Tubulointerstitial nephritis is a primary lesion of the tubules and interstitial tissue of the kidneys, which results in a deterioration in their functionality.
Provocateurs of the acute variant of the pathology are often allergic reactions to medications, as well as infections. The development of chronic pathology is possible due to a combination of a number of reasons, including hereditary disorders, metabolic diseases, obstructive uropathy, chronic intoxication caused by prolonged contact with toxic substances in the environment, with drugs and herbs.
The disease is diagnosed based on a combination of anamnestic data and laboratory test results. Correction tactics are determined by etiological factors and the possibility of reversibility of the pathological process at the time of its detection.
Basic concept
Tubulointerstitial nephritis is a nonspecific disease that affects the liver. A rapidly occurring inflammatory process negatively affects the hepatic soft tissues and its canal passages. If treatment is not started in a timely manner, atrophy is possible. The etiology of this disease varies. Nephritis can be a consequence of an immune or metabolic malfunction. As kidney disease develops, it becomes worse, the blood flow becomes less clear, the normal functioning of the body is disrupted, and serious, irreversible consequences are possible.
Main classification
There are several classifications of tubulointerstitial nephritis. Main:
- The cause of the disease.
- Flow.
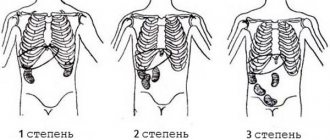
- Degree of tubular disorder.
If the main cause is tubular damage, then it is divided into:
- Tubular dysfunction.
- Partial violations.
- Malfunction of the endocrine system.
Occurrence and production locations: all over the world
There are jade deposits in different parts of the world, and most of them are still far from depleted. One of the most ancient suppliers of this stone is Burma. It is also mined in China, India, New Zealand, Mexico, Brazil, Canada, and the USA. Deposits are also known in European countries: Poland, Germany, Switzerland, Italy.
In Russia, greenish-gray jade was found in the Southern Urals at the beginning of the 20th century. Today, deposits of this mineral are known in Transbaikalia, in the Polar Urals. White jade was discovered in Buryatia; stones of this color are quite rare and highly valued
Causes of disease
Sometimes taking antibiotics or other anti-inflammatory drugs lasts for a long time. And kidney damage occurs after severe poisoning with chemicals and heavy metals. Ethanol vapors are especially harmful. Tubulointerstitial nephritis can occur due to many reasons:
- after a viral infection – in 46% of cases;
- toxic manifestations of an allergic nature provoke the disease in 28.3%;
- metabolic disorders in the body contribute to the occurrence of the disease in 13.9%;
- disorders of the circulatory function of the ureters – 8.8%;
- genetic and immune causes - in 0.9% of diseases;
- several causes are immediately observed in 2.5% of cases.
Chronic forms of the disease are caused by serious violations of the integrity of cytomembranes, dysplasia of kidney tissue, metabolic changes, congenital and acquired anomalies of the ureters.
Forms of the disease
Renal nephritis, tubulointerstitial, is divided into acute and chronic.
Acute tubulointerstitial nephritis manifests itself sharply, most often it is provoked by an allergic reaction to medications or infections. Quite quickly, kidney failure occurs and develops against the background of inflammation of the tubules.
Chronic tubulointerstitial nephritis can be caused by long-term use of medications or an overdose of infusions of medicinal herbs.
Predictions of therapy and undesirable consequences for the human body
Chronic tubulointerstitial nephritis requires long-term treatment. The average time to get rid of symptoms and partially restore the body is from 2 to 7 months. The likelihood of developing complications and undesirable consequences is influenced by other pathologies the patient has (especially damage to the heart, blood vessels, endocrine glands), his lifestyle, and the presence of bad habits.
In older people, due to the body's insufficient ability to regenerate, recovery is much slower. In particularly severe cases, it may take several years.
During the recovery period, it is extremely important for the patient to adhere to medical recommendations in order to avoid the development of unwanted complications. A colleague of mine was involved in the treatment of a young man with chronic tubulointerstitial nephritis who was a professional wrestler. The period of exacerbation of the disease coincided with the period of main preparation for the competition, as a result of which the patient spent a lot of time in the hospital. Before discharge, the doctor warned the man that it was necessary to reduce the intensity of training or even switch to a calmer and less traumatic sport. The patient followed the prescribed recommendations for a week, after which he returned to his usual program. Intense physical activity together with traumatic injury to the lumbar region contributed to the deterioration of the patient's condition. The newly cured nephritis worsened again, and the patient ended up in intensive care, where doctors fought for his life for a long time.
Undesirable consequences of pathology:
- uremic intoxication - deposition of urea in various organs and tissues with a violation of their integrity;
- acute or chronic renal failure, as a result of which the patient has to attend hemodialysis (artificial blood purification);
- anemia - anemia;
- the formation of cysts - cavities inside which there is fluid;
- development of inflammatory diseases of the bladder (cystitis), urethra (urethritis) and kidneys (pyelonephritis);
- disruption of metabolic processes in the body;
- thrombosis and embolism;
- tendency to spontaneous bleeding;
- urinary incontinence.
Photo gallery: complications of the disease
Pyelonephritis is characterized by inflammation of the kidney tissue
Rupture of kidney cysts can lead to shock
Uremic intoxication affects almost all internal organs
Main causes
For the development of tubulointerstitial nephritis, a provoking factor must reach the organs, most often these are medications.
Failure of the liver occurs for 9 main reasons:
- Long-term use of medications: non-narcotic analgesics, antibiotics, drugs containing lithium, potent medicinal herbs.
- Exposure to toxins: heavy metals, pesticides, low-quality alcoholic beverages, biological poisons.
- Failure of metabolic processes: blockage of arteries, hyperuricemia, rejection of a foreign body by the body, hepatitis.
- Infectious diseases.
- Viruses.
- Damage to the body by bacterial infections.
- Anemia.
- Myeloma.
- Inflammation of the genitourinary system.
Important!!! If an individual has already had problems with the normal functioning of the kidneys or has diseases of a chronic or other nature, disruptions in the functioning of the heart that can provoke inflammation, then he is not recommended to take diuretics, take antibiotics, sulfonamides, immunosuppressants for a long time, identify elements to which the body reacts especially acutely.
If the body has been affected by renal, tubulointerstitial nephritis, it will be difficult to get rid of it. The disease passes from acute to chronic form quite quickly. These processes can be triggered by untimely seeking of medical help, incorrect treatment and incorrect diagnosis.
Complications and prognosis
With tubulointerstitial nephritis, renal dysfunction occurs quite slowly, so the development of end-stage renal failure is unlikely, or occurs in a very advanced form. If the disease is not treated in time, there is a possibility of developing pulmonary edema. The disease can become chronic. If the correct treatment is chosen, the kidneys are restored completely.
Tubulointerstitial nephritis is a secretive disease, and it can sometimes be difficult to detect. You need to listen to your body in time and visit a specialist in a timely manner.
Only after appropriate tests can an accurate diagnosis be made and treatment begin.
Symptoms of the disease
The incubation period for kidney disease is 30 days. After this, tubulointerstitial nephritis begins to actively manifest itself. The symptoms are quite vague, so only an experienced specialist can prescribe the correct diagnosis and proper treatment.
General symptoms:
- Constant desire to drink.
- Severe pain in the lumbar region.
- Constant desire to go to the toilet.
- Rashes on the body.
- The appearance of edema.
- Pain in the head area.
- Weakness.
- Lack of appetite.
Acute tubulointerstitial nephritis is characterized by:
- A sharp increase in pressure.
- The occurrence of polyuria.
- Increased body temperature.
- Pain during urination.
- Purulent masses in the urine.
Chronic tubulointerstitial nephritis is characterized by:
- Increased pressure.
- Inability to go to the toilet for a long period.
- Increased levels of protein in the urine.
- The appearance of blood in the urine.
- Formation of kidney stones.
Clinical manifestations
Symptoms of the disease are varied and nonspecific. Their character largely depends on the cause of the pathological process.
