Achalasia
is a motility disorder of the digestive tract where nerve cells and muscles do not work properly. The disorder can lead to difficulty swallowing, chest pain, regurgitation, coughing, and breathing problems if food enters the lungs.
Achalasia can affect any part of the digestive tract, including the intestines. Hirschsprung's disease is also a type of achalasia. Patients are usually diagnosed between the ages of 25 and 60. The disorder occurs in one in 100,000 people.
The cause is unknown and there is no cure, but treatment may provide relief.
Introduction
Achalasia (cardiospasm, achalasia cardia) is a rare disease of the esophagus that causes the lower part of the esophagus to lose the ability to swallow food. Result: Swallowing becomes increasingly problematic, causing people to feel as if food is getting stuck in their throat.
If the dysfunction develops as primary achalasia on its own, the nerve cells that normally control the precise movements of the esophagus during swallowing fail. The exact reasons for this are still unknown.
Accordingly, doctors also call primary achalasia idiopathic (that is, without an apparent cause). However, there is some evidence that inherited autoimmune processes are behind the disease.
Rarely, esophageal dysfunction also occurs as a result of another disease (called secondary achalasia or pseudoachalasia): for example, esophageal cancer or stomach cancer, as well as a tropical disease called Chagas disease.
In most cases, achalasia cardia occurs in middle age. Its typical symptoms:
- swallowing disorders (dysphagia);
- belching of undigested food debris (regurgitation);
- chest pain behind the breast bone.
At first, the symptoms are mild and appear only occasionally. Only later does achalasia become more noticeable: then the process of eating is increasingly disrupted, which can lead to gradual weight loss.
In some cases, pneumonia comes to the fore, which can be caused by food debris being pushed out and entering the respiratory tract.
In order to determine the symptoms associated with achalasia, endoscopy of the esophagus is recommended. Measurement of pressure in the esophagus (so-called manometry) and X-ray examination with a contrast medium are also important for diagnosis.
Various methods can be used to treat achalasia. They all pursue the same goal: to reduce pressure in the lower esophageal sphincter and thereby ensure the rapid and complete passage of food from the esophagus to the stomach. This helps relieve symptoms.
To treat mild achalasia initially, medications are sufficient. However, widening (or dilating) the muscles of the lower esophagus through surgery usually produces better treatment results and long-term results. However, cardiospasm cannot be completely cured.
Definition
Achalasia, also called cardiospasm, achalasia cardia, is a motility disorder of the esophagus, i.e. The ability of the esophagus to move (motility) is impaired. This problem is defined as follows:
- The lower esophageal sphincter in patients is in a state of increased tension, so it does not weaken when swallowing food, unlike healthy people.
- At the same time, the movements of the middle and lower esophagus that transport food (so-called peristalsis) decrease.
The esophagus is a muscular tube lined on the inside with mucous membrane.
Inside the muscle layer are interconnected nerve cells (the so-called Auerbach plexus). They control the precise movement of the esophagus during swallowing. These movements transfer food completely from the mouth to the stomach. The acidic environment disinfects food, mixes it with enzymes and destroys it.
The lower esophageal sphincter (gastroesophageal sphincter) between the stomach and esophagus, like a valve, prevents food and aggressive hydrochloric acid from returning to the esophagus: it ensures muscle contraction, responsible for their tension and relaxation, so that food entering the stomach does not return the contents of the stomach back.
In achalasia, the lower esophageal sphincter is unable to relax due to failure of the Auerbach plexus.
Thus, the gastric duct in achalasia is so tightly closed that food cannot completely enter the stomach - the food literally gets stuck in the throat. This causes increased pressure in the esophagus and leads to its expansion.
A little anatomy
Anatomically, the entire esophagus is divided into 3 parts:
- cervical,
- chest,
- abdominal
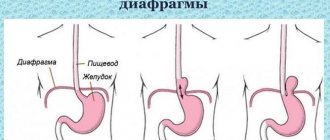
We are interested in the lowest part, starting from the entrance to the diaphragm and connecting to the stomach. The short diaphragmatic section (15–25 mm long) is located at the level of the IX-X thoracic vertebrae, anterior and slightly to the left of the middle.
