From this article you will learn:
- what is ethmoiditis,
- ethmoiditis - symptoms and treatment (conservative and surgical).
Ethmoiditis is an inflammation of the ethmoid sinus (ethmoid sinus). Often, inflammation of the ethmoid sinus is called the general term “sinusitis,” which should be understood as inflammation of any of the four pairs of paranasal sinuses.
The paranasal sinuses (in addition to the ethmoid sinus) also include -
- maxillary sinuses - their inflammation is called “sinusitis”,
- frontal sinuses - their inflammation is called “frontitis”,
- sphenoid sinuses - their inflammation is called “sphenoiditis”.
The ethmoidal sinus is paired (Fig. 1). Each ethmoid sinus consists of many small cavities in the bone (microsinuses), filled with air and lined from the inside with mucous membrane. The sinus has an oblong shape and is elongated in the anteroposterior direction.
Etiology, causes of occurrence and mechanism of development of ethmoiditis
The etiology of inflammation of the mucous membrane of the cells of the labyrinth (ethmoid bone) is infectious. The cause of the development of the disease can be viruses (adenoviruses, influenza viruses, rhinoviruses, etc.), bacteria (staphylococci, pneumococci, streptococci, etc.) and some pathogenic fungi.
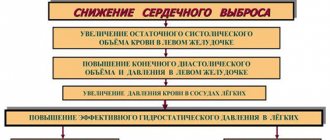
When infection penetrates the mucous membrane of the paranasal sinuses, irritation and inflammation occur. This provokes swelling of the tissues and an increase in their volume, which impairs not only nasal breathing, but also the outflow of mucus intended for sanitization of the nasopharynx. A large amount of secretions accumulates in the affected sinus or several of them, creating a favorable environment for the growth of pathogenic microorganisms. In the presence of such an environment, the pathogen or microbial association actively multiplies in the inflamed area, aggravating intoxication and provoking the release of pus.
Inflammation of the mucous membrane of the ethmoid bone in most cases is a secondary pathology - a complication of rhinitis, tonsillitis, sinusitis and other diseases of the upper respiratory tract. Infection by direct contact is unusual for ethmoiditis, which sharply distinguishes it from inflammation of other paranasal sinuses. Penetration of pathogens occurs primarily through the blood: this is due to the deep location of the labyrinth.
The following factors contribute to the development of infection in the cavities of the ethmoid bone:
- the presence of foci of chronic inflammation in the ENT organs;
- hyperplasia of the lymphoid tissue of the pharyngeal tonsil (adenoids);
- congenital anatomical features of the nasopharynx and facial bones (narrow nasal passage and cells of the ethmoid bone, etc.);
- facial injuries, curvature of the nasal septum due to a fracture;
- allergic rhinitis;
- immunodeficiency states.
Pathogens
The main causative agents of sinusitis are the same viruses that provoke the occurrence of acute respiratory viral infections, influenza, rhinovirus or adenovirus infections. The cause of the disease can be bacteria - staphylococci and streptococci, as well as pathogenic fungi. In medicine, there have been cases where sinusitis develops due to the so-called mixed infection. Several pathogens are detected in the material under study.
Ethmoidal sinusitis in rare cases develops primarily. As a rule, in preschool and school-age children and adults it appears as a complication from other infectious diseases: sinusitis, rhinitis, sinusitis. The infection enters the ethmoid sinus in two ways: hematogenous (most often) and contact. Sinusroethmoiditis can even affect newborn children. The cause is umbilical, intrauterine and skin sepsis.
Classification of ethmoiditis
One of the goals of diagnosis is to determine the type of ethmoiditis: symptoms and treatment directly depend on the form of the disease. This pathology is classified according to the following criteria:
- The nature of the current. According to this criterion, acute and chronic ethmoiditis are distinguished. The nature of the course most significantly influences the clinical picture of inflammation.
