Bronchial asthma (BA) refers to bronchopulmonary diseases. It is based on chronic inflammation of the airways, which leads to hypersensitivity, swelling, narrowing and obstruction of the airways.
The main signs of bronchial asthma are wheezing, chest tightness, coughing attacks, and a feeling of suffocation. The disease occurs in attacks, but with severe development, bronchial obstruction can be permanent, complicating a person’s daily life.
Asthma is a serious, chronic disease that requires constant monitoring and lifestyle adjustments. Timely assistance from a pulmonologist, correctly selected medications, therapeutic exercises and psychological support significantly improve the patient’s quality of life.
Classification of laryngotracheitis
Depending on what caused the disease, laryngotracheitis is usually classified into infectious, bacterial and mixed.
According to the nature of the course of the disease, acute and chronic forms of the pathology are distinguished. In turn, acute forms can be primary and recurrent in nature, as well as continuous or wave-like. With laryngotracheitis, laryngeal stenosis develops, that is, its pathological narrowing. This condition is dangerous because air does not enter the respiratory tract well and oxygen deficiency can develop. This condition is a threat to all human organs and systems and is fraught with serious consequences. Stenosis, when it is possible to compensate for breathing, occurs:
- Compensated;
- Incomplete compensation;
- Decompensated;
- Terminal (asphyxia or suffocation).
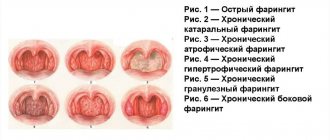
According to morphology, laryngotracheitis is usually divided into catarrhal, hypertrophic and atrophic.
This classification allows for differential diagnosis and provision of timely medical care to the patient. It is necessary to begin treatment as soon as possible if the patient is suspected of having laryngotracheitis; the symptoms of the disease are quite characteristic and have a decisive diagnostic value.
Morphological signs of various forms of laryngotracheitis
The most common form of the disease is acute laryngotracheitis. During the initial visual examination, you can see that the patient’s larynx is very hyperemic, has a bright red tint, and a large amount of purulent plaque (exudate) is visible in the lumen of the larynx. The mucous membrane is swollen and thickened. Based on the consistency of the exudate, one can determine how long ago the inflammatory process began in the patient. If at the early stage of the disease the exudate has a liquid consistency, then as the disease progresses, it becomes thicker and fibrous films are formed. By the color of the plaque itself on the mucous membrane of the larynx, you can even determine the etiology of the disease. So, with staphylococcal and streptococcal infections, the larynx becomes covered with very characteristic yellow-green crusts.
The catarrhal form of laryngotracheitis is characterized by characteristic changes in the mucous membrane. The mucosa is hyperemic and bluish in color, thickened and has small pinpoint hemorrhages in the submucosal layer.
In chronic hypertrophic laryngotracheitis, the patient experiences growth of the structural elements of the mucous membrane (hyperplasia), as well as hyperplasia of the submucosal layer and infiltration (impregnation) of the fibers of the muscles of the larynx and trachea, including the vocal cords, with exudate. Thickening of the vocal cords can be either diffuse or localized in the form of nodules. Such changes in the structures of the vocal cords are typical for people with increased load on the speech apparatus (singers, teachers, commanders, actors, lecturers and speakers). Hypertrophic laryngotracheitis can be complicated by the formation of cysts or characteristic ulcers of the larynx.
The atrophic form of pathology is characterized by various degenerative processes. The patient's vocal cords are very thin, the mucous membranes are dry, and upon visual examination, characteristic dry crusts can be found on the mucous membrane. Atrophy of the muscles and glands inside the larynx occurs and the nature of the epithelial tissue changes.
Causes of laryngotracheitis
There are many causes of laryngotracheitis, but it is very important to understand that the main cause is immunodeficiencies of various etiologies. A weakened body is very susceptible to various viruses and bacteria and is an excellent habitat for bacterial microflora. Even those microorganisms that are considered conditionally pathogenic (those with which a person gets along well) actively multiply in conditions of weakened immunity and often lead to the development of quite severe pathologies. Also predisposing factors can be considered:
- alcohol abuse, especially low quality alcohol;
- smoking;
- environmental factor;
- the patient has severe chronic diseases;
- constant hypothermia;
- congestive processes in the lungs of various etiologies (chronic bronchitis, bronchial asthma, COPD, etc.);
- various diseases of the nasopharynx that make breathing through the nose difficult or completely impossible (choanal atresia, sinusitis, sinusitis, allergic rhinitis, etc.).
In most cases, laryngotracheitis is a complication of one or another viral infection:
- adenoviral;
- ARVI;
- influenza virus;
- parainfluenza;
- rubella;
- measles;
- mumps;
- chicken pox;
- scarlet fever, etc.
Less commonly, laryngotracheitis can have a bacterial etiology and result from infection:
- staphylococcus;
- streptococcus;
- tuberculosis;
- pneumococcus;
- treponema pallidum;
- mycoplasma;
- chlamydia, etc.
