Acute coronary syndrome (ACS) is a serious condition caused by impaired coronary circulation and myocardial ischemia. When the blood supply to the heart muscle completely stops, hypoxia occurs, which is the direct cause of heart attack and death. This deadly pathological process is popularly called a pre-infarction condition or a heart attack. ACS is a general concept that includes a number of processes that are equal in origin and similar in course, but differ in prognosis and likelihood of cure.
Diseases of the cardiovascular system, which are based on coronary insufficiency syndrome, are designated by the term ACS. This is what clinicians call heart diseases in which its blood supply deteriorates: myocardial infarction and unstable angina. These diseases have similar initial manifestations, pathophysiological mechanisms and some treatment principles. That is why the concept of “acute coronary syndrome” was introduced into medical practice. It is used to make a preliminary diagnosis, when all the characteristics of the patient’s pathological process are not fully clarified.
Acute coronary syndrome has an ICD-10 code of 124.9 and the name “Acute coronary heart disease, unspecified.” The causes of the pathology most often are: thrombosis and thromboembolism caused by rupture of an atherosclerotic plaque or erosion of the endothelium of the coronary artery. There is a special form of the syndrome that is of allergic origin. It is associated with excess production of inflammatory mediators by mast cells. Symptoms of the syndrome are: shortness of breath, irregular heart rhythm, pressing chest pain that occurs at rest or with minor physical stress. The most dangerous sign of ACS is sudden cardiac arrest. This diagnosis is usually made in the intensive care unit.
Coronary disease occurs with pronounced periods of exacerbation and remission. IHD worsens under the influence of provoking factors. In this case, its mild form develops - unstable angina or a severe form - myocardial infarction. In the first case, acute ischemia of the heart muscle does not lead to necrosis. Due to narrowing or blockage of the coronary arteries, trophic changes occur that develop gradually, slowly, in steps. After exposure to the trigger factor, an attack of ACS occurs. With myocardial infarction, irreversible cell death occurs. This pathology is much more dangerous - it is accompanied by severe chest pain, impaired breathing and consciousness, and an avalanche-like death of cardiomyocytes. Destruction of large areas is manifested by the most severe symptoms. With angina pectoris, there are no ECG signs of myocardial necrosis and specific biochemical markers in the blood. It is possible to transition from one clinical form of IHD to another.
The characteristic clinical picture of the syndrome allows you to quickly make a diagnosis and help the patient. To save his life, you should know the algorithm for providing emergency medical care and be able to carry out all the necessary measures before the arrival of qualified specialists. Emergency treatment of ACS will help avoid the development of serious complications and death. It is effective only if diagnosed early. General therapeutic measures prescribed to patients depend on clinical manifestations, the severity of pathological changes and the general well-being of the patient.
Currently, acute coronary syndrome is a pressing medical problem. This is due to the high frequency of its occurrence and the need for preventive measures. The development and implementation of a new medical strategy can save the lives of patients with ACS.
Anatomy of the myocardial circulatory system
Oxygen-enriched blood enters the myocardium (heart muscle) through arteries located in the form of a crown on its surface, and venous blood, with a high content of carbon dioxide and metabolic products, is discharged through the veins. It is precisely due to the similarity with the royal attribute that the coronary vessels of the heart were called “coronary” in the Russian version, and in the Latin accepted in medicine - “coronary” (from “corona” - crown). The great Leonardo da Vinci made the first anatomical sketches of human organs, and he came up with some such poetic names.
Let’s move on from lyrics to utilitarian comparisons, so that complex things become simpler and clearer. So, the wall of any artery has a unique standard of structure, similar to the familiar braided water hose. On the outside there is a dense layer of connective tissue, then there is the muscle part, it is able to contract and relax, creating a pulse wave and helping blood flow. Then the inner lining, the thinnest and perfectly smooth intima, or endothelium, improves blood flow by reducing friction. It is with this that the problems of most “heart” patients are associated. Coronary heart disease, in an anatomical sense, begins with damage to the inner lining of the coronary arteries.
In case of lipid metabolism disorders, cholesterol can accumulate at the border of the muscle layer and intima and form conglomerates - soft cholesterol plaques. The endothelium above them rises and thins, as a result, a thin layer of cells breaks through and forms an elevation inside the artery.
The blood flow gives local turbulence and slows down, creating conditions for new deposits and precipitation of insoluble calcium salts - their calcification. Such “grown” plaques, with uneven and hard calcifications, are already very dangerous: they can ulcerate, damaging the muscular layer of the arteries; Thrombotic masses are deposited on them, reducing the lumen until it is completely blocked. The result is ischemia, angina, heart attack, this is the sequence in which events develop.
Possible complications
Possible consequences include:
- Heart failure.
- Heart attack, primary or repeated. Each new one carries a great danger to life.
- Stroke. Poor circulation in brain structures with tissue necrosis.
- Cardiogenic shock. Blood pressure drops to critically low levels. Mortality is close to 100%.
Sudden death or at least disability without treatment is expected within a few years or less.
Reasons for the development of ACS
The mechanisms of development (pathogenesis) are the same for all ischemic, that is, associated with a lack of oxygen, heart diseases, including acute coronary syndrome. There are only two reasons that disrupt the normal movement of blood through the arteries: a change in the tone of the arteries and a decrease in their lumen.
1. Spasm of the vascular wall can occur from an increased release of adrenaline, for example in a stressful situation. The expression “the heart sank in the chest” accurately describes the state of a person with a short-term attack of ischemia. A short-term lack of oxygen is easily compensated for: the heart rate (HR) increases, blood flow increases, oxygen flow increases, well-being and mood become even better.
People who are passionate about extreme sports and recreation constantly receive short adrenaline “attacks” on the heart and associated pleasant sensations - joyful excitement, an influx of energy. A physiological bonus of any, even small, loads is a decrease in the sensitivity of the coronary vessels to spasm, and therefore the prevention of ischemia.
If the stressful situation is prolonged (the time varies depending on the “training” of the heart), then the decompensation phase begins. Muscle cells use up emergency energy reserves, the heart begins to beat slower and weaker, carbon dioxide accumulates and reduces the tone of the arteries, and blood flow in the coronary arteries slows down. Accordingly, the metabolism in the heart muscle is disrupted, part of it may become dead (necrosis). Foci of necrosis of the muscular wall of the heart are called myocardial infarction.
