Pneumofibrosis is actually the final stage (outcome) of a chronic disease of the lung tissue.
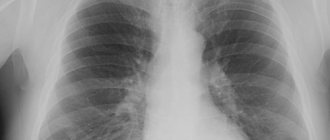
The outcome of long-term pathology leads to the fact that even the appearance of the lungs deteriorates significantly. They become like an organ eaten away by ulcers. In medicine, this type of lung is called a “honeycomb lung.” Features of chronic diseases of the lung tissue (these diseases are called interstitial) are associated with inflammatory processes in the interstitial tissue (the so-called connective tissue of the lungs). Part of this tissue is called interstitium. Small blood vessels pass through this tissue, through which the gas exchange function is carried out (carbon dioxide is exhaled, oxygen is taken for transfer to the body cells).
In a healthy state, interstitial tissue is very thin and practically invisible on x-ray examination. But in chronic diseases, due to inflammation, it begins to thicken, become covered with edema and scars (the same pleuropneumofibrosis develops). The simplest symptom of this transformation is shortness of breath.
General information
Pneumofibrosis of the lungs - what is it? This is the process of formation of connective tissue in the lungs, which replaces normal lung tissue. The formation of an excess amount of connective tissue is a consequence of sluggish, protracted inflammatory processes in the lung tissue and bronchi. We can say that pulmonary fibrosis is a secondary process and completes these diseases. It develops in areas of long-term unresolved pneumonia , in the tissue around the bronchi and blood vessels, around the lymphatic vessels, the walls of the alveoli and septa. The ICD-10 code is J84.1 (interstitial lung diseases with mention of fibrosis). Also, pneumofibrosis can occur for no apparent reason and progress rapidly - this is idiopathic fibrosing alveolitis (synonymous with Hamman-Rich syndrome ).
The stroma (framework) of the lungs is made up of connective tissue, which is located around the arteries, bronchi, and in the interalveolar septa. The structure of connective tissue contains collagen and elastin fibers. Elastin and collagen fibers intertwine in the walls of the alveoli and around the bronchi, and it is their interweaving that gives the lungs elastic properties - the ability to expand when inhaling and return to its original position when exhaling. The strength of the lung framework is associated with collagen.
With pulmonary fibrosis, an increased amount of connective tissue is formed due to collagen , and therefore the elasticity of the lung tissue is lost, the function of gas exchange is significantly reduced, since collagen is deposited in the walls of the alveoli, and respiratory failure progresses. The extent of fibrosis (local or diffuse) determines the degree of respiratory and gas exchange impairment, the course of the disease and its prognosis.
Medicines
Photo: ravenna24ore.it
The main drugs used in the treatment of pulmonary fibrosis are:
- glucocorticoids;
- cytostatics;
- antifibrotic agents.
The administration of systemic glucocorticoids (prednisolone, dexamethasone) alleviates the general condition of the body. It is also believed that drugs in this group can influence the replacement of normal lung tissue with connective tissue, inhibiting this process. However, there is also a negative side to taking glucocorticoids. In the treatment of fibrosis, glucocorticoids are prescