Cystitis is an inflammatory disease consisting of irritation and damage to the walls of the bladder.
Cystitis actually affects women much more often. Approximately 2-3 out of 10 representatives of the fair sex suffer from this disease at least once in their lives. In males, only 1% have some form of cystitis. In most cases these are men over 45 years of age.
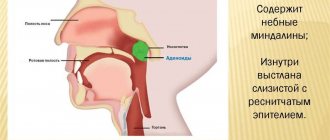
The difference in the incidence of diseases between the sexes is explained by physiological differences in the structure of their genitourinary organs. First of all, men have a very long and tortuous urethra. But the walls of the urethra are an extremely difficult obstacle for pathogenic microorganisms, since immune cells are active in them.
In addition, in the male body, the opening of the urethra is located very far from the anus, so it is practically impossible for pathogenic microflora to enter the canal from the anus.
What is cystitis in men
Cystitis is constant aching pain in the lower abdomen, urination in small portions with stinging and burning, frequent urges and even blood in the urine. There is no talk about sex during the period of exacerbation, since even an erection causes discomfort, not to mention ejaculation.
Inflamed bladder walls are unable to contract normally and store urine. They swell, ulcerate, and in some cases become covered with ulcers or granulomas. With severe inflammation, the temperature rises and general weakness occurs.
As for infecting partners, it all depends on the type of cystitis. If the inflammation is caused by an infection, then there is a risk of its transmission during unprotected sex. Pathogens can migrate both up and down the urethra. Together with sperm, they enter the woman’s genital tract. As a result, either inflammation will develop or the immune system will suppress pathogens.
The smell of discharge from cystitis
Usually, any woman's discharge has a characteristic delicate odor. With cystitis, it changes to unpleasant. In the case of a slightly sour aroma, this is most likely an associated fungal infection. If you smell a very nasty odor, then there may be a purulent disease. A fishy aroma indicates that you have vaginal dysbiosis.
Regardless of the color or smell of discharge from the vagina or urethra that bothers you, be sure to tell your doctor. This will greatly facilitate your therapy and even speed up your recovery.
Classification
The nature of bladder inflammation depends on many factors. Depending on the time of occurrence, cystitis can be primary or secondary. Secondary develops against the background of already existing inflammation: prostatitis, urethritis, pyelonephritis. Primary occurs as an independent disease.
According to the form of its occurrence, acute and chronic cystitis are distinguished. Acute develops quickly and manifests itself clearly. The disease usually develops into a chronic form as a result of an untreated acute form. The frequency of relapses depends on immunity and lifestyle.
Acute cystitis can be complicated or uncomplicated. In the first case, in addition to inflammation of the bladder, the man is faced with pathological changes in the kidneys, urethra, and testicles due to the migration of infection. Chronic cystitis is almost always complicated, since inflammation is supported by systemic diseases (diabetes mellitus) and changes in the normal structure of the bladder walls. This form most often occurs in the elderly.
According to the degree of distribution, there are 3 forms of cystitis:
- Cervical – inflammation of the bladder neck.
- Diffuse - damage to the entire cavity.
- Focal - inflammation is localized in several limited areas.
Based on the nature of pathological changes in the walls of the bladder, the following types of cystitis are distinguished:
- Hemorrhagic. Characterized by ulceration and bleeding from the urethral canal (hemorrhage). In acute inflammation, this form occurs in 80% of cases.
- Catarrhal. Inflammation affects the first two layers of the mucous membrane of the walls. Swelling, increased blood flow, and mucopurulent plaque are observed.
- Ulcerative. Often develops after radiation therapy. Characteristically, all layers of the wall are affected.
- Phlegmonous. Severe purulent inflammation, which affects not only the membrane of the bladder, but also the tissue around it.
- Gangrenous. The wall structure is completely destroyed, necrosis often develops. Dead tissue comes out during urination.
- Endoscopic. The mucous membrane swells greatly, thickens, ulcerations and microulcers appear on it. The elasticity and contractility of the walls decreases.
- Encrusting. On the surface of the mucous membrane, layers of salts form, against which chronic ulcers and polyps appear.
- Cystic. In the submucosal layer of the walls, small tubercles of lymphoid tissue form.
Combined forms of cystitis are often diagnosed.
Signs of acute and chronic form
If cystitis is present in men, the symptoms depend on its form:
| Acute | Chronic |
| • Low urine output (only 10-20 ml). • Sharp pain syndrome. • Decreased performance. • General weakness. • Increase in temperature to a febrile state. • Urinary incontinence (the condition worsens at night). • Increased irritability, nervous instability. • Presence of mucus, blood or other impurities in the urine. • Pain and aches in muscles. | • Chills. • Mild pain. • Stable temperature change up to 37 degrees. • Decreased sexual activity in men. • Burning sensation during urination. |
The transition of cystitis from acute to chronic form is usually rapid.
This happens after 10-14 days. The disease must be treated as soon as the first sign appears. Acute cystitis can be completely cured, but chronic cystitis cannot.
Causes of cystitis
Depending on the causes, there are two main forms of cystitis: infectious and non-infectious. Each of them has its own provoking factors.
Infectious cystitis
Types of cystitis depending on the causative agents:
- Fungal (candida);
- Chlamydial;
- Trichomonas;
- Tuberculous;
- Viral, occurring against the background of influenza or due to the penetration of adenoviral, parainfluenza, herpetic infections;
- Mycoplasmosis;
- Ureaplasmosis;
- Nonspecific, caused by Escherichia coli, staphylococcus, streptococcus, enterococcus.
To enter the bladder through the urethra, the pathogen must first attach to the epithelium of its wall. This is not so simple because the lining of the urethral canal is constantly renewed, the cells are carried out in the urine. Once the infection has taken hold, it means that it has a very good ability to adhere, or the man has impaired immunity and hormonal levels.
Once in the bladder, the pathogen must also attach to its wall, more precisely, to the lining - the urothelium. In a healthy man, the bladder wall is protected by a special glycosaminoglycan layer that prevents this process. When it is damaged due to disruption of the synthesis of protective cells, inflammation develops.
Attachment of E. coli to damaged bladder walls
Chlamydial, mycoplasma and ureaplasma cystitis are dangerous due to their gradual asymptomatic development. Acute symptoms occur against the background of significant damage to the structure of the bladder walls and a decrease in cellular immunity.
Viral cystitis occurs in an acute form and goes away along with the underlying disease in 2-3 weeks. The virus usually causes disruption of the vasculature and nerve endings of the bladder walls.
Non-infectious cystitis
Types of non-infectious cystitis:
- Chemical.
- Kholodova.
- Exchange.
- Parasitic.
- Neuropsychic (stressful).
- Ray.
- Allergic.
The above types of cystitis ultimately become infectious, but the prerequisite for their development are external factors that provoke damage to the walls of the bladder.
Hypothermia is a common cause of non-infectious cystitis. Under the influence of cold, the vessels of the bladder walls spasm, blood circulation slows down and defense mechanisms are suppressed, which creates favorable conditions for the development of infection.
Urologist and dermatovenerologist Lenkin Sergey Gennadievich will tell you about the causes of cystitis in men
Chemical cystitis is caused by toxic substances. They enter the bladder through the blood or when drugs are infused for therapeutic purposes in too high a concentration. Substances that cause chemical cystitis:
- Phenacetin;
- Urotropin;
- Cantharidin;
- Ethanol;
- Erroneous infusion of iodine and boric acid into the bladder instead of collargol;
- Cytostatics used to treat cancer patients: thiotef, endoxan, cyclophosphamide.
A burn with iodine is one of the most severe, since this substance causes deep tissue damage. Urgent rinsing with a solution of lapis (silver nitrate) is required.
Causes of allergic cystitis:
- Food products.
- Medicines.
- Waste products of parasites.
- Condoms.
- Cosmetical tools.
Allergic inflammation is quickly and effectively relieved with antihistamines.
An example of cystitis caused by a metabolic disorder is hypercalciuric. Occurs against the background of calculous pyelonephritis. The kidneys secrete excess amounts of calcium salts, which damage the walls of the bladder. Inflammation is complicated by the presence of Bacillus, Proteus, and Staphylococcus. The main symptom is cloudy, foul-smelling urine. Treatment is aimed at eliminating pathogenic microflora and taking medications to acidify urine.
Functional bladder disorders occur against the background of severe stress. No bacteria are sown; there is no connection with hypothermia or hypovitaminosis. A distinctive feature is a persistent course, a tendency to frequent relapses.
The cause of parasitic cystitis is schistosomiasis (bilharzia). Infection can occur in a pond or during agricultural work. The spread of parasites occurs against the background of general malaise, headache, sweating, and fever. The larvae develop, among other things, in the veins of the walls of the bladder, resulting in granulomatous or ulcerative inflammation of its walls. Parasite eggs are released in the urine, and blood is periodically observed in it. The first signs appear 4-6 months after infection. The prognosis without proper treatment is unfavorable: shrinkage of the bladder, narrowing of the ureters, pyelonephritis. If eggs are detected, Praziquantel and Metrifonate are prescribed. This type of cystitis can be complicated by cancer, in which case it is removed (cystectomy).
Schistosomiasis (schistosomiasis, bilharzia) is a tropical parasitic disease caused by blood flukes (trematodes) of the genus Schistosoma
Radiation cystitis develops some time after irradiation during the treatment of oncological lesions of the pelvic organs. The reason is the increased sensitivity of tissues to ionizing effects, excessive dosage, and too short intervals between sessions. As a result, sclerosis of the nerves and vessels of the bladder wall occurs, and metabolic processes are disrupted. Against this background, ulcers, fistulas, and fibrous areas develop.
A type of cystitis that doctors do not understand is postcoital cystitis, which occurs every time after sex. Characterized by an acute onset and course, like a normal bacterial inflammation, but there are no bacteria. For prevention, men are advised to urinate immediately after sex.
Cystitis can occur against the background of stagnant processes in the pelvic area. The mechanism of inflammation development is triggered due to disruption of microcirculation and intercapillary exchange. As a result, the walls of the bladder experience oxygen starvation, their structure is disrupted, and functionality decreases.
Another difficult to diagnose form of cystitis is interstitial. Signs:
- Chronic pain in the pelvic area;
- Urgent and frequent urge to urinate;
- Burning when urinating;
- Absence of pathogens and signs of inflammation in the urine.
During cystoscopy (examination of the bladder from the inside), pathological changes from slight redness to deep ulcers are detected on the walls. The problem is that they are located under the mucous layer and provoke permanent inflammation. In the chronic form of cystitis, the process of scarring begins, which leads to wrinkling of the walls and a narrowing of the volume of the organ. In 90% of cases, interstitial cystitis has an atypical form: neither laboratory nor instrumental studies show anything. Possible causes: autoimmune disorders, intoxication, endocrine disorders.
Discharge color
Fluid can be released from two sources - the vagina and urethra. Let's consider the first case. Vaginal secretion is normally transparent or slightly white, its amount is determined by the individual characteristics of the woman. If you do not have any unpleasant sensations regarding the volume or influence of these secretions, then there is no point in mentioning this at the appointment.
It's another matter if you find brown marks on your underwear and labia. In parallel with cystitis, this may indicate inflammation of the uterus, appendages or cervical erosion. You need to visit a gynecologist for proper specific therapy.
With sexually transmitted diseases, purulent discharge appears, yellow or green. Proper and timely treatment of these infections will lead to relief from cystitis.
Mostly, diseases of the female reproductive system provoke cystitis; in this case, it is more likely to be concomitant. Its treatment comes as an addition to the main source of health problems.
Urethral discharge is closer to bladder infections:
- a whitish coating is a fungal infection;
- bloody or brown discharge indicates acute or chronic inflammation in the bladder and urinary canal;
- When pus appears, you can talk about a severe bladder infection.
The most dangerous ones are pink or bloody discharge. They indicate the severity of the disease and its ascent into the renal tissue.
Diagnostics
A urologist diagnoses cystitis. Basic methods:
- Laboratory tests of urine and blood.
- External examination by a urologist, smear from the urethral canal.
- Cystoscopy and cystography (X-rays after administration of a contrast agent).
- Ultrasound of the genitourinary system.
- Palpation of the lower abdomen.
- Uroflowmetry.
- Multispiral computer cystourethrography.
If necessary, the patient is referred to a neurologist or endocrinologist.
Disease prevention
Preventive prevention of the development of cystitis is one of the most correct decisions. Because if a man maintains hygiene and leads a healthy lifestyle, then the risk of cystitis is minimal.
But if there are still pathologies listed below, then it is necessary to take them under control so that they cannot provoke the onset of the disease:
- pyelonephritis;
- stress factors and constant hypothermia;
- diseases of the male genitourinary system;
- the appearance of purulent foci.
For such diseases, it is necessary to constantly check the genitals and undergo a course of antimicrobial preventive therapy.
How to treat cystitis in men
Uncomplicated primary cystitis with properly prescribed therapy can be cured in 7-8 days. Chronic cannot be treated. It can be put into stable remission and maintained with all efforts.
Bacterial cystitis is treated with antibiotics, which are prescribed based on the results of urine culture. Usually these are cephalosporins, fosfomycin, fluoroquinolones: Nolitsin, Azithromycin, Levofloxacin. To relieve pain, non-steroidal anti-inflammatory drugs and antispasmodics are prescribed.
Medicines for the treatment of male cystitis
Drug therapy can be etiotropic or symptomatic. Etiotropic therapy is aimed at counteracting pathogenic organisms - the causative agents of the disease. The goal of symptomatic treatment is to relieve unpleasant symptoms - pain and spasm.
If the cause of the disease is a bacterial infection, then a course of antibiotics is necessary. The most commonly used drugs are fluoroquinolones (such as lomefloxacin, ofloxacin, gatifloxacin, ciprofloxacin), nitrofurans, cephalosporins, and less commonly penicillins. The duration of treatment is usually a week.
Before choosing an antibiotic treatment regimen, it is necessary to conduct research on the type of pathogen and its resistance to antibiotics.
Preparations with herbal anti-inflammatory and antibacterial components are also often used, such as Canephron, Phytolysin, Monurel, Urocam, Uroflux, Urolesan, Cyston, bearberry herb, horsetail and St. John's wort decoction.
Another class of drugs used for the disease are antispasmodics (papaverine, drotaverine), which help relieve spasms and the pain syndrome caused by them. NSAIDs are also used to reduce symptoms of pain and inflammation. For severe pain, novocaine blockades are used. It is also recommended to take vitamins to increase the body's resistance to infection.
Prevention of cystitis in men
Prevention measures:
- Avoid stress, hypothermia, unprotected sex.
- Rationalize nutrition.
- Do not abuse alcohol, stop smoking.
- Perform exercises regularly to accelerate blood flow in the pelvic area and strengthen muscles.
- Do not abuse spicy, salty foods, or caffeinated drinks.
- For men with diabetes, it is important to monitor their blood sugar levels.
Urinalysis according to Nechiporenko
After detecting a pathology in a urine test, the doctor prescribes a test to determine the condition of the organs of the urinary system. The content of elements in 1 ml of urine is determined.
The accepted norm is: the number of red blood cells in 1 ml of urine is no more than 1000, leukocytes – 2000, cylinders – 20. In the case of acute inflammation, these figures can increase several times.
It should be remembered that if the material is collected incorrectly or hygienic requirements are not met insufficiently, the result may be unreliable. In order for tests to confirm the presence of a disease or exclude it, you must follow the rules for collecting urine:
- wash your hands thoroughly with soap;
- retract the foreskin, releasing a small amount of urine into the toilet, stop urination;
- holding the foreskin, bring the container for collecting urine to the external opening of the urethra, without touching it with the head of the penis, and fill the container to the desired level (20-40 ml is required for analysis);
- tightly closing the container with a lid, transfer it to the laboratory; if it is not possible to quickly deliver the urine, you can place it in the refrigerator, but store it for no more than 1 day.
It is necessary to wash your hands thoroughly with soap.
Reviews about the treatment
Male cystitis, as a rule, is a consequence of prostatitis or urethritis, so the symptoms disappear after proper treatment of prostate inflammation. The forums discuss mainly chronic forms that do not respond to standard treatment methods. They give different advice:
Most men succeed in transferring chronic cystitis into stable remission by adjusting their lifestyle and increasing immunity.
Male discharge with cystitis
Men can also get cystitis. It often accompanies prostate diseases. As with the female half of the population, clear discharge is the norm.
The appearance of profuse leucorrhoea may be evidence of cystitis complicated by urethritis. If they are accompanied by mild itching, this is a clear sign of candidiasis. With chills and pus, this can be either a sexually transmitted disease or a sign of prostatitis. Bloody or brownish discharge indicates severe cystitis and possibly pyelonephritis.
How long does it take to treat inflammation?
Acute cystitis of a bacterial nature is treated with antibiotics for no more than 5-7 days. When inflammation is chronic, the course duration is 1-3 months. If complications arise, therapy is carried out in a hospital setting.
For a wrinkled bladder, surgical plastic surgery is performed to replace the damaged area with intestine. The rehabilitation period takes from 3-4 weeks to several months. To speed up the healing of the bladder, physiotherapy is prescribed - inductothermy, UHF, magnetic therapy.