-7 years of age, usually in boys. Among the provoking factors are injuries and dysplasia (developmental disorders) of the hip joints.
As a rule, patients complain of the appearance of lameness and subsequent pain in the area of the hip joint and knee. Over time, the mobility of the joints decreases: hip abduction and rotation are limited. Atrophy (wasting) of the muscles of the buttocks, thighs and lower legs often appears.
In some cases, the disease may be complicated by subluxation of the hip, which is accompanied by shortening of the limb and difficulty in supporting it.
Schlatter's disease
The pathology occurs at the age of 11-17 years (more often in boys) and affects the tuberosity of the tibia. Athletes, especially fencers, are susceptible to the disease, which is associated with extreme load on the knee joints.
Osteochondropathy manifests itself as pain in the upper third of the lower leg when kneeling, squatting, and climbing stairs. Swelling in the affected area is often observed. At the same time, the range of motion in the knee does not suffer.
Keller's disease
This pathology has two types:
- Damage to the navicular bone of the foot. A relatively rare disease that occurs mainly in boys 5-8 years old. Pain appears on the anterior inner surface of the foot, which intensifies when palpated and walks. The affected area often swells, which changes the gait of the child, who tries to step not on the entire foot, but on its outer edge.
- Necrosis of the 2nd and 3rd metatarsal bones. The problem most often occurs in girls of puberty. Pain appears at the base of the second and third toes. Pain increases with palpation, raising on toes, running and walking. The affected area is often swollen, and shortening of the second and third fingers of the lower limb is sometimes observed.
Schinz's disease
Necrosis is observed at the level of the apophysis (tubercle) of the calcaneus. The development of the disease is observed mainly in adolescents, but there are frequent cases of heel osteochondropathy in children of early school age. Typically, patients complain of pain in the heel bone after running or jumping. Swelling often occurs without inflammatory signs (redness and warming of the skin).
A characteristic manifestation is a change in gait that relies on the toes to reduce pressure on the heels. A distinctive feature of the disease is the disappearance of any discomfort and pain at night.
Calvet disease
The pathology is characterized by necrotic lesions of the vertebral bodies - platyspondyly. The disease manifests itself with a rise in temperature to subfebrile levels; Pain sensations appear in the spine, which are paroxysmal in nature. In this case, the pain tends to spread to the lower extremities in a standing position and disappear during night sleep.
When examining the spine, some “retraction” of the spinous processes of necrotic vertebrae is noted. Feeling this area leads to increased pain, as well as detection of protective muscle tension. The mobility of the spine in the affected area is often limited.
Scheuermann-Mau disease
The disease appears during puberty in young men. Usually the course of osteochondropathy of the vertebral apophyses is asymptomatic. Whereas the reason for visiting a doctor is a curvature of posture - kyphosis (stooping). During the period of deformation of the spinal column, discomfort appears in the thoracic region, which intensifies when sitting for a long time.
Along with the progression of the disease, shooting pains appear between the shoulder blades, a visible hump, as well as sensory disturbances (feelings of “goosebumps” on the skin or anesthesia) and motor disorders (muscle weakness or paresis).
Koenig's disease
The disease refers to partial osteochondropathy with damage to the bone structures of the joints. During the necrotic process, a wedge-shaped portion of the articular surface of the bone is separated, turning into a so-called “intra-articular mouse” that moves freely throughout the articulation cavity. The disease is observed with equal frequency in children and adults. Usually the lesion covers the knee, less often the shoulder and ankle.
When a fragment is pinched in a joint, a sharp pain syndrome occurs, which can be relieved by careful flexion and extension of the limb. The presence of an “intra-articular mouse” leads to constant trauma to the bone structures of the joints with the subsequent development of inflammation and deformation of the joints.
Diagnostics
Only an orthopedic doctor can make a correct diagnosis based on the information obtained after the patient undergoes instrumental examinations. However, not the least place in the diagnostic process is occupied by the following manipulations performed directly by the clinician:
- studying the medical history - to establish the presence of endocrinological pathologies or infectious diseases;
- analysis of life history - will allow you to find out the most characteristic physiological predisposing factor for a particular person;
- detailed examination and palpation of the affected area - this should also include assessment of gait and motor functions;
- a thorough interview of the patient or his parents to determine the first time of appearance of clinical signs and the degree of their severity. The combination of such factors will indicate the stage of progression of osteochondropathy of the scaphoid bone or any other localization.
Instrumental diagnostic procedures are based on the following:
- radiography of the affected segment;
- Ultrasound of bones;
- magnetic resonance imaging and CT scan of bones.
Osteochondropathy of the knee joint on x-ray
Laboratory studies are of an auxiliary nature and involve the following:
- blood biochemistry;
- hormonal tests;
- general clinical blood test.
How is osteochondropathy treated?
Treatment of osteochondropathy consists of a conservative approach: a protective regimen, ensuring rest of the affected part of the body and treatment of the underlying disease (metabolic or hormonal disorder, infection or micronutrient deficiency). Only the attending physician can prescribe medications.
- Perthes disease . Treatment of femoral head necrosis is carried out in a hospital setting with long-term immobilization. In some clinical cases, specialists resort to skeletal traction. The patient is prescribed physiotherapeutic procedures, gymnastics and spa treatment. If there is significant destruction of the femoral head, reconstructive surgery is performed.
- Schlatter's disease . In case of dystrophic lesion of the tibia tuberosity, the patient is given a plaster splint for 1.5-2 months in order to immobilize the knee. Physiotherapeutic courses (paraffin, electrophoresis, etc.) are also prescribed.
- Keller's disease . Patients are advised to limit the load on the foot (exclude running, jumping, long walking). If there is significant pain, a plaster boot is applied. During the recovery period, physiotherapy and selection of orthopedic shoes are indicated.
- Schinz's disease . At the time of exacerbation, the patient must exclude axial load on the heel (use a cane or crutch). Calcium electrophoresis and thermal effects are used as physiotherapy procedures.
- Calvet disease . Therapy for necrosis of the vertebral bodies is carried out in a hospital. Patients should follow bed rest, perform physical procedures and health-improving exercises. Complete restoration of the vertebrae usually takes about 3 years.
- Scheuermann-Mau disease . Damage to the apophyses of the vertebrae leads to persistent curvature of the spinal column (the appearance of a hump). To restore posture, strict bed rest is necessary. If pain persists, a posterior plaster cast may be applied. Patients are also advised to massage the back and abdominal muscles. The recovery period is based on physical therapy.
- Koenig's disease . If articular structures are damaged (before the formation of a bone fragment), resting the affected joint and performing physical therapy is sufficient. In case of persistent pain syndrome, it is possible to use blockades with anesthetics (Lidocaine, Novocaine). If an “intra-articular mouse” has formed, arthroscopy is required to remove the bone fragment from the joint cavity.
Treatment
Most often, it is possible to get rid of damage to the ankle, knee, hip or any other joint using conservative therapeutic techniques. It follows that the basis of treatment is:
- application of skeletal traction - often indicated for osteochondropathy of the femoral head;
- physiotherapeutic procedures, namely calcium and phosphorus electrophoresis, as well as paraffin applications and heating;
- vitamin therapy;
- performing a complex of physical therapy, which is selected individually for each patient with a similar diagnosis;
- wearing a special plaster boot - applicable for damage to the metatarsal bone and navicular bone of the foot. After this, it is necessary to wear shoes with arch support;
- massotherapy.
As for surgical intervention, it is indicated only in cases of the formation of an “articular mouse” - this occurs in situations where the damaged area is separated from the articular surface. Frequent joint blockades for osteochondropathy of the patella or other area are also recommended for surgery.
Prevention
To prevent the development of osteochondropathy it is necessary:
- carefully monitor children with a genetic predisposition to the onset of the disease (born in families with osteochondropathy);
- diagnose hereditary disorders of the blood supply to bone tissue and metabolic disorders (metabolic syndrome X with inadequate carbohydrate, fat and purine metabolism);
- correct poor nutrition with a deficiency of vitamins and microelements (calcium, phosphorus, magnesium, etc.);
- treat long-term eating disorders (anorexia, bulimia) in a hospital setting;
- control and eliminate nutritional (dietary) or hormonal obesity;
- carry out specific diagnosis and treatment of bacterial and viral infections;
- if possible, exclude professional sports activities associated with permanent injuries and being in non-anatomical positions (gymnastics, figure skating, circus acrobatics, etc.).
Remember! Considering the predominantly early development of osteochondropathy (at school and adolescence), responsibility for preventing the disease falls on the child’s parents.
It is worth noting that the disease has a favorable prognosis. However, advanced aseptic necrosis can lead to deforming arthrosis and fractures. The latter, with massive bone dystrophy, are caused by vomiting, muscle spasms and even coughing. But such complications are rare, while no fatal cases of osteochondropathy have been recorded to date.