The muscles of the diaphragm form one of the physiological narrowings of the esophagus. Together with fibrous tissue and loose fiber, it is represented by a ring that hermetically closes the entrance to the cardia (the part adjacent to the stomach). At rest, the diaphragmatic area is closed, there is no lumen.
Features of the structure and functioning of the esophagus
The subphrenic part of the cardia is 30–40 mm long, extends from the dome of the diaphragm behind the left lobe of the liver, and is covered in front and side by the peritoneum. The lower border of the cardia is determined by the angle formed by the greater curvature of the stomach and the lateral wall of the esophagus (the angle of His).
The degree of readiness of the esophagus to prevent regurgitation (return of food) depends on the sharpness of the angle. On the inside, at the border, there is a fold of mucous membrane that plays the role of a valve. The parasympathetic innervation of the esophagus forms a complex network:
- anterior - mainly from fibers of the right vagus nerve
- back - from the left.
The main task of the vagus nerve is to ensure motor activity of the esophagus.
Sympathetic signals enter the ganglia (nodes) and are connected to the nerve fibers of the lungs, heart, aorta, and solar plexus. They are responsible for the tone of the esophageal wall. In addition, the mobility of the cardia is controlled by the internal nervous apparatus, located in the submucosal layer, adventitia, between the muscle fibers.
Causes of achalasia
Depending on the reasons for the development of achalasia, doctors call esophageal disorders primary (or idiopathic, i.e. occurring for no apparent reason) or secondary (i.e. as a result of other diseases).
The cause of primary achalasia is that nerve cells in the nerve network (called Auerbach's plexus or Meissner's plexus) die in the area of the lower esophagus. This so-called neurodegeneration means that the muscles of the esophagus are no longer sufficiently supplied with nerves. Subsequently:
- The lower esophageal sphincter (called the gastroesophageal sphincter) cannot relax when swallowing and
- The ability of the middle and lower esophagus to contract and, therefore, facilitate the transport of food is reduced.
The exact causes of neurodegenerative disorders are not yet clear. It is likely that primary achalasia is an autoimmune disease and, therefore, those affected have a hereditary predisposition to it. On the other hand, achalasia can occur due to other problems, for example:
- Down syndrome: anyone born with a genetic change (called trisomy 21) has a 200-fold risk of developing achalasia;
- Sjögren's syndrome;
- systemic lupus erythematosus;
- triple syndrome (AAA): In addition to achalasia, this rare inherited disorder is associated with Addison's disease (a disease of the adrenal cortex) and alacrymia (decreased or absent tearing).
However, in most cases, primary achalasia occurs on its own, i.e. not as part of a syndrome.
In rare cases, other diseases can cause esophageal dysfunction. Thus, secondary achalasia can occur, for example, in the chronic stage of Chagas disease, a tropical disease of South America.
If secondary achalasia develops as a result of a disease that is not associated with Auerbach's plexus, it is also called pseudo-achalasia.
The most common cause of pseudo-achalasia is a narrowing of the junction between the esophagus and the stomach: it is usually caused by tumors of the esophagus (called esophageal carcinoma) or stomach (gastric carcinoma).
Advantages of treatment at the Swiss University Hospital
- The clinic is equipped with the latest generation equipment, which allows the operation to be performed without damaging nearby structures, the muscularis mucosa is dissected without damaging the mucosa, intraoperative complications are also excluded, etc.
- The treatment method is selected for each patient individually, taking into account his state of health. Great importance is given to preserving the natural anatomical location of the esophagus, diaphragm and stomach, which avoids the occurrence of reflux esophagitis and sphincter insufficiency in the future.
- When treating patients, the clinic uses a technique that makes it unnecessary to leave a transgastric tube after surgery, which makes the postoperative course easier. Thanks to the original method used, the risk of further relapse is minimal; in more than 97% of patients, good results were achieved, confirmed by fibroesophagogastroduodenoscopy, X-ray examination and esophagomanometry.
- In our clinic, patients with several diseases requiring surgical treatment can undergo simultaneous surgery. Performing several surgical interventions during one anesthesia reduces the burden on the body, hospitalization time, and recovery, compared to conventional surgery, takes much less time.
Difficulty swallowing and other symptoms of achalasia
Typical symptoms of achalasia:
- dysphagia (swallowing disorders);
- regurgitation (regurgitation) of undigested food;
- pain in the chest area.