2. A decrease in the lumen of the coronary arteries is associated either with disturbances in the normal state of their inner lining, or with the blocking of blood flow by a thrombus (blood clot, atherosclerotic plaque). The frequency of the problem depends on risk factors, which, with prolonged exposure, lead to metabolic disorders and the formation of blood clots.
Main external factors:
- Smoking – general intoxication, disruption of the cells of the inner layer of arteries, increased risk of blood clots;
- Unbalanced diet – increased lipid levels in the blood; inadequate intake of proteins to the body’s needs; changing the balance of vitamins and microelements; metabolic imbalance;
- Low physical activity - “untrained” heart, decreased force of heart contractions, venous congestion, deterioration of oxygen supply to tissues, accumulation of carbon dioxide in them;
- Stress – constantly increased adrenaline levels, prolonged arterial spasm.
Agree, the name “external” is no coincidence; their level can be lowered or increased by the person himself, just by changing his lifestyle, habits and emotional attitude to what is happening.
Over time, the quantitative effect of risks accumulates and transforms into qualitative changes - diseases that are already considered internal risk factors for acute coronary insufficiency:
- Heredity - structural features of blood vessels, metabolic processes are also transmitted from parents, but as relative risk factors. That is, they can be either aggravated or significantly reduced by avoiding external factors.
- A persistent increase in lipids in the blood and atherosclerosis - deposits in the arteries in the form of atherosclerotic plaques with narrowing of the lumen, myocardial ischemia.
- Obesity - an increase in the total length of blood vessels, increased load on the heart, thickening of the muscle wall (myocardial hypertrophy).
- Arterial hypertension - consistently high blood pressure, changes in the walls of the arteries (sclerosation) with a decrease in their elasticity, congestive manifestations - edema
- Diabetes mellitus - blood viscosity increases and the risk of blood clots forms; changes in arterioles (the smallest arterial vessels) lead to ischemia of organs, including the myocardium.
The combination of several factors increases the likelihood of blood clots that completely block the heart’s own arteries. The consequence of developments in this scenario will be sudden coronary death , the second most common outcome (after myocardial infarction) of acute coronary syndrome.
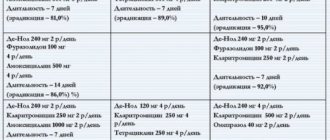
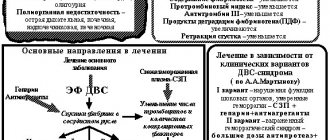
Antithrombotic therapy
Antithrombotic therapy is the cornerstone of treatment for patients with ACS. It includes two components: antiplatelet and anticoagulant therapy.
Antiplatelet therapy
Aspirin. It blocks the synthesis of thromboxane A2 by irreversibly inhibiting cyclooxygenase-1, thereby reducing platelet aggregation. The initial daily dose should be from 162 to 325 mg, and then reduced - from 75 to 162 mg. Used for long-term secondary prevention.
Clopidogrel is a recommended alternative for patients who are intolerant to aspirin. It reduces platelet activation and aggregation and reduces blood viscosity. The loading dose is 600 mg, the maintenance dose is 75 mg per day. Therapy with clopidogrel and aspirin is recommended for almost all patients with ACS.
Anticoagulant therapy
Anticoagulant therapy should begin as soon as possible after diagnosis. Today, the following drugs are used for its implementation: unfractionated heparin, enoxaparin, fondoparinux.
Unfractionated heparin (UFH). Several randomized trials suggest that UFH is associated with lower mortality rates than aspirin alone. But when prescribing it, it is necessary to monitor the activated partial thromboplastin time (PTT) to prevent hemorrhages.
Fondoparinux is a synthetic pentasaccharide that is an indirect factor Xa inhibitor and requires antithrombin to achieve a therapeutic effect. This drug is preferred over other anticoagulants for patients undergoing conservative therapy and in patients at increased risk of bleeding.
Lipid-lowering therapy
In the absence of contraindications, lipid-lowering therapy with statins should be initiated in all patients with ACS, regardless of baseline cholesterol and LDL cholesterol levels.
Thrombolysis therapy
It is carried out at the prehospital stage. If this is not possible, no later than 30 minutes after hospitalization. The following types of drugs are used:
Streptokinase – 1.5 million, OD IV over 30-60 minutes;- Alteplase - 15 mg IV bolus, 0.75 mg/kg body weight over 30 minutes, then 0.5 mg/kg over 60 minutes; the total dose should not exceed 100 mg;
- Tenectoplase - bolus IV administration of the drug depends on the patient’s weight: 30 mg for a weight less than 60 kg; 35 mg per 60-69kg; 40 mg for 70-79 kg; 45 mg for 80-89 kg; 50 mg for weight over 90 kg.
Surgeries to treat ACS
Surgical treatment of acute coronary syndrome is aimed at restoring blood circulation in the coronary arteries. Coronary artery bypass grafting and stenting allow this to be achieved. The essence of the first method is to create a bypass for arterial blood, avoiding the affected area. Thus, those parts of the heart that suffered from hypoxia begin to function normally again. The essence of stenting is to place a stent in the artery, which will expand the narrowed area and prevent further plaque growth.
Clinical forms of ACS and the degree of risk for the patient
There are two main forms of ACS:
- Unstable angina is chest pain characteristic of a heart attack, which appears for the first time or repeatedly, immediately after physical or emotional stress, or in a calm position.
- Myocardial infarction is death (necrosis) of the muscular wall of the heart. Depending on the area of the lesion, small-focal (microinfarction) and extensive are distinguished, according to localization - according to the accepted names of the walls of the heart - anterior, lateral, posterior diaphragmatic and interventricular septum. The main life-threatening complications are fatal arrhythmias and rupture of the heart wall.
Classification is important both for assessing the severity of the condition and for analyzing the level of risk of sudden coronary death (occurring no more than 6 hours from the onset of the attack).
High risk
presence of at least one of the following signs:
- An attack of angina for more than 20 minutes and to the present;
- Pulmonary edema (difficulty breathing, bubbling breathing, pinkish foamy sputum, forced sitting position);
- On the ECG: decrease or elevation of the ST segment more than 1 mm above the isoline;
- Angina pectoris with decreased pressure in the arteries;
- Laboratory: change in the level of markers of myocardial necrosis.