- Type of discharge (morphological features). Depending on the nature of the discharge, inflammation can be catarrhal, edematous-catarrhal, purulent and polyposis. Edematous-catarrhal and polypous forms of pathology have a chronic course. Morphological features are determined by the etiology of the process and its causative agent. The type of discharge is important for prescribing therapeutic measures.
- Prevalence of infection. Inflammation of the labyrinthine mucosa can be isolated or combined. A combined lesion can involve two sinuses (for example, sphenoethmoiditis) or more, up to all paranasal sinuses (pansinusitis).
- The side of the affected mucous membrane of the labyrinth cells. Depending on the side that the inflammatory process covers, right-sided, left-sided and bilateral pathology is distinguished.
The location of other infected sinuses in non-isolated ethmoiditis affects the localization of the focus of the inflammatory process. When the sphenoid sinus is affected, the area of the posterior cells becomes inflamed first, and when the frontal and maxillary sinuses are affected, the anterior cells become inflamed.
How does the disease develop?
From nearby organs, the inflammatory process moves to the cells of the ethmoid labyrinth. In case of inflammation of the maxillary and frontal sinuses, as a rule, the anterior cells are affected, and in the case of inflammation of the sphenoid sinus, the posterior cells are affected. Once on the mucous membrane of the cells, microorganisms multiply and damage its cells, and also penetrate deep into the tissues. Next, signs of inflammation appear (swelling, narrowing of the lumens of the cells and their excretory ducts).
Anatomy of the human hearing system
These changes lead to disruption of the outflow of fluid from the ethmoid labyrinth. In children, the pathological process can spread to the bone with subsequent destruction. The pathology results in purulent complications of ethmoiditis: abscesses, fistulas, empyema.
If left untreated, the pus can spread into the eye socket or cranial cavity, also causing life-threatening complications.
Clinical signs of ethmoiditis
Symptoms of ethmoiditis vary depending on the nature of its course, the type of infectious agent and morphological features. The main manifestations of pathology are the following:
- difficulty breathing through the nose, swelling of the nasal mucosa (rhinoethmoiditis);
- copious discharge of mucous or purulent exudate (most typical of combined lesions);
- decreased or complete absence of olfactory function;
- elevated temperature (usually up to subfebrile levels, but with severe intoxication and weakening of the body - up to a temperature of 38°C);
- increasing weakness, apathy;
- sleep disorders;
- loss of appetite;
- decreased performance and concentration;
- severe pressing pain in the projection area of the affected sinus;
- increased pain when bending forward and pressing on the projection area of the inflamed mucosa.
The labyrinth of the ethmoid bone is located in the area of the bridge of the nose. In the lateral projection, this sinus is located deeper than the eye sockets, so during inflammation, pain can radiate to the eyes, and in severe pathology, manifest as ophthalmological symptoms.
In vulnerable groups of patients (patients with immunodeficiencies and malnutrition, children, etc.), the signs of ethmoiditis may be more pronounced than in people with a normal immune response. This is due to the high probability of destruction of part of the ethmoid bone by pathogens and penetration of purulent masses into the orbital area. Acute intoxication and damage to the organ of vision is manifested by symptoms such as:
- fever;
- loss of visual acuity;
- swelling and redness of both eyelids;
- exophthalmos;
- restriction of eye movements due to their soreness.
The chronic inflammatory process in the ethmoid sinus occurs predominantly latently, with long periods of remission, interspersed with exacerbations. During an exacerbation, characteristic pressing pain near the bridge of the nose, mucous discharge (often with purulent impurities), deterioration of smell, swelling and soreness of the inner corner of the eyelids, displacement of the eyeball and signs of intoxication may appear.
During the period of remission, sluggish pathology is also manifested by symptoms of intoxication (weakness, lethargy, apathy), which significantly worsen the patient’s quality of life and performance. At the same time, mild but constant pain in the face, impaired sense of smell, and discharge of various types may be observed.