At first, achalasia is mild and rare. Only with the further course of the disease, the symptoms gradually intensify and begin to have a negative impact in everyday life.
Swallowing disorders are the first signs of achalasia. First of all, it occurs mainly when swallowing solid food: victims feel that the food is stuck in the throat and often drink it down so that the food can pass.
With progressive achalasia, liquid food is also difficult to swallow. In addition, in the later stages, spontaneous regurgitation (when food particles pass from the esophagus back into the oral cavity) occurs in the supine position. There is a risk of food particles getting into the airways, which can cause inflammation of the lungs (called aspiration pneumonia).
Progressive achalasia can lead to pneumonia many times over.
Achalasia can also be accompanied by spasmodic chest pain, which patients sometimes misinterpret as heart pain.
Because the disease interferes with eating, patients often lose weight over time: as a rule, patients slowly lose a maximum of ten percent of their original weight. This happens over a period of several months to several years.
Diagnostics
With achalasia, diagnosis can only be made years after the first symptoms appear. Reason: In the early stages, esophageal dysfunction usually causes few characteristic symptoms.
Various examinations of the esophagus are suitable for diagnosing achalasia. These include:
- endoscopic examination;
- manometry (measurement of pressure in organs);
- X-ray examination.
Endoscopy
Under certain circumstances, achalasia may be indicated by food debris, inflammation, or visible narrowing of the lower esophagus. Endoscopy, i.e. examination of the esophagus and stomach with an endoscope is especially necessary for making a diagnosis in order to exclude other possible causes of complaints (for example, esophageal cancer).
In some cases, the doctor will also take tissue samples during this test to check for changes and abnormalities (called a biopsy).
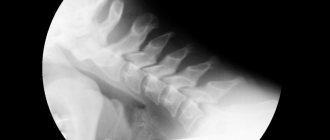
X-ray
To evaluate achalasia on an x-ray, you are given a contrast agent before the x-ray examination, which helps you see the esophagus during diagnosis.
Manometry
Manometry is also useful in cases of suspected achalasia: manometry allows the doctor to measure the pressure in the esophagus. If the lower esophageal sphincter does not relax when swallowing, this indicates achalasia.
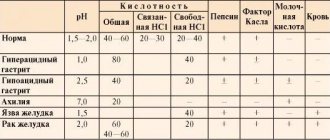
Manometry allows us to draw conclusions about the mobility of the esophagus (peristalsis). Depending on the mobility of the esophageal muscles, three forms of achalasia are distinguished:
- hypermotile form: increased peristalsis;
- hypotonic form: reduced peristalsis;
- mobile form: no more peristalsis.
Causes and factors of the disease
It is impossible to name the specific cause of the disease, but provoking factors are known. These include:
- hereditary predisposition - confirmed by identifying cases in one family; there may be congenital defects in the innervation of the esophagus;
- past infection - a proven connection with infection with herpes viruses, chickenpox, cytomegalovirus;
- lack of nutritional vitamins (especially group B), protein;
- past stressful situations, mental trauma, constant overexertion.
Treatment of achalasia
Once the disease is detected, therapy is necessary. Treatment is aimed at relieving symptoms of esophageal dysfunction. There are various treatment methods for this, but they all have the same goal:
- decreased pressure in the lower esophageal sphincter - the valve between the stomach and esophagus,
- so that food quickly and completely passes from the esophagus to the stomach.
However, the cause of achalasia cannot be eliminated: it is impossible to correct the impaired nervous system of the esophageal muscles. By this we want to say that the disease cannot be cured.
Drug therapy
In the early stages of achalasia, medications that reduce pressure in the lower part of the esophagus and thus significantly alleviate the symptoms of the disease are suitable for treatment.
Drugs that are used for high blood pressure and coronary heart disease are also suitable: calcium antagonists and nitrates.
The drug should be taken about half an hour before meals.
However, in the long term, the effect of the drugs decreases; in this case, other methods should be considered to treat achalasia.
If the medications used cause side effects (low blood pressure, dizziness, headaches), you may have to stop taking the medications.
Balloon dilatation
For achalasia, therapy can also be carried out using balloon dilatation (expansion). This is a special endoscopic instrument that the doctor inserts into the esophagus and stomach. This procedure mechanically widens the narrowed lower esophageal muscle.