Medium risk
Discrepancy with high-risk items, or the presence of one of the mentioned signs:
- An attack of angina lasting less than 20 minutes, which stopped when taking nitroglycerin;
- Angina at rest for less than 20 minutes, which stopped after taking nitroglycerin;
- Nocturnal attacks of chest pain;
- Severe angina that first appeared within the last 14 days;
- Age over 65 years;
- On the ECG: dynamic changes in the T wave to normal, Q waves more than 3 mm, decreased ST segment at rest (in several leads).
Low risk
in case of discrepancy with the criteria for high and medium risk:
- More frequent and severe attacks than usual;
- Lower level of physical stress that causes an attack;
- Angina appeared for the first time, from 14 days to 2 months;
- On the ECG: a normal curve in accordance with age, or no new changes compared to previously obtained data.
Nitroglycerin and nitrates
Intravenous administration of nitrates on the first day of myocardial infarction is recommended if there are the following indications:
- acute left ventricular failure;
- early post-infarction angina;
- arterial hypertension;
- with extensive anterior myocardial infarction.
Start as early as possible if there is no arterial hypotension (blood pressure more than 90 mm Hg). The initial rate of nitroglycerin administration is 5-20 mcg per minute. The infusion rate should be selected individually, increasing the rate of administration by 5-10 mcg every five minutes (SBP should drop 10-15 mm Hg lower, but no more than 10% in normotensive patients, and no more than 25-30% in hypertensive patients) .
If blood pressure monitoring is available, it is more correct to use the mean arterial pressure value. With the correct infusion rate, it should decrease by 10-15% from the initial level. Should be administered over 18-24 hours. For signs of heart failure - until the condition stabilizes.
For patients with unstable angina, doctors prescribe intravenous nitroglycerin until anginal attacks at rest stop. After stabilization of the condition, they switch to oral administration of nitrates - isosorbide-5-mononitrate 40 mg twice a day (preferred) or isosorbide dinitrate (nitrosorbide) 10-20 mg 4 times a day.
How does acute coronary syndrome manifest?
The main symptoms of acute coronary insufficiency are few and characteristic of each form of ACS.
- The first and most important sign is severe, constant pain behind the sternum, squeezing, burning or squeezing in nature. The duration of an attack can vary from half an hour to several hours, but there are cases where patients endured pain that lasted more than a day. Many people complain of irradiation (conduction of pain impulses along local nerve endings) to the left upper part of the body - the shoulder blade, arm and hand (little finger area), neck and lower jaw. With myocardial infarction localized in the posterior diaphragmatic wall of the heart, painful sensations can be concentrated only in the region of the costal angle, at the junction of the ribs with the sternum.
- The pain begins either immediately after physical activity, or against the background of complete rest - at night or early in the morning, when the person is still lying in bed.
- The reaction of the nervous system to extreme stress: an excited and extremely restless state. Characteristic is a feeling of panicky fear of death, which only intensifies compared to the onset of the attack. Self-control is minimal, consciousness is confused.
- The skin is pale, cold sweat appears on the forehead. The patient feels a constant lack of air, tries to take a more comfortable position for inhalation (orthopnea), asks for a higher pillow or tries to sit down.
Rehabilitation and further observation of the patient
Cardiac rehabilitation includes:
- dietary counseling;
- prescribing a set of exercises;
- psychosocial support;
- to give up smoking;
The goal is to quickly and completely restore the body and reduce the likelihood of ACS recurrence. The rehabilitation program focuses on improving physical fitness, self-confidence and social integration. It is carried out with the help of a doctor, specialized physiotherapists, nurses and is divided into hospital and outpatient stages. In addition, constant consultations with the treating doctor are necessary.
What treatment can help before the doctor arrives?
- Emergency help: first of all, give a nitroglycerin tablet under the tongue: this area is rich in blood vessels; the active components are quickly absorbed through the mucous membrane and enter the blood. By acting on the muscular wall of the arteries, the drug relieves spasm of the coronary vessels of the heart and temporarily improves blood flow. If necessary, you can take 1 tablet every 5 to 10 minutes. Remember that a side effect of intensive use of nitroglycerin can be brain steal syndrome: dizziness, narrowing of the field of vision and darkening of the eyes, nausea. All these phenomena disappear within a couple of minutes, but it is better for the patient to lie down during this time.
- Aspirin, chew tablet, dosage 160 – 325 mg. Small concentrations of acetylsalicylic acid reduce blood clotting, so you can initially protect against an increase in the size of blood clots already formed in the coronary arteries.
- Oxygen – open a window and create a draft to help bring in fresh air. If possible, use a medical balloon; they are usually always ready for chronic patients. Supply gas through a humidifier, or put gauze, moistened with water and wrung out, into the mask: pure oxygen greatly dries out the mucous membranes.
Further treatment tactics are determined by the doctor; it depends on the final diagnosis made on the basis of electrocardiogram data and biochemical blood tests. Patients with acute coronary insufficiency must be hospitalized.
Classification
Typing is carried out according to a group of bases.
Based on the shape, they talk about two varieties:
- Unstable angina. Gradual, chronic malnutrition resulting from narrowing of the coronary arteries (much more common) or blockage.
Recovery requires long-term assistance. The pathological process itself is divided into 4 functional classes, they correspond to the severity of the disease.
The first is treated completely, starting with the second, it will no longer be possible to radically stop the condition. Lifelong therapy.
Unstable angina, a form of acute coronary syndrome, occurs in attacks, usually preceded by some trigger factor. From physical overexertion to hypothermia and others.
- Heart attack. In terms of severity, it is much more dangerous and characteristic. Accompanied by severe pain in the chest, impaired breathing and consciousness.
If angina pectoris develops slowly, stepwise, cardiomyocytes die in small groups, in this case the process is avalanche-like.
Destruction of large areas is possible. The wider the affected area, the more intense the symptoms.
After a certain time from the onset of this form of acute coronary syndrome, the phenomena subside.
Attention:
Imaginary prosperity should be perceived as an alarming sign, since destruction continues at a rapid pace.
The severity is partially affected by the clinical variant of the described condition:
- Primary form. Develops in patients who have not previously experienced angina attacks and have no history of heart attack.
- Progressive variety. Its essence lies in the aggravation of the main process. Usually the reason for this is a complication of the underlying disease, for example, atherosclerosis or an unhealthy lifestyle. Also lack of treatment or its insufficient effectiveness.
- Postoperative form. Accompanied by severe symptoms, but usually occurs over a short period of time. If the intervention is carried out incorrectly, a resistant variety may develop.
- Post-infarction type. Accompanies the rehabilitation period of an emergency condition. Requires mandatory correction, as it increases the risk of relapse.
- Spontaneous angina. The most dangerous from clinical point of view. Provokes frequent episodes of malnutrition in the short term. Up to 5-8 attacks can occur in a week.
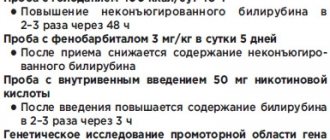
Diagnostic tests for ACS
Electrocardiogram and its values in various forms of ACS
- ST segment: without elevation, or labile or persistent depression of more than 2 mm, changes in the T wave. Against the background of pain in the heart, this variant on the ECG is characteristic of acute myocardial ischemia. If markers of myocardial necrosis are not detected in the blood, then the diagnosis of unstable angina is justified. The presence or detection of a dynamic increase in the level of markers indicates a small-focal myocardial infarction.
- ST segment: persistent elevation above the isoline of more than 2 mm, plus new conduction disorders (left bundle branch block), pain and increased markers, caused by acute coronary insufficiency, diagnosis - myocardial infarction.
Coronary angiography (coronography)
Injection of an X-ray contrast agent into the arteries, which allows you to visualize the coronary pattern and assess the degree of occlusion (overlap) of the vessels. The method has a leading place in the diagnosis of ischemic heart lesions. The risk of complications of the procedure is no more than 1%, there are no absolute contraindications, relative ones - acute renal failure, shock conditions.
Disadvantages: exposure to up to 6.5 mSv
Performing a coronography is possible only after making an appropriate entry in the medical history (a separate protocol) about the indications, and after the consent of the patient or his closest relatives.
Computed tomography (CT)
allows you to identify stenoses of the coronary arteries, atherosclerotic plaques of various sizes and densities. Disadvantage: The patient is asked to hold their breath for a few seconds to obtain high-quality images.
Electron beam CT: high temporal resolution, the required breath holding is only 1-2 seconds, scanning in layers of 1.5 - 3 mm, the entire heart is examined in 1-2 breathing pauses.
Multi-slice CT: An X-ray tube rotates rapidly around the patient, requiring only one breath-hold to obtain a complete image of the heart.
Disadvantages of the CT method: radiation (from 1 mSievert to 3.5 mSv), intravenous administration of iodine-containing contrast agent - contraindications for allergic reactions to iodine.
Cardiac MRI (magnetic resonance imaging)
MRI allows you to take layer-by-layer images with a wide view in any plane. Measurements of arterial blood flow and filling of the atria and ventricles are possible, the blood supply to the myocardium and the characteristics of heart contractions are assessed. The patient is not exposed to ionizing radiation (radiation) at all.
Establishing diagnosis
Patients with suspected ACS are examined, their complaints are analyzed, the heart is auscultated and percussed, and blood pressure and pulse are measured.
Electrocardiographic examination is the main diagnostic method for ACS. An ECG should be done as soon as possible after the onset of cardialgia. This technique involves recording the electrical activity of the heart using electrodes attached to the skin. First, electrical impulses in the form of waves are displayed on a monitor and then printed on paper. When the myocardium is damaged, its conductive function is impaired. The ECG shows the form of ACS - angina or heart attack.
As soon as the patient’s condition becomes satisfactory, you can move on to a full diagnostic program, including:
- 24-hour Holter monitoring – measuring blood pressure and pulse over 24 hours.
- General blood test, blood for hormones - general examination of the body.
- Clinical examination of urine to determine the functional state of the kidneys.
- BAC - detection of the level of cholesterol, glucose, as well as enzymes that, during the development of myocardial infarction, are released from damaged cardiomyocytes into the blood.
- Coagulogram is an assessment of the functional state of the blood coagulation system.
- Echocardiography is an ultrasound examination of the heart to detect lesions. Ultrasound waves are sent from the device's sensor to the heart and then returned back. The received signals are processed by a computer, and a video image is formed on the monitor screen.
- X-ray examination of the chest cavity - determining the size and shape of the heart and large blood vessels.
- Coronary angiography is an invasive test that identifies the location and extent of narrowing or occlusion of the coronary arteries. A long catheter is inserted into the heart vessels through the large arteries of the arms or legs. The vascular bed is filled with a liquid contrast agent and a series of x-rays are taken, in which the areas of narrowing are clearly visible. During the catheter procedure, the doctor can use tiny balloons to relieve the narrowing. They are introduced into the affected vessel and inflated. At the same time, the narrowing expands and the occlusion is eliminated. To prevent repeated spasm, a stent - a mesh tubular frame - is installed in the artery.
- Scintigraphy – detection of coronary blood flow disorders. Radioactive substances are injected into the blood, and special cameras monitor their uptake by the myocardium. Thus, where blood flow is obstructed, less radioactive material passes through. In the resulting image, such zones appear as dark spots.
- Computed tomography with contrast is performed in difficult diagnostic cases when other methods cannot determine the cause of anginal pain. Before the examination, the patient is injected with a contrast agent intravenously, and then the CT scanner takes a series of images, from which the computer creates a three-dimensional image of the heart. CT scans allow doctors to evaluate the condition of the arteries and detect narrowing or blockages in them.
- Bicycle ergometry is a stress test that is performed after acute signs of cardiac pathology have been removed. This technique allows you to determine the reaction of the heart and blood vessels to physical stress.
- Pulse oximetry - determining the level of oxygen in the blood.
ACS on ECG
All diagnostic measures are carried out under the constant supervision of a cardiologist. If the patient’s condition is serious, he is not examined comprehensively, but is limited only to visual examination data, pulse and pressure indicators, and ECG results. After stabilizing the patient’s well-being, they proceed to diagnostic measures.
Treatment in hospital
- Thrombolytic therapy – drugs are used to both dissolve blood clots and prevent the formation of new blood clots.
Endovascular (intravascular) and surgical methods to restore blood flow in the coronary arteries:
- Angioplasty and stenting. A catheter is inserted through the femoral artery into the coronary artery, and a balloon is inflated at its end, expanding the lumen of the artery. Then a prosthesis resembling a metal spring is installed - a stent, which strengthens the wall of the coronary vessel.
- Coronary bypass surgery. Using a heart-lung machine (with cardiac arrest), or under conditions of a beating heart, bypass paths (shunts) are formed around the affected area of the coronary arteries. It is through them that normal blood flow in the heart muscle is recreated.
- Direct coronary atherectomy. For this purpose, a cylindrical device with a side “window” located at the end of the catheter is used. It is fed under the plaque, it is cut off with a rotary knife and removed.
- Rotational ablation. The instrument is a special micro-drill (rotablator) designed to remove calcified plaques. Rotation speed 180,000 rpm, equipped with an elliptical tip. Injected into the artery, it grinds the plaque into microscopic fragments, clearing the way for blood flow. In the future, it is advisable to perform stenting. The method is not indicated for thrombosis.
Trigger factors
Factors that directly provoke an attack of acute coronary syndrome are:
- Intense stress, emotional shock. It causes a momentary narrowing of the arteries and manifests itself in different ways.
- Physical overload. For example, jogging, climbing to a floor without an elevator, carrying heavy objects without special equipment, and other options. Based on the nature of the provoking limit, we can talk about the severity of the process.
- Consumption of tobacco, coffee, alcohol, narcotic substances.
- Hypothermia.
The factors are easily identified. Many are subjective in nature and can therefore be eliminated by the patient himself. This is an important point, since activities are part of the prevention structure.
Chronic coronary insufficiency
The term “coronary insufficiency” means a state of reduced blood flow through the coronary vessels. Unlike the acute form, chronic coronary insufficiency develops gradually, as a consequence of atherosclerosis, hypertension or diseases leading to “thickening” of the blood (diabetes mellitus). All chronic forms of coronary circulatory failure are combined under the name “ischemic heart disease” or “coronary heart disease”.
The most common cause of coronary insufficiency is atherosclerosis, and the severity of the pathology often depends on the degree of vascular neglect
The main symptoms of chronic coronary insufficiency are similar in different forms and functional stages of the disease:
- Shortness of breath, dry cough are signs of stagnation in the pulmonary circulation, edema of the intercellular spaces of the lung tissue (interstitial edema) and pneumosclerosis (replacement of active tissue with connective tissue);
- Increased heart rate;
- Compressive, dull pain similar to angina pectoris that occurs after exercise (walking long distances or up stairs; after a heavy meal or nervous tension);
- Digestive system disorders: nausea, flatulence (bloating);
- Increased frequency of urination.
Diagnostics
An approximate diagnosis is made after listening to complaints and examining the patient. For final diagnosis, laboratory and instrumental studies are needed.
Standard methods:
- Complete blood count: detailed formula, ESR;
- Biochemical: lipoproteins, transferases, inflammatory markers;
- Blood clotting: degree of tendency to form blood clots;
- Coronary angiography: level of overlap of the lumen of the coronary arteries;
- Electrocardiography: the degree of myocardial ischemia, its conduction and contractility are determined;
- Chest X-ray, ultrasound: assessing the presence of other diseases, studying the cause of cardiac ischemia.
Treatment of chronic coronary insufficiency (principles)
- Stabilize the course of the underlying disease that caused myocardial ischemia (atherosclerosis, hypertension, diabetes mellitus);
- Reduce the impact of external risk factors (smoking, physical inactivity, obesity, stress, inflammatory processes);
- Prevention of angina attacks (vasodilators, sedatives, blood viscosity-reducing agents);
- If necessary, use surgical methods (angioplasty, bypass surgery).
The goal of complex treatment is to provide the heart muscle with a normal flow of oxygen. Surgical methods are indicated only in cases where they are considered the most effective for a given patient.
The chronic form of coronary insufficiency is never completely cured , so doctors give the following recommendations to people with this diagnosis:
- Maintain an optimal metabolic level for your age: normalization of body weight, balanced diet with limited fat, intake of vitamin-mineral complexes and Omega-3 (polyunsaturated fatty acids).
- Adequate daily physical activity: exercise, swimming, exercise on an exercise bike, walking (at least an hour a day) in the fresh air.
- Hardening: strengthening the immune system and preventing colds.
- Periodic visits to your doctor, tests and ECG - twice a year.
Non-standard advice
- It has been proven that pets prolong a person’s life. Simply petting a cat can normalize blood pressure, and walking a dog will put the nervous system in order. So consider getting a four-legged companion.
- Sleep: always with an influx of fresh air, always in a dark room - this is when the hormone melatonin is produced in the body. It slows down aging, optimizes the functioning of all organs, including the heart.
- Yoga classes, low-impact hikes, traveling in comfort - all this is quite accessible to patients diagnosed with chronic coronary insufficiency.
Treatment on the second and subsequent days
Treatment with the above drugs should be continued. If there is intracardiac thrombosis, the patient is prescribed warfarin. The goals of treatment are relief of pain, prevention of repeated attacks of angina, prevention of the development of acute myocardial infarction and associated complications.
In some cases (for example, if beta-blockers are contraindicated), calcium antagonists - verapamil, diltiazem, but not nifedipine - can be used. These calcium antagonists can be combined with nitrates. Angina pectoris not controlled with antianginal drugs is an indication for coronary angiography, followed by balloon angioplasty or CABG.
Before a person is discharged from the hospital, 24-hour ECG Holter monitoring and/or a test with mild physical activity (heart rate not exceeding 120 beats/min) are performed to identify latent ischemia. The presence of angina pectoris or silent myocardial ischemia in a patient is an indication for long-term treatment with antianginal drugs (calcium antagonists, beta-blockers, if necessary, in combination with nitrates), or surgical treatment.
Is it necessary to talk today about the relevance of such a problem as acute coronary syndrome (ACS)? Probably not. Like any extremely important topic, this cardiological pathology is constantly present on the pages of the medical press. The problem of ACS has long passed
Is it necessary to talk today about the relevance of such a problem as acute coronary syndrome (ACS)? Probably not. Like any extremely important topic, this cardiological pathology is constantly present on the pages of the medical press.