Infection occurs through airborne droplets, especially when a sick person intensively sneezes or coughs in a confined space. That is why, more than others, laryngotracheitis affects children who spend a lot of time in a group of peers, where any infection spreads very quickly.
Prevention
There is no specific prevention of acute stenosing laryngotracheitis. But since OSLT is often included in the symptom complex of influenza and ARVI, preventive measures include measures to prevent infection with them. False croup can be prevented to a certain extent by creating certain living conditions for the child: moist and moderately cool air in the home, for which it is better to use humidifiers. It is equally important to harden the child, dress according to the season, which allows him to avoid overheating/hypothermia and do not forget about regular walks in the fresh air.
Symptoms of acute laryngotracheitis
The first symptoms of the disease occur, in most cases, against the background of a progressive infection of the upper respiratory tract of various etiologies. The main symptoms of an infectious disease (hyperthermic syndrome, fever, rhinitis, etc.) include a dry “barking cough”, sore throat, difficult or painful swallowing. In some cases, the disease occurs when the main symptoms of a viral disease have already passed.
Cough and its character is an important diagnostic sign. A dry and barking cough with laryngotracheitis has some features. First of all, this cough is characterized by pain in the chest, both during and after coughing. The patient's cough occurs more often at night or immediately after waking up. The rest of the time, anything can trigger a coughing attack: taking a deep breath, inhaling dust or too cold air, laughing, crying, etc. In acute laryngotracheitis, sputum is released when coughing, but it is not much and it has a viscous consistency.
As the disease progresses, the sputum becomes more abundant and thin and has a mucopurulent character. The patient experiences severe discomfort in the larynx: a feeling of the presence of a foreign body, difficulty swallowing, sore throat, dryness, burning, etc. The patient's voice changes its timbre and becomes hoarse and hoarse.
The lymph nodes of the patient's cervical group are enlarged upon palpation; upon auscultation, the patient's breathing is noisy, and sometimes dry wheezing can be heard.
Surgery
Tracheostomy is one of the ways to treat severe forms of laryngotracheitis. It is performed when the patient loses the ability to breathe fully. During the operation, the doctor makes incisions in the muscles and pushes the cartilage apart. A tracheostomy tube is then placed into the trachea.
Its special structure, similar to the anatomy of the larynx, allows one to avoid a wide range of complications and irritations that appear when a foreign body is introduced into the body. Until the patient’s natural breathing function is restored, the tube remains in the throat.
In case of severe stenosis with complete closure of the larynx, conicotomy is necessary - an emergency operation to restore breathing.
To do this, an incision is made in the skin and tissue between the cricoid cartilage and the Adam's apple. In an emergency, this can be done with a knife or piercing the throat with a thick needle. The skin must first be treated with an antiseptic.
At home, this is any alcohol-containing liquid, iodine or hydrogen peroxide. Then you need to insert an air tube into the larynx: the base of a pen or a thin syringe. If the procedure is carried out
Symptoms of chronic laryngotracheitis
Particular attention should be paid to cough. If in the acute form of laryngotracheitis it is episodic and paroxysmal, then in the chronic form of this pathology the cough is permanent. Moreover, the patient constantly experiences a feeling of discomfort in the pharynx and trachea, as well as frequent painful sensations behind the sternum. A constant persistent feeling that the throat is scratched, dry mouth, painful swallowing - this is an incomplete list of manifestations of chronic laryngotracheitis.
The most characteristic diagnostic sign is dysphonia or disturbances in the patient's voice function. Dysphonia can vary in intensity from mild “hoarseness” to complete inability to speak. Attempts to make sounds cause discomfort to the patient. This condition can be aggravated by certain climatic factors or various hormonal changes. Particularly severe forms of dysphonia occur in women during menopause, during pregnancy or during menstruation. This condition can be either periodic or permanent. Persistent dysphonia indicates various morphological changes in the structures of the vocal cords. If the patient’s professional activity involves the need to constantly communicate and be in public, the slightest changes in voice timbre can become a psychologically traumatic factor for them. As a result of this, the patient’s psychosomatic state is disrupted: sleep dysfunction, constant nervous tension, depression or neurasthenia.
Development mechanism
The trachea acts as an air-conducting tube, and during inflammation, swelling may occur in the area of its mucous membrane. This leads to the formation of content that is difficult to separate, irritating the receptors and disrupting the conduction of air masses.
The larynx, in addition to its air-conducting function, also plays the role of a voice-forming element. Due to the vocal cords. Air flows and vibrations of the ligaments create a certain sound heard by the ear.
With inflammation, the vocal cords become damaged and swell, and the area of the peri-ligamentous tissue begins to accumulate fluid and compress the area of the larynx.
A complication may occur - false croup (swelling with compression of the respiratory tract and suffocation).
Diagnosis of laryngotracheitis
The result of treatment depends on correct and timely diagnosis. Therefore, if you notice the first signs of the disease, you should immediately consult a doctor. Particular attention should be paid to laryngotracheitis in children, as the disease quickly progresses and takes on threatening forms. Often parents underestimate the seriousness of the situation, and therefore children end up in pediatricians in a deplorable state.
The most important diagnostic treatment is the initial interview with the patient and collection of anamnesis. If you have had an acute respiratory viral infection, recently had the flu or other upper respiratory tract diseases, do not forget to tell your doctor about this. After the survey is completed, the doctor conducts a visual examination. For this purpose, microlaryngoscopy is performed (a diagnostic procedure that allows you to determine the condition of the patient’s ligamentous apparatus and larynx). If the doctor sees such a need, a superficial biopsy (scraping out tissue samples for subsequent examination) can be performed during microlaryngoscopy.
In order for the treatment of the disease to be as effective as possible, it is necessary to identify the infectious pathogen. To do this, swabs from the patient’s throat and nose, as well as sputum, are sent to the clinical diagnostic laboratory for bacteriological culture. As additional research methods, sputum analysis for oxygen-resistant bacteria and its microscopy are used. Laboratory research methods such as enzyme-linked immunosorbent assay (ELISA), polymerase chain reaction (PCR) and immunofluorescence reaction (RIF) are also used. These advanced technologies make it possible to identify almost all pathogens of infectious diseases known to medicine.
It is also necessary to conduct radiography and computed tomography for the purpose of differential diagnosis from diphtheria, malignant and benign neoplasms of the larynx, pneumonia, bronchial asthma and retropharyngeal abscess.
How to treat with folk remedies
- Ginger, honey and lemon. A tasty and healthy medicine that can be taken during the cold season for prevention. You need to grate the ginger, chop the lemon along with the peel, and then add natural honey. Take 1-2 spoons per day, you can add it to warm tea.
- You can use onions in the form of a decoction. For adults, you need to cut one onion and grind it with two small spoons of sugar, then add water (250 ml). Boil until a thick mass is obtained, and take a teaspoon every hour during the day.
- To gargle, use a tablespoon mixture of eucalyptus leaves and chamomile flowers, add boiling water and leave in a thermos for two hours.
- Potato juice has a good effect: grate the potatoes and squeeze out the juice (you can use a juicer), add it to warm water for rinsing.
- Combine licorice root and fennel fruits, crushed leaves of coltsfoot and marshmallow in equal proportions. Pour 300 ml of boiling water over a teaspoon of the mixture and let it cool. After infusion, the resulting decoction should be drunk 4 times a day, 70 ml.
Complications of laryngotracheitis
The main complications of laryngotracheitis concern the bronchopulmonary system. An infection of the upper respiratory tract tends to descend into the bronchi and lungs, which causes tracheobronchitis, obstructive bronchitis or pneumonia. Inflammatory processes in the bronchi and lungs are accompanied by changes in the patient’s somatic condition: general weakness and symptoms of intoxication of the body, dizziness, increased body temperature (low-grade fever or hyperthermic syndrome), pain and discomfort in the throat, etc.
The most dangerous conditions occur in the youngest patients. Due to the anatomical structure of the larynx, complications in children can be very serious. Anatomically, the already narrow lumen of the larynx in a child with laryngotracheitis is filled with accumulated sputum and spasms of the laryngeal muscles often occur. This condition can cause a baby to have an attack of false croup - an acute inflammatory process of the larynx. False croup is classified as a condition that threatens the patient's life. If medical care is not provided, various respiratory dysfunctions are possible, including hypoxia and asphyxia. Cases of death have been recorded in pediatric practice.
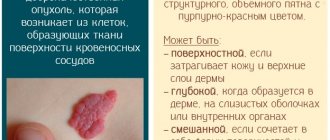
In chronic laryngotracheitis, in the absence of adequate therapy, constant irritation of the laryngeal mucosa occurs. Such “traumas” do not go away without a trace. Against the background of chronic laryngotracheitis (especially in the hypertrophic form), various neoplasms often arise. Initially, they are benign in nature, but tend to degenerate over time into a malignant tumor (larynx cancer).
Types of bronchial asthma
Let's consider one of the most general classifications:
- Allergic (atopic).
- Non-allergic.
- BA with late onset
- With fixed airway obstruction.
- BA in obese patients.
Atopic asthma has a pronounced dependence of clinical manifestations on exposure to allergens. It is often combined with other types of allergic reactions - allergic rhinitis, conjunctivitis, atopic dermatitis.
Atopic types are distinguished by the types of allergens that cause attacks - dust, fungal, pollen, epidermal (reaction to wool). Allergic asthma is one of the most common and is often inherited. It is usually well controlled, characterized by complete reversibility of obstructive processes and does not lead to mortality.
Other forms of the disease are much less well controlled, and the prognosis for them is more unfavorable for patients.
Asthma of a non-allergic nature is often provoked by respiratory tract infections - sinusitis, chronic bronchitis, pharyngitis. It can also occur as a reaction to stress, the use of certain drugs (for example, aspirin), as a result of damage to brain structures, hormonal imbalance and other reasons. This form of the disease is not hereditary.
Late-onset asthma is considered a disease that occurs after 40 years of age.