One of the first signs of drug-induced TIN may be a repeated wave of fever against the background of effective antibiotic use in combination with skin rashes and an increase in the level of eosinophils in the blood, and less commonly, arthralgia. This condition is often misinterpreted and leads to the prescription of even more medications, which makes the situation worse. As the pathological process progresses, the patients' condition worsens; upon examination, they are found to have:
- moderate urinary syndrome with hematuria and proteinuria (up to 2 g/l);
- non-oliguric acute renal failure without arterial hypertension (decrease in glomerular filtration rate, decrease in the relative density of urine, increase in the concentration of creatinine and urea in the blood);
- liver damage (hepatitis);
- hyperproteinemia;
- decrease in hemoglobin;
- accelerated ESR.
Such tubulointerstitial nephritis in most cases has a cyclical course and quickly reverses after discontinuation of the culprit drug.
Among viral infections, hemorrhagic fever with renal syndrome is of greatest importance. Cases of the disease have been registered in the Far East, the Urals, and Bashkiria. The source of infection is rodents - field mouse, gray and black rat. The disease is characterized by autumn-spring seasonality and the following symptoms:
- increased body temperature;
- malaise;
- areas of hemorrhage on the skin and mucous membranes;
- thrombocytopenia;
- urinary syndrome.
Later, such patients develop acute renal failure with pronounced electrolyte changes. In this case, other organs and systems may be involved in the pathological process.
Acute TIN of a bacterial nature occurs as acute pyelonephritis. It can be primary (due to hematogenous spread of infection) or secondary, which develops against the background of any abnormalities in the development of the kidneys or impaired urine outflow. Sometimes kidney damage complicates the course of bacterial infections without bacteremia, for example, scarlet fever or diphtheria.
Among parasitic infestations, leptospirosis is of particular importance in the development of TIN. At the same time, numerous leptospires and infiltration of the interstitium with immune cells are found in the kidneys. Clinically this manifests itself:
- fever with severe intoxication;
- jaundice;
- enlarged liver and spleen;
- changes in urine composition (hematuria, leukocyturia, proteinuria);
- oliguric acute renal failure.
Kidney damage of this type often occurs in systemic diseases.
- Tubulointerstitial nephritis with renal failure may be the first manifestation of the disease in sarcoidosis.
- In patients with systemic lupus erythematosus, a number of cases of acute renal failure due to changes in the interstitial tissue have been described.
TIN in combination with uveitis is identified as a separate syndrome. This pathology is more often detected in girls in adolescence, less often in adult women. The disease begins against a background of complete well-being and manifests itself:
- general weakness;
- fatigue;
- loss of body weight;
- fever;
- pain in joints, muscles, lower back;
- skin rashes;
- changes in urinary sediment;
- development of renal failure.
In some cases, the causes of TIN cannot be determined, so they are considered idiopathic.
How to treat interstitial nephritis?
Treatment of acute interstitial nephritis begins with hospitalization of the patient in a hospital, preferably a nephrological one. Since in most cases the disease proceeds favorably, without severe clinical manifestations, no special treatment is required.
Immediate discontinuation of medications that caused the disease in acute cases often leads to rapid disappearance of symptoms. In the first 2-3 weeks, strict bed rest and limiting sodium in the diet are recommended. The amount of protein in the diet depends on the level of azotemia. Correction of disturbances in electrolyte composition and acid-base properties is necessary.
In case of severe disease (high body temperature, severe oliguria), in order to quickly reduce the swelling of the interstitial tissue, intravenous administration of high doses of furosemide, oral prednisolone for 1.5-2 months, followed by a gradual reduction in the dose until complete withdrawal are indicated. The administration of anticoagulants and antiplatelet agents is also indicated.
Treatment of chronic interstitial nephritis consists primarily of discontinuing those medications that caused the development of the disease. This helps to slow down the progression and stabilize the pathological process in the kidneys, and in some cases, with early diagnosis, a ban on further use of drugs can lead to the reverse development of inflammatory changes in the interstitial tissue and restoration of the structure of the tubular epithelium.
Prescribe vitamins (ascorbic acid, B6, B5) to improve hemostasis in the presence of anemia, antihypertensive drugs if there is arterial hypertension, anabolic hormones (mainly in the stage of chronic renal failure).
Patients with severe chronic interstitial nephritis and a rapidly progressive course are prescribed glucocorticosteroids at a dose of 40-50 mg. In the absence of signs of chronic renal failure, there is no need for restrictions on the diet; it should be physiologically complete in terms of the content of proteins, carbohydrates and fats, rich in vitamins. There is no need to limit the amount of kitchen salt and liquid, since there is usually no edema, and daily diuresis is increased.
The addition of a secondary infection requires the inclusion of antibiotics and other antimicrobial agents in the complex of treatment measures.
Stimulants of nonspecific immunity (lysozyme, prodigiosan), drugs that support renal plasma exchange, and vitamin supplements are also prescribed.
Diagnostic methods
Making an accurate diagnosis is a rather complex and lengthy process that takes place in several stages.
When a patient comes in with complaints and suspicion of renal tubulointerstitial nephritis, they are required to submit urine for a general analysis. They look at the levels of protein, leukocytes, red blood cells, and urine density. An analysis is required to determine the reaction to alkali.
If abnormalities are detected, the patient's blood is sent for biochemical analysis. In acute tubulointerstitial nephritis, sodium levels will be reduced. Based on these data, it is already possible to 90% assume the presence of the disease, and an ultrasound examination of the kidneys is prescribed.
To accurately confirm the diagnosis of tubulointerstitial nephritis, the doctor may recommend additional procedures:
- Urine culture.
- Biopsy of kidney material.
During kidney ultrasound, special attention is paid to the degree of swelling of the organ. If the form of the disease is acute, then they are enlarged. In chronic tubulointerstitial nephritis, the kidneys may be in a standard state. An examination is carried out to identify tumors and cysts, and the general condition of the tubules is studied.
If the ultrasound examination does not provide accurate data, the patient is sent for a computed tomography scan and, based on these data, treatment for tubulointerstitial nephritis is started.
Treatment of interstitial nephritis at home
Treatment of interstitial nephritis is carried out exclusively in a hospital setting, where the patient is provided with bed rest, dietary nutrition, constant monitoring by specialized specialists and therapy appropriate to his condition.
Patients with acute interstitial nephritis, after the disappearance of acute manifestations of the disease, should be released from work for at least another 2-3 months, and sometimes for a longer period. Patients should avoid overwork and hypothermia. Prevention of acute interstitial nephritis should be aimed at excluding etiological factors of the disease.
Treatment methods
For any form and level of development of tubulointerstitial nephritis, during treatment it is necessary to restore normal kidney function as quickly as possible, stop the inflammatory process and prevent complications.
Traditional black and green tea can be replaced with herbal tea, which includes bearberry and lingonberry.
You can prepare a medicinal infusion from flax seeds. To prepare, you need to brew the seeds with boiling water and leave for 40-50 minutes. Take 0.5 cups every 2-3 hours. The course of treatment is 2 days.
Tubulointerstitial nephritis is a disease for which treatment without medication is preferable. But, all unconventional methods must be reported to your doctor.
During the period of exacerbation of the disease, it is necessary to prevent sudden changes in temperature, hypothermia, and stressful situations.
For viral tubulointerstitial nephritis, antiviral drugs are prescribed, and for bacterial tubulointerstitial nephritis, antibiotics are prescribed.
During treatment, the patient must undergo a blood clotting test; if it is impaired, a course of anticoagulants is prescribed. If you do not drink it in time, blood thickening is possible, which, in turn, can lead to blood clots and kidney failure.
The treatment process must be constantly monitored by medical personnel, so the patient must stay in a medical facility around the clock.
Treatment of interstitial nephritis during pregnancy
Interstitial nephritis during pregnancy is an unfavorable disease that negatively affects both the health of the mother and the chances of survival of the fetus. Therefore, doctors strongly recommend that women prevent the disease rather than subsequently treat it.