The problem of ACS has long crossed the boundaries of local clinics, intensive care units, specialized departments of medical institutions, becoming a medical and social problem, since it is associated with a high risk of developing myocardial infarction (MI) in patients, the possibility of a sharp deterioration of the condition, unpredictable consequences, the first place among which is sudden death.
So, our topic is acute coronary syndrome, our interlocutor is the head of the department of resuscitation and intensive care at the Institute of Cardiology. N. D. Strazhesko of the Academy of Medical Sciences of Ukraine, Doctor of Medical Sciences, Professor Alexander Nikolaevich Parkhomenko.
Alexander Nikolaevich, it has long been concluded that ACS is not only a medical problem, but also a social and public one. What is meant by the concept of “acute coronary syndrome” at the present stage?
— By ACS today we mean a chain of clinical manifestations united by one pathogenesis, which is based on atherosclerosis. There is atherosclerosis, which means that there are atherosclerotic plaques in the vessels; if plaques are present, then there is a possibility of developing their instability, etc. Ulceration or erosion of an atherosclerotic plaque leads to serious clinical consequences, in particular, the formation of unstable angina, small focal MI (or without a Q wave), large focal or transmural (with a Q wave).
According to statistics, about 50 thousand cases of MI are registered annually in Ukraine, but there is practically no information about the development of destabilization caused by unstable angina. Why? Because it is still difficult for our doctors to diagnose true instability of coronary blood flow and the development of minor myocardial damage. As a result, we are faced with the following situation. Patients who have suffered a large focal MI and have developed heart failure (HF) receive adequate (depending on the capabilities of the clinic and the patient) treatment. It is motivated because, having experienced a heart attack, patients are afraid of its reoccurrence. Patients diagnosed with unstable angina, who have a more or less favorable course of the disease, where there is a fairly low hospital mortality rate, are discharged home by doctors after observation in the hospital with a light heart, and local doctors, in the absence of symptoms of the disease, also easily cancel previously prescribed medications. When comparing statistical data regarding five-year survival, a paradoxical result was obtained: patients who suffered a large-focal MI often die less frequently than patients with a small MI.
Now let's approach the problem from the other side and see how many patients who suddenly feel ill are admitted to hospitals with a diagnosis of myocardial infarction? It turns out, not so much. If we were able to carry out competent statistical processing of data on the fatal outcomes of such patients, and make a comparative analysis of them, we would be able to show that the majority of deaths occur due to untimely provision of medical care or the patient’s visit to a doctor. The last fact is quite understandable: a person who has not previously had heart problems is unlikely to consult a cardiologist on time, due to various circumstances. The patient's visit to the doctor takes from several hours to several days. For comparison, in the United States of America emergency care is provided on average 2.5 hours after the onset of MI, in Holland - after an hour, in Ukraine - much later. Hence the late hospitalization of patients with MI and unfavorable outcomes, which once again indicates the relevance of the problem that we are considering today.
In addition, this also indicates the need for timely diagnosis. Which modern methods should a doctor rely on when diagnosing myocardial infarction without a Q wave?
— In principle, you need to understand the following: the term “acute coronary syndrome” itself is not a final diagnosis. This is a phenomenon that develops as a result of a certain sequence of a number of processes. Clinically, the onset of the process can occur in different ways. The patient feels pain (most often behind the sternum), the pain syndrome progresses sharply, is difficult to relieve with nitroglycerin, and even if it does, the treatment has an unstable effect. There are changes in the electrocardiogram, but in patients who have previously had a MI, there may be no additional changes in the electrocardiogram. As a result, when diagnosing ACS, the doctor often relies on his own intuition and proceeds from objective, often subjective, motivations. In addition to the pain syndrome and the nature of its development, we must not forget about progressive angina, which is generally known as an unstable condition. Here, special emphasis should be placed on patients who have the greatest risk of developing immediate complications. It is important to carry out a differential diagnosis with other similar pain in the chest, which may occur with pulmonary embolism, spontaneous pneumothorax, dissecting aortic aneurysm, various diseases of the gastrointestinal tract, in particular with pancreatitis, ulcers, strangulated hiatal hernia.
Of course, additional diagnostic research methods, which can only be implemented in a specialized hospital, play an important role in recognizing ACS; the results of these studies are used to assess the patient’s risk of complications. Let me give you an example. When examining cardiogram data when diagnosing myocardial infarction, the doctor always pays attention to the presence of a negative T wave, indicating myocardial damage. The occurrence of ST segment depression, even short-term, is not treated so carefully. When analyzing data on survival and the risk of developing MI in patients with ST segment depression and a negative T wave, it was found that the incidence of complications is 40-50% higher in patients with ST segment depression. A negative T wave has the lowest prognostic significance in terms of the development of complications in such patients. Why did we previously believe that by identifying negative T we could judge the development of myocardial necrosis? Yes, because we did not have other markers for assessing damage to the heart muscle.
What do we have today? When there is a question about diagnosing ACS, specific enzymes should be used - these are creatine phosphokinase and its MB fraction. This is the law. Without biochemical diagnosis of myocardial damage, we have no right to make a final diagnosis. Myoglobin testing is also used for this purpose, but it has not found widespread use in Ukraine, since its sensitivity and specificity is comparable to creatine phosphokinase.
Due to the fact that with minor damage to the myocardium, the doctor can sometimes miss the rise in creatine phosphokinase, other biochemical methods have been developed - determination of troponins T and I. Troponins make it possible to diagnose damage to the heart muscle not only in the early stages, but also at a later date, when the patient is admitted to the hospital. hospital some time after the condition worsens. In addition, troponin is not just a marker of myocardial damage, but also a marker that the prognosis of this patient is worse and the risk of developing repeated vascular accidents is higher. Unfortunately, today the determination of troponins cannot be considered accessible. These markers are not a standard test, which is regulated by the regulations on clinical laboratory tests, therefore, hospitals cannot purchase reagents for their determination at government expense. So far, such a very early diagnostic method as the determination of free fatty acid binding protein, which allows a diagnosis to be made within the first 40 minutes of the development of necrosis, has not yet found widespread use.
An additional method for objectifying the diagnosis is ultrasound. Modern ultrasound equipment makes it possible to evaluate the contractility of individual zones of the myocardium, which, in the absence of changes in the electrocardiogram, with a blurred clinical picture, helps the doctor to detect areas of reduced myocardial contractility and assume that it is ischemia that is the cause of the patient’s pain. It is quite difficult to verify this fact, since one cannot exclude the possibility of a decrease in its contractility even before the patient’s condition worsened.
Among laboratory research methods that have great prognostic value, the study of C-reactive protein in the blood is of particular interest. For a long time we assessed it qualitatively, not quantitatively. Today there is an opportunity to quantify low protein content. An increase in protein concentration in patients with ACS indicates the risk of further destabilization of their condition, and in patients with chronic ischemic heart disease - the risk of developing ACS. In addition, the prognostic value of markers such as increased fibrinogen and renal dysfunction has recently been proven. Thus, the detection of microalbuminuria and a decrease in creatinine clearance clearly correlate with patient outcomes during long-term follow-up.
Summarizing what has been said, I want to emphasize that from the standpoint of diagnosis and treatment, the approach to patients must be comprehensive. Stabilizing a patient's condition is not that difficult. The administration of heparins, for example, leads to stabilization in 70-90% of patients, but this stabilization is short-term. If treatment is not continued, the prognosis of the disease will not improve. First of all, we must answer two questions: does the patient actually have ACS and does this patient have an increased risk of developing further complications. This is fundamentally important, because if the risk of developing MI is high, therapy should be more aggressive. Following European guidelines, such patients should immediately undergo interventional intervention with drug support. In patients with a lower risk, the first priority is drug therapy, the effectiveness of which determines the need for coronary angiography in order to study the structure of the coronary arteries, the degree of their narrowing, the condition of plaques and the advisability of angioplasty or stenting.
Alexander Nikolaevich, when managing a patient, what are taken as a basis, recommendations or standards?
— These concepts are often confused. Recommendations, as is known, are created based on the results of large multicenter randomized controlled trials; they provide advisory information for understanding how best to treat the patient. Recommendations do not have legal force; in fact, using them, a specialist, knowing the problem, can vary, starting from the main directions of diagnosis and treatment.
Standards do not always coincide with recommendations. Each hospital, based either on national recommendations or using treatment standards approved by the Ministry of Health, can develop its own standards in relation to certain categories of patients.
What is needed to implement the standard? We need equipment that will allow this to be done, markers that can be used to clarify the patient’s diagnosis and prognosis, and medications for the patient. For example, a patient with ST segment elevation or unstable angina was admitted to the hospital, the doctor is obliged to prescribe him aspirin, heparin, and a beta blocker. To comply with the standard, all conditions must be created, which is quite often problematic in our country. We will probably be able to talk about standards that are as close as possible to the recommendations only with the introduction of insurance medicine. Although an intermediate option between the standard and the recommendations, to ensure the possibility of implementing the recommendations, of course, must exist. And it, without a doubt, must meet the modern requirements of the recommendations of the European and Ukrainian Societies of Cardiology.
As for me personally, I prefer to follow recommendations when managing a patient that have an objective and, if you like, intellectual basis. The doctor is obliged to think and look for compromises, since recommendations are not always feasible. We must not forget that they are created on the basis of large studies in which tens of thousands of patients participate, the individual approach is leveled out, and it is sometimes difficult to transform the average result in relation to a specific patient.
Alexander Nikolaevich, let’s dwell on the main principles of managing a patient with ACS.
— The primary priority for patients with ACS, of course, should be antithrombotic therapy, namely the use of antiplatelet drugs as first-line drugs. The proven gold standard remains acetylsalicylic acid - aspirin, a drug that has no analogues in medicine in terms of cost and effectiveness. The CURE study showed that the combination of aspirin with an antiplatelet drug of a different mechanism of action - clopidogrel - improves the prognosis both in the first hours after its use and in a longer period reduces the risk of developing myocardial infarction, cerebral strokes, and refractory angina. It was the proven effectiveness of the use of clopidogrel (Plavix) in patients with non-ST segment elevation ACS that allowed it to be included in the recommendations as a basic treatment regimen. In addition, clopidogrel is recommended for patients with non-ST segment elevation ACS who have undergone interventional procedures (stenting, angioplasty).
Today, to prevent complications of atherosclerosis and reduce the risk of their development, such a direction as the creation of drugs based on several drugs, in particular, combining a statin with aspirin, is being actively developed.
Separately, I would like to say about a relatively new group of antiplatelet drugs for our country - glycoprotein receptor blockers. Their story is interesting. At one time, studies conducted using drugs in this group did not show effectiveness in patients who did not undergo interventional interventions (angioplasty or stenting), so their use in patients without intervention was discontinued. At the same time, the latest analysis of the all-American database on the treatment of ACS in real clinical practice showed the absolute reliability of their effectiveness in reducing the risk of death. With what it can be connected? The fact is that in large multicenter clinical trials, most patients are initially prescribed angiography, and if a high risk is identified, they are immediately given interventional procedures under the protection of glycoprotein receptor blockers. In patients for whom stenting is not indicated, the risk of complications is low, so such potent drugs do not lead to a pronounced clinical effect.
But if we take people who do not participate in studies, but are actually treated, then in all countries, even patients at increased risk are not immediately sent for coronary angiography, but their condition is first stabilized (even if there is an increased risk). Prescribing glycoprotein receptor blockers in such patients in real clinical practice can have a good effect. I think that in Ukraine, where the availability of interventional interventions is low, the paramount issue is the need for stabilization; these drugs will find their place, they are reserved, although they are still used extremely rarely in clinical practice. Once a patient with non-ST segment elevation ACS is stabilized, I am an absolute advocate that if there are markers of high risk of long-term complications, he should be referred for coronary angiography. By the way, the question of when to start interventional procedures if ACS is diagnosed is now being actively discussed: in the first 4, 12 hours after destabilization of the condition or 3-5 days after stabilization of the patient? There is no consensus yet. A lot of research is currently being carried out in this direction, as a result of which, I hope, an answer to this question will be obtained.
As for anticoagulant therapy, and this is the next stage after the antiplatelet line of defense, among the drugs in this group we use direct anticoagulants - heparins, which have a rapid effect on thrombus formation. Among anticoagulants, standard heparin has historically been widely used, but its use requires constant monitoring of blood coagulation, intravenous administration, and the use of specific laboratory methods, which, like troponins, are not available everywhere. The use of surrogate methods does not make it possible to obtain an adequate result. In addition, we should not forget that many patients with non-ST segment elevation ACS are in therapeutic and cardiology departments, where often not only is there no question of adequate control, but also of the use of this drug (it is simply not prescribed).
Low molecular weight heparins, of course, have a significant advantage from a practical point of view over conventional heparin. The results of experimental studies have shown that their use may be more effective than heparin. After the accumulation of clinical data, the appearance in medical practice of several drugs of this generation, after a scrupulous comparison of standard heparin (if administered correctly) and low molecular weight heparins, it turned out that these drugs are similar in effectiveness. If we talk about different studies that were conducted using low molecular weight heparins, it is very difficult to compare them with each other, since all studies are characterized by different designs, different methods and criteria for monitoring the blood coagulation system, and different degrees of severity of ACS in the patients included in them. Therefore, the following can be found in the recommendations: in clinical practice, it is possible to use regular heparin, provided that the doctor keeps it in the doses that are necessary. And this is quite difficult, it requires very careful control, well-trained laboratory and personnel. In such a situation, most professionals prefer to use low molecular weight heparins (deltaparin, nadroparin, enoxaparin, etc.), to control the use of which there is no need for strict laboratory monitoring. In addition, the risk of bleeding during the period of time when their use is recommended (5-7 days) is small. It should be remembered that full recommended therapeutic doses may still cause bleeding in patients with a low platelet count or the presence of acute ulcers in the gastrointestinal tract.
One of the new directions for improving the stabilization of patients with ACS, in addition to the mandatory use of beta-blockers and, if necessary, angiotensin-converting enzyme inhibitors, is the prescription of lipid-lowering therapy. The emergence of this direction is absolutely logical, since today new, non-hypolipidemic (pleotropic) aspects of the action of drugs that can lower cholesterol levels have been elucidated. First of all, we are talking about statins and fibrates, which have anti-inflammatory properties. Based on the fact that a patient with ACS in the future has a chance to again get into an acute situation with unpredictable consequences, it was concluded that statins are preferentially prescribed in the hospital compared to their prescription after the patient is discharged from the hospital. The patient's adherence to this treatment develops in the hospital, so he continues to follow the doctor's recommendations after discharge. Outside the hospital, the patient, after stabilizing his condition, usually cancels treatment himself. The question of how long to prescribe statins after a patient develops unstable angina or MI is currently being actively debated. Theoretically, and the results of a number of pilot clinical studies have shown the advantage of their early administration, but this issue is still being debated.
Everything you said was reflected in the Draft Recommendations of the Ukrainian Society of Cardiology, which will be approved in September this year at the next congress of cardiologists?
— Last year, our working group on emergency cardiology discussed the possibility of adapting international recommendations to our conditions. The project has been created, it will be approved in September this year at the Ukrainian Congress of Cardiologists, which will be held in Dnepropetrovsk. Of course, the Project differs somewhat from the European recommendations. We discussed a lot about whether to leave the directions that we cannot implement today, or to proceed only from practical tasks? And we decided to leave behind much of what is unattainable for us today. We need a bar to which we must strive, and this bar is laid down in the Project.
The Draft National Recommendations included interventional procedures, stress testing of patients, assessment of troponins and C-reactive protein, and introduced such an item as intermediate risk for patients who would prefer to use a combination of clopidogrel and aspirin, etc. Of course, we understand that the same biochemical markers will not be available in all clinics and medical institutions, and stress testing will not be mandatory for all patients with ACS. But, I repeat, this is our benchmark, the future of good work.
And the most important thing that should be present in such a future is modern units or intensive care units for cardiac patients. Recently, we, the leadership of the Working Group on Emergency Conditions of the European Society of Cardiology, of which I am a member, have developed recommendations for the creation of such structures and regulations governing their work, approved by the Board of the European Society of Cardiology. In addition, proposals have been made to introduce a new specialty - cardiologist-resuscitator for European countries, primarily for the countries of the European Union. Unfortunately, the proposals of our Institute (since 1993) and specialists working in this field in Ukraine, that we also need such structures and trained specialists that meet modern high requirements, who would work on the appropriate equipment in the relevant institutions where they would have the opportunity to fully perform the functions that our medicine and society assign to them, while they remain proposals for the Ministry of Health. I hope that these issues will someday be resolved.
Absolute contraindications to TLT
- Any history of intracranial bleeding.
- Ischemic stroke within the last three months.
- Structural lesions of cerebral vessels.
- Malignant neoplasm of the brain.
- Closed head injury or facial injury in the last three months.
- Dissecting aortic aneurysm.
- Gastrointestinal bleeding over the past month.
- Pathology of the blood coagulation system with a tendency to bleeding.
Relative contraindications to TLT
- Refractory arterial hypertension (systolic blood pressure more than 180 mm Hg).
- History of ischemic stroke (more than three months old).
- Traumatic or prolonged (more than 10 minutes) cardiopulmonary resuscitation.
- Major surgery (up to three weeks).
- Puncture of a vessel that cannot be pressed.
- Peptic ulcer in the acute stage.
- Anticoagulant therapy.
In the absence of conditions for TLT, as well as in patients with ACS without ST segment elevation on the ECG, the prescription of anticoagulants is indicated: heparin 5000 U intravenous bolus or low molecular weight heparin - enoxaparin 0.3 ml intravenous bolus, followed by continuation of treatment in a hospital setting.
Prognostic assessments
The prognosis depends on the nature of the condition, lifestyle, age, gender (men can expect a slightly worse outcome), the presence of addictions, heredity, the nature of the treatment, concomitant pathologies, and type of professional activity.
The more negative factors, the worse the prognosis. Only a doctor can give specifics after a comprehensive assessment of all aspects and dynamics of the pathological process.
Attention:
Extremely unfavorable signs are fainting, especially frequent, the presence of heart failure, organic heart defects.
Acute coronary syndrome is a generic name for angina and heart attack. It is diagnosed accordingly, the code is determined according to the ICD. Prospects for cure are present for infarcts of minor severity and the initial stages of angina pectoris.