Balloon dilation is considered the most effective non-surgical treatment for achalasia: after a single injection, signs of swallowing disorders improve for several months in most cases, and even for several years in half. Repeated dilatation may then be required.
However, especially in children and adolescents, the effect after treatment only lasts for a short time.
The advantage of treating achalasia with balloon dilatation is that the procedure is performed during refraction of the esophagus and stomach, and does not require surgery. However, complications may occur during treatment: the esophagus may rupture during dilatation (3%).
Features of the disease in children
Among all cases of esophageal achalasia, children under 15 years of age account for 5%. It has been established that motility disorders occur not only in the esophagus, but also in the intestines, stomach, and gall bladder. More often, the disease manifests itself after five years of age, with maximum incidence occurring at 8–9 years of age.
The most common symptoms are:
- vomiting during meals or a little later (in 80% of cases);
- difficulty swallowing (in 76% of cases);
- cough at night;
- baby crying in pain.
If the disease begins in infancy, then the mother notices that while feeding the child she vomits uncurdled milk, there is no admixture of gastric contents. The baby “chokes” due to insufficient peristalsis in the lower segment of the esophagus and the cardiac sphincter remaining in a closed position. Difficulties in getting food cause retardation in physical development, vitamin deficiency, and frequent bronchopneumonia.
Forecast and course
Achalasia is a chronic disease - spontaneous recovery does not occur when the function of the esophagus is impaired. Typically, swallowing disorders develop slowly and steadily over many years or decades. However, with appropriate treatment, symptoms can usually be satisfactorily relieved. Unfortunately, the disease cannot be completely cured.
However, if achalasia is not treated at all, the esophagus will expand more and more (the so-called dilatation, this is a disease, not a procedure) - to the so-called megaesophagus with a complete loss of esophageal function.
In addition, in the later stage (due to typical belching), lung complications or inflammation of the esophagus (due to food remaining in the esophagus for a long time) may occur, which in turn can lead to ulcers or bleeding.
Achalasia is generally associated with an increased risk of cancer, with approximately 4 to 6 percent of patients developing esophageal cancer (esophageal carcinoma) many years later.
Thus, the risk of developing esophageal cancer with achalasia is approximately 30 times higher. Therefore, regular endoscopic examinations are important for follow-up care.
Esophageal achalasia - dietary recommendations
The patient will require a liquid diet for the first few days after treatment. As swallowing becomes easier, they can transition to a solid diet. Patients should eat slowly, chew food thoroughly, and drink plenty of water with meals.
You should not eat food before bed. You should sleep with your head elevated so that food does not linger in the esophagus.
Foods to avoid include citrus fruits, alcohol, caffeine, chocolate and ketchup as they promote reflux. Fatty and spicy foods can also irritate the digestive system and worsen symptoms.
- Foods that may help: Soft foods such as soups, purees or porridge;
- Ginger can aid digestion and prevent heartburn;
- Peppermint in teas and yogurts may reduce gastric secretions;
- You should drink at least 10 glasses of water daily.
It is important to maintain a balanced diet that contains all the nutrients and fiber needed for a healthy lifestyle.
Prevention and recommendations
You cannot prevent achalasia because the exact cause of esophageal dysfunction is unknown. However, if you are one of those affected, you can reduce the risk of some common underlying conditions (such as esophagitis) by avoiding alcohol and nicotine, for example.
In addition, in the case of achalasia, regular endoscopic examination of the esophagus is recommended for follow-up in order to detect possible late complications (especially esophageal cancer) at an early stage.
Prices
| Disease | Approximate price, $ |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing Crohn's disease | 3 560 — 4 120 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for hepatitis C diagnostics | 5 700 — 6 300 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for colorectal cancer treatment | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of nonspecific ulcerative colitis | 5 670 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of gallstone disease | 9 000 — 11 950 |
| Prices for the treatment of gastroenterological diseases | 4 990 — 8 490 |
| Prices for diagnosing Crohn's disease | 5 730 — 9 590 |
| Prices for treatment of viral hepatitis C and B | 5 380 — 7 580 |
| Prices for treatment of gastrointestinal cancer | 4 700 — 6 200 |