Prevention of acute interstitial nephritis primarily consists of careful and reasonable prescription of medications, especially in individuals with individual hypersensitivity to them. When prescribing medications, it is always necessary to take into account the likelihood of developing acute interstitial nephritis and first carefully collect an anamnesis on the patient’s individual sensitivity to a specific drug. Prevention of chronic interstitial nephritis of drug origin is to limit the use (especially long-term and in large doses) of phenacetin, analgesics and NSAIDs.
They should be prescribed only according to indications and treatment with them should be carried out under strict medical supervision, especially in cases of increased individual sensitivity.
Timely cessation of the use of analgesics helps, especially in the early stages of the development of chronic interstitial nephritis, stabilize the pathological process in the kidneys, slow down its progression with improvement of kidney function, and sometimes in patients with mild disease, can lead to recovery.
Tubulointerstitial nephritis in children
This disease can also affect children's bodies. The causes and symptoms are similar to those in adults. The forms of the disease are similar.
Additionally, doctors claim that this disease can be passed on to a child “by inheritance.”
Children under 10-12 years of age are very difficult to tolerate tubulointerstitial nephritis. Their body temperature rises greatly, rashes and itching, nausea, and vomiting appear on the skin. Weakness is constantly present.
Unlike an adult’s body, a child’s body cannot contain the disease for a long time and complications appear, for example, kidney failure. That is why, if your baby has any health problems, you should immediately contact a pediatrician. Self-treatment is strictly prohibited.
Tubulointerstitial nephritis is a latent disease, therefore, in order to identify it in the early stages, you need to be attentive to your health, if you suspect inflammation, do not self-medicate, and consult a specialist as soon as possible.
What drugs are used to treat interstitial nephritis?
- Prednisolone - 40-60 mg per day for 1.5-2 months. followed by a gradual reduction in dose until complete withdrawal;
- Heparin - 20,000-30,000 units per day intramuscularly or intravenously;
- Dipyridamole - 300-450 mg per day.
The duration of active therapy depends on the course of the disease and the effect of treatment.
Symptoms of the disease
In the first stages of the disease, symptoms do not appear. Some patients are unaware of the developing pathology. Later stages of the disease make themselves felt with expressive signs:
- rashes appear partially or on the entire surface of the body, which are itchy;
- the temperature rises within small limits, severe cases are marked by a febrile state;
- pain in the kidneys is felt constantly or in frequent attacks;
- fatigue increases, the patient feels drowsiness;
- pressure surges are observed for no apparent reason;
- polyuria occurs.
Tubulointerstitial nephritis is characterized by many diverse manifestations. Symptoms include fever and rashes, but these changes in the body alone are not enough to make a diagnosis. The rash appears a month after the action of the toxin or within 3-6 days. It depends on the state of the body and its reaction to the allergen. There is weight loss, pain in the abdomen and in the back above the buttocks.
A disease that has passed into a chronic stage is characterized by mild symptoms for a certain period, which intensify over time. Some people develop nocturia and polyuria. Increased blood pressure and swelling of the extremities are not observed until renal failure occurs. The symptoms described in the list are characteristic of the acute stage of the disease.
Mineral and zodiac signs: choose by color
Jade has a special place in astrology; it is not associated with any particular zodiac sign. It is a stone of religions and life changes. In principle, almost everyone can wear it. But it is most suitable for Virgo and Libra , and is also good for Aquarius , Capricorn , Pisces, Cancer . Moreover, a stone is selected for a specific zodiac sign depending on its shade.
For Virgo, the best option is red or red-brown jade. For representatives of this sign, this stone brings good luck, as well as harmony in the family. Libra ; it is a talisman and assistant to representatives of this sign in all matters, and also promotes longevity.
For water signs - Pisces and Cancer - jade of a bluish tint, as well as black, is recommended. A blue stone is good for Aquarius, and a green stone for Capricorn. Jade is least suitable for Taurus and Sagittarius.