A patient with diabetes insipidus constantly feels thirsty and, accordingly, produces a large amount of urine, which has a low specific gravity, due to the lack of the required amount of glucose. Even if you limit your water intake, urine will be released copiously. The disease is quite rare and is diagnosed in 1 in 25,000 people; both women and men, aged 40 to 50, suffer from the disease equally.
Diabetes insipidus occurs in humans due to impaired secretion of antidiuretic hormone. In addition, the cause of the development of the disease may be reduced sensitivity of the kidneys to the action of the hormone. The causes of the disease are benign and malignant tumors that arise due to pathologies of the hypothalamus. Diabetes insipidus can be a consequence of poorly performed operations when brain cells were affected.
Classification of diabetes insipidus
In addition to the congenital and acquired form of diabetes insipidus, the disease can have other forms, such as: central diabetes insipidus, renal diabetes insipidus, idiopathic diabetes insipidus.
Central diabetes insipidus
This form of diabetes insipidus is also called hypothalamic-pituitary. The disease develops as a result of the fact that the kidneys cannot accumulate fluid due to improper functioning of the distal tubules of the nephron. As a result, the patient not only suffers from a constant feeling of thirst, but also from frequent urination. In cases where the patient has the opportunity to regularly quench his thirst, there will be no harm to his body. In a situation where it is not possible to drink water when necessary, a person begins to develop dehydration. If these symptoms are not eliminated in time, there is a high risk that the person will fall into a hypersomular coma. When the disease lasts for a long enough time, the kidneys begin to get used to antidiuretic drugs and become insensitive to medications. As a result of the fact that the patient drinks a lot of fluid, along with diabetes insipidus, other diseases develop, such as biliary dyskinesia, irritable bowel syndrome, and gastric prolapse. In this regard, it is recommended to begin treatment of this form of diabetes insipidus as early as possible.
Idiopathic diabetes insipidus
This form of diabetes insipidus occurs in 1/3 of patients. Idiopathic diabetes insipidus is extremely rare and may be inherited. During diagnosis, pituitary gland pathologies of the organ are not visualized.
Renal diabetes insipidus
A very rare form of diabetes insipidus, provoked by organic and receptor pathologies of the kidneys. If diabetes is diagnosed in a child, then most likely it is congenital. When diagnosed in an adult, the cause of renal diabetes insipidus may be renal failure.
Stages and stages of the disease
The clinical picture of diabetes insipidus implies the classification of this disease based on the severity without correction by drugs:
- for a mild degree of the disease, it is common to increase the daily volume of urine to 6-8 l;
- the average degree of this pathology is characterized by the release of daily urine in a volume of 8-14 l;
- severe diabetes insipidus is accompanied by daily urine excretion in a volume of more than 14 liters.
When using drug therapy, the following degrees of the disease are distinguished:
- compensatory stage: characterized by the absence of symptoms of thirst and an increase in the volume of daily urine;
- subcompensation stage: manifested by the presence of polyuria and the periodic appearance of a feeling of thirst;
- During the decompensation stage, there is a constant feeling of thirst and polyuria, even during therapy.
Complications of diabetes insipidus
The greatest danger in diabetes insipidus is dehydration, which causes the loss of a large amount of fluid excreted along with urine due to frequent urination. Also, as a result of dehydration, the patient develops diseases such as: tachycardia, general weakness, possible vomiting and disturbances in mental and emotional state. Complications may include blood thickening, neurological disorders, and hypotension, which can be life-threatening. However, even with severe dehydration, the patient continues to have a high level of fluid excretion from the body. Women may experience menstrual irregularities, and men may experience decreased libido. Also, due to frequent intake of liquids, sometimes quite cold, respiratory tract diseases may develop.
Diagnosis
A decrease in polyuria with an increase in the specific gravity of urine above 1.010 with the administration of vasopressin drugs is of diagnostic significance. In the renal form D. n. in children, administration of vasopressin does not reduce polyuria. However, characteristic symptoms and a sharp deterioration in the child’s condition when he is deprived of fluid make it possible to differentiate the forms of D. n. Differential diagnosis is carried out with diseases occurring with polyuria. Diabetes mellitus is differentiated on the basis of hyperglycemia, glycosuria, high specific gravity of urine (see Diabetes mellitus); with hron, kidney failure, protein and casts are found in the urine; hyperparathyroidism (see) and primary aldosteronism (see Aldosteroma) differ due to the characteristic wedge picture (with the first disease there is hypercalcemia, with the second - hypokalemia). Differential diagnosis with psychogenic polydipsia is difficult, in which thirst develops primarily, and polyuria develops secondary; in these cases, use a test with a dry diet or intravenous administration of 50 ml of 2.5% sodium chloride solution for 45 minutes. In the presence of psychogenic polyuria during the test, urine output decreases and its specific gravity increases (more than 1.020), while in patients with D. n. no such phenomena are observed. Given the possibility of dehydration, these tests are carried out only in a hospital setting. The diagnostic criterion is the adiurecrine inhalation test (see); at the same time, in patients with the central form of D. n. the amount of urine decreases, its specific gravity increases to 1.010-1.015, and in the renal form there is no reaction to adiurecrin.