Physiotherapy
An effective method of treatment is physiotherapeutic procedures (in complex therapy). To relieve painful symptoms, doctors prescribe the following procedures to the patient:
- Electrophoresis in combination with antibacterial drugs. During treatment, the anterior paranasal sinus is affected. Medicines penetrate tissues that do not have a blood supply, resulting in faster healing results than with oral antibiotics.
- Phonophoresis. The treatment procedure affects the affected paranasal sinus with ultraviolet rays. To obtain a better anti-inflammatory effect, medications are first applied to the site of exposure.
- Helium-neon laser. Radiation slows down inflammatory processes, relieves hyperemia and swelling, improves blood supply in the affected area.
- UHF. Ultrafrequency therapy is used to warm up the ethmoid sinuses (used only during remission of chronic ethmoiditis).
Complications of ethmoiditis
If you do not consult a doctor in a timely manner, dangerous consequences of the pathology may develop. These include:
- deterioration of nasal breathing by more than 50%, complete loss of smell;
- inflammation of the ethmoid bone and destruction of part of the bone tissue;
- infection of the orbit (retrobulbar abscess, phlegmon, empyema);
- lesions of the arachnoid and pia mater (arachnoiditis, meningitis);
- brain abscess;
- other pathologies that arise against the background of a chronic focus of infection.
Diagnosis of ethmoiditis
If there are symptoms of ethmoiditis, the diagnosis should be carried out by an otolaryngologist. Diagnostic measures are carried out in the following order:
- Based on the patient’s complaints and medical history, a primary diagnosis is established. When interviewing the patient, the presence of chronic pathologies, immune status (in the presence of immunodeficiency) and characteristics of the condition are revealed.
- A visual examination of the patient is carried out. The purpose of the examination is to detect characteristic redness, swelling of the eyelids and exophthalmos, and to study increased pain during certain actions (palpation, bending).
- An endoscopic examination of the nasal cavities is performed. The study makes it possible to determine the condition (swelling, hyperemia) of the mucous membrane of the cavities and sinuses, the presence and nature of discharge, the condition of the lining of the labyrinth and the localization of the source of inflammation. In a chronic process, the prevalence of polypous formations is determined using endoscopy.
- An x-ray (image) of the paranasal sinus area is taken in the frontal projection. The presence of ethmoiditis on x-ray is indicated by darkening in the area of the labyrinth cells. In some cases (for example, to clarify the nature of formations or for the purpose of differential diagnosis), computed tomography is performed in addition to radiography.
To determine the type of pathogen and the state of the body, the patient may be prescribed laboratory tests (clinical tests of urine and blood, bacteriological culture of nasal discharge, etc.).
Prevention of ethmoiditis
Inflammation of the sinuses has an infectious etiology, so prevention of ethmoiditis is not specific and is aimed at the general strengthening of the body's defenses.
To prevent the occurrence of pathology, hardening methods, taking vitamin-mineral complexes and immunomodulators (on the recommendation of a doctor), and maintaining a sleep and rest schedule are suitable. In addition to hardening, it is necessary to dress in accordance with weather conditions, eat well, receive timely treatment for exacerbation of chronic pathologies and undergo a preventive examination by a therapist and otolaryngologist at least 1-2 times a year.
When traditional medicine is ineffective
Most often, doctors do not recommend treatment with folk remedies, since such therapy, as a rule, turns out to be ineffective and leads to loss of time. In this case, the acute phase very quickly transforms into chronic ethmoiditis, the symptoms of which are especially difficult for the patient to tolerate. That is why it is important not to waste precious time and promptly identify the symptoms of ethmoiditis and receive adequate treatment. It is not recommended to self-medicate during an exacerbation of a chronic form of pathology.
Prognosis of ethmoiditis
In rare cases, ethmoiditis resolves spontaneously in adults.
In most cases of acute pathology, after a course of antimicrobial therapy and the necessary procedures, complete recovery occurs.
Treating chronic sinus inflammation is a more difficult task. With an integrated approach to treatment (a combination of medication and surgery) and prevention of further exacerbations, it is possible to put the patient into a state of stable remission.
The most severe is inflammation complicated by infections of the eyes or brain. This pathology requires close attention from doctors, and often requires immediate hospitalization of the patient.
Antibiotics for ethmoiditis -
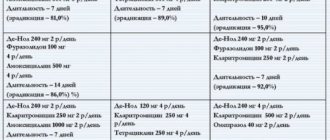
As we wrote above: acute frontal sinusitis most often develops against the background of acute respiratory viral infections and influenza, and antibiotics, as is known, do not act on viruses. Taking antibiotics for acute frontal sinusitis only makes sense if a bacterial infection occurs and purulent inflammation develops, but this does not happen immediately.
If there are indications for taking antibiotics, then the drug of first choice is Amoxicillin in combination with Clavulanic acid. Preparations that contain this combination: “Augumentin”, “Amoxiclav”. If the patient is allergic to antibiotics of the penicillin group, then it is better to use -
- antibiotics of the fluoroquinolone group (for example, Ciprofloxacin),
- or macrolides ("Clarithromycin", Azithromycin).
Antibiotics for frontal sinusitis are prescribed for approximately 10-14 days. However, after 5 days from the start of treatment, it is necessary to evaluate the effectiveness of therapy. If significant improvement is not achieved, then it is best to prescribe a more potent antibiotic.
Treatment
To completely eliminate ethmoiditis, treatment should consist of several stages:
- relieving intoxication and improving the general well-being of the patient;
- stimulation of the patient's immunity;
- relieving swelling of the mucous membranes, restoring normal fluid outflow and nasal breathing;
- rehabilitation of foci of inflammation and destruction of bacterial microflora in the sinuses.
For this purpose, medications, physiotherapeutic and surgical techniques, as well as folk remedies, are used.
Drug treatment
Medications for the treatment of sinus inflammation include the following drugs:
- antimicrobial drugs (Zinnat, Augmentin, Flemoklav, Sumamed, Amphotericin B, etc.);
- decongestants (antihistamines Cetrin, Loratadine, Zodak, etc.);
- vasoconstrictor and combined sprays for local action (Nazivin, Rinofluimucil, Xylometazoline);
- anti-inflammatory drugs (Paracetamol, Panadol, Nurofen, Nise, Ketorol);
- immunomodulators (Ribomunil, Immunal, etc.);
- vitamin and mineral preparations (Vitrum, Alphabet, Multitabs).
Antibiotics, vasoconstrictors and anti-inflammatory drugs are recommended to be used only as prescribed by a doctor.
Physiotherapy
In parallel with taking medications, the patient is advised to rinse the affected sinuses. The purulent contents are washed out using a special device - a YAMIK catheter. During the procedure, all paranasal sinuses are filled with physiological or antiseptic solution and the fluid is sucked out along with the pus that is removed. Rinsing continues until the cavities are completely clean.
If positive dynamics appear in the relief of inflammation, the doctor may prescribe physical therapy to the patient (electrophoresis with antibacterial agents, phonophoresis with glucocorticoids, UHF on the projection of the inflammatory zone, laser effect on the mucous membrane, etc.). These procedures stimulate tissue repair, reduce swelling and improve microcirculation in the affected sinuses.
Surgery
If other methods are ineffective, surgical treatment of ethmoiditis is performed - ethmoidotomy. The least traumatic operation is with endoscopic access to the bone through the nasal passage. In case of severe bone lesions and a high risk of disruption of nearby structures (eyes, central nervous system), surgical intervention with open access to the labyrinth is prescribed.
ethnoscience
In folk medicine, the following methods are used to eliminate sinus inflammation:
- instillation of vegetable juices (a mixture of freshly squeezed carrot and beet juices with honey in a 1:1:1 ratio), camphor oil and aloe juice;
- compresses with eucalyptus essential oil;
- warming up the sinus projection zone (in the absence of pus).
Traditional methods are not reliable and effective, and some of them can cause burns to the mucous membrane or the spread of infection. Before treating ethmoiditis with home remedies, you should consult your doctor.
Folk remedies
First of all, treatment with traditional recipes can only be started after consultation with an otolaryngologist. Many experts are against treating ethmoiditis at home, since the disease is dangerous due to its complications. If the doctor has approved the use of traditional methods, the treatment regimen is built on the principle of traditional treatment - the use of a vasoconstrictor, elimination of inflammation through rinsing, drops and inhalations.
Washing
- Soda, salt, tea tree oil. Dissolve 1 tsp in a glass of boiled water at room temperature. salt, a pinch of soda, a few drops of tea tree essential oil. The procedure is carried out three times a day using a syringe.
- Chamomile. Brew 1 tbsp in a glass of water for an hour. chamomile flowers. Strain the mixture and rinse your nose several times a day.
- Chlorophyllipt. A ready-made alcohol solution of chlorophyllipt can be purchased at a pharmacy. Dissolve a tablespoon of the product in two glasses of water. Wash your nose with the solution twice a day.
Inhalations
The procedure can be carried out in two ways: traditional (breathe healing vapors under a towel); using a nebulizer.
Traditional method of using steam inhalation
Recipes for decoctions for traditional inhalations.
- Pour 10 pieces of bay leaves with water, bring to a boil, reduce heat to low. Breathe in pairs for 5-10 minutes.
- Grind 3 cloves of garlic, add 100 ml of apple cider vinegar and a glass of boiling water. Carry out the procedure for a quarter of an hour three times a day;
- Pour 3 tbsp into two glasses of water. chamomile inflorescences, boil for 5-7 minutes, leave for 1.5-2 hours, bring to a boil again, add 5 drops of tea tree oil (can be replaced with eucalyptus oil). The duration of the procedure is 5-10 minutes, three times a day.
Steam inhalation using a nebulizer
Drops
- Drops from cyclamen juice. This remedy is the most effective in the list of folk recipes. To prepare, you will need to rinse the plant tuber, grate it, and squeeze out the liquid. The resulting juice is diluted with water - 1 part juice, 4 parts water. Place two drops of the prepared product into each nostril. The procedure is carried out before bedtime, since heavy discharge begins after instillation.
- Kalanchoe is another effective folk remedy against infections that get into the nose and prevent free breathing. You will need to cut three large leaves and put them in a cool place for three days. Then the plant needs to be crushed and the juice squeezed out. Strain the liquid and add water in equal proportions. The product is instilled 2-3 drops into each nostril several times a day.
- Black radish juice drops are a fairly effective folk remedy for ethmoiditis. To prepare, you will need to wash the radish, chop it, squeeze the juice out of the pulp, strain and bury it in your nose three times a day, 3-4 drops in each nostril.
After the procedure, the nose should be massaged especially actively in the area of the appendages. Then you need to lie on your back so that the drops spread evenly in the nasal cavity. After instillation, you need to blow your nose.
Ethmoidal sinusitis in children
Parents of infants and preschoolers need to remember what ethmoiditis is, because this pathology is characteristic of children and the only sinus lesion that can manifest itself up to 3-5 years.
In young patients, inflammation is more severe than in other patients: they have a high temperature (usually above 38-39°C), hyperemia or cyanosis of the swollen eyelids, protrusion and decreased eye mobility, severe anxiety, tearfulness, loss of appetite, nausea and vomiting (spitting up in babies).
If assistance is not provided, dehydration and intoxication of the central nervous system quickly sets in.
Unlike adults, who are characterized by combined lesions (sphenoidal and frontoethmoiditis), children under 5 years of age experience predominantly isolated inflammation of the mucous membrane of the labyrinthine cells due to the immaturity of the other sinuses.