Prognosis for diabetes insipidus
The prognosis of diabetes insipidus mainly depends on what form is diagnosed in the patient. The majority of patients with diabetes insipidus have a favorable prognosis for life, but not for recovery. Diabetes insipidus does not affect performance or life expectancy, but can significantly reduce its quality. With severe diabetes insipidus, most patients are assigned disability group 3. If diabetes insipidus is symptomatic, then when the cause is eliminated, recovery occurs. If the disease was caused by an injury, then after treatment it is possible to restore the functions of the pituitary gland. If diabetes insipidus is not treated, dehydration will cause the development of stupor and subsequent coma.
Treatment
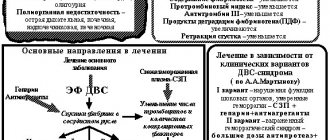
When patol is recognized, the process leading to D. n., etiol, treatment is carried out: for a tumor - its removal or radiation therapy, for hypothalamic syndrome - appropriate treatment; recovery after specific therapy for D. n. is described. syphilitic, tuberculosis and malarial etiology. Recovery is described in hypothalamic syndrome with D. n., caused by an acute respiratory infection after the use of antibiotics and intravenous administration of hexamethylenetetramine: penicillin 60,000 units and intravenous administration of 40% hexamethylenetetramine solution, 10.0 ml for 6-10 days.
In case of idiopathic form or lack of effect from anti-inflammatory therapy, vasopressin drugs are prescribed. Adiurecrin is inhaled at a dose of 0.03-0.05 g 2-4 times a day; in case of inflammation in the nasal cavity, pituitrin injections are prescribed under the skin or into the muscles at a rate of 0.5-1.0 ml (5-10 units) every 8-12 hours An oil suspension of vasopressin tannate is also used, 0.2-0.6 ml (1-3 units) into the muscles once every 1-3 days. The effect is achieved after 1-2 weeks, after which the dose is reduced. Saluretics can have a moderate symptomatic effect (paradoxical effect); hypothiazide is prescribed 50-100 mg per day; with long-term therapy, potassium salts are required. The mechanism of action of saluretics is not clear. In some patients, the use of chlorpropamide at a dose of 0.125-0.5, occasionally 0.75 g per day is effective. Administration of chlorpropamide reduces the reabsorption of water in the renal tubules. It is believed that its action is due to increased activity of small amounts of vasopressin. Hypoglycemia is possible when using chlorpropamide. It is most advisable to prescribe chlorpropamide for a combination of diabetes insipidus and diabetes mellitus.
For children, adiurecrin and pituitrin are dosed depending on age. At the age of 3 to 7 years, adiurecrin is prescribed at 0.01-0.02 g, from 7 to 12 years - 0.02-0.03 g, over 12 years - 0.03-0.04 g (2-3 inhale once a day). Children under 3 years of age are prescribed adiurecrine ointment containing 100 units per 1 g (0.1-0.2 g 2-3 times a day in the nasal cavity). Pituitrin is used for children (containing 5 units in 1 ml) at the age of up to 1 year - 0.1 - 0.15 ml, 2-5 years - 0.2-0.4 ml, 6-12 years - 0 .4-0.6 ml (1-2 times a day under the skin or into the muscles). Pathogenetic treatment of the renal form D. n. not developed; with the help of sulfonamide diuretics it is possible to significantly reduce diuresis; To prevent dehydration, children are allowed to drink liquids without restriction.
Reasons for development
There are a number of etiological factors under the influence of which diabetes insipidus occurs. More details about each.
Genetic causes
All about type 1 diabetes
Central hereditary diabetes insipidus develops as a result of mutations in the vasopressin gene or against the background of abnormalities in the structure of the midbrain. Symptoms of this form of the disease are noticeable already during the first five years of the baby’s life. With age, the pathology progresses, and vasopressin secretion levels decrease.
Important! There are known clinical cases of a sharp improvement in the condition of sick women and men over the age of 40 years.
Lack of the hormone may be part of a hereditary syndrome, which, in addition to diabetes insipidus, includes diabetes mellitus, deafness, and optic nerve atrophy.
Primary bedwetting
Children have high levels of hormonally active substances at night, which reduces the amount of urine. In sick children with primary bedwetting, the amount of antidiuretic hormone decreases sharply at night, and accordingly, a large amount of diluted urine is excreted.
Traumatic brain injury
A number of injuries (for example, a fracture of the base of the skull, a fracture of the sella turcica) can cause the development of swelling around the cells responsible for the production of the hormone. Insufficiency of synthesis can be temporary or persistent. In some patients, signs of the disease appear no earlier than 1-1.5 months after the injury.
Surgical interventions
Surgeries to remove pituitary adenoma, metastases, and craniopharyngioma are a common cause of diabetes insipidus. The specialist must distinguish between the occurrence of pathology and the physiological process of removing fluid that entered the body through infusions during surgery.
Important! Both development options are accompanied by a large amount of diluted urine excreted, however, in the case of disease, the osmotic concentration of the blood will be higher than normal.
Tumors
A common cause is dysgerminoma. To cause the disease, the tumor must be significant in size or located directly in the place where the largest number of cells responsible for the secretion of vasopressin are localized. Diabetes insipidus can develop when the hypothalamus is damaged by metastases against the background of kidney, lung, or breast cancer.
Endocrinologist – assistant in the fight against pathology
Neuroinfections
The reasons for the development of the type of pathology insipidus are meningococcal, cryptococcal infections, toxoplasmosis, cytomegalovirus, which involve the base and membranes of the brain in the process.
Diagnostics
- Low relative density of urine (if the value is more than 1005, the diagnosis can be reliably excluded).
- Urine hypoosmolarity (<300 mOsm/kg).
- Blood sugar: normoglycemia (exclusion of diabetes mellitus).
- Dry eating test: abstaining from liquids for 8–12 hours. In the case of diabetes insipidus, there is a weight loss of more than 5% and there is no increase in the relative density and osmolarity of urine (< 300 mOsm/kg).
- X-ray of the skull, MRI of the brain to exclude a space-occupying lesion in the hypothalamic-pituitary region.
Features of anatomy and physiology
The kidneys are a paired organ located behind the posterior abdominal wall at the level of the lower thoracic and upper lumbar vertebrae. The organ has a fibrous membrane, a fatty capsule and renal fascia. There is a conditional division of the kidney into two parts:
- organ parenchyma - its functions include the process of blood filtration and urine formation;
- pelvis - accumulates and removes urine from the body.
Each kidney has a huge number of nephron structural units that provide its functionality. The nephron has the following structure:
- The glomerulus is represented by a close plexus of capillaries through which blood flows. The glomerulus is immersed in the Shumlyansky-Bowman capsule.
- The capsule has two walls, and there is free space between them. The capsule passes into the cavity of the tubules.
- The tubules are located in the form of loops in the thickness of the renal parenchyma.
Nephron is the smallest structural unit of the kidneys
Functions
The kidneys remove excess fluid from the human body, metabolic metabolites of allergens, toxic and poisonous substances, and medications. In addition, the organ is involved in regulating water-salt balance, blood acidity, and pressure.
Important! Such processes are achieved through the formation of urine.
Urine is formed as follows. Arterial blood is filtered in the glomeruli of nephrons. Here the blood flow becomes slow due to the high pressure in the kidney artery and the difference in the size of the vessels. The filtered plasma enters the capsule along with toxins, unnecessary substances, glucose, and amino acids. The kidney vessels do not allow proteins and other large molecular compounds to pass through.
Further, in the urinary tubules of the nephrons, the reabsorption of water and substances necessary for the body occurs. Unnecessary substances accumulate and enter the urine excretion system (collecting ducts, pelvis, and then into the ureters and bladder).
What is the action of vasopressin?
Vasopressin is a hormone of the hypothalamic-pituitary system that is involved in the process of urine formation. The amount produced is regulated using the trace element sodium. Its quantitative increase in the body increases the synthesis of the hormone, while its decrease slows it down.
Under the influence of vasopressin, reabsorption of water and nutrients from primary urine occurs.
Hormone functions:
- ensures contraction of nephron vessels;
- maintains optimal pressure level;
- improves blood clotting rates;
- controls the production of a number of other hormones;
- controls the osmotic concentration of biological fluids;
- stimulates RATS.
Model of the vasopressin molecule – an antidiuretic hormone, the deficiency of which leads to the development of the disease
Important! A deficiency of the hormone vasopressin leads to the development of a disease such as diabetes insipidus. Moreover, such a pathology can occur not only in people, but also in animals (for example, cats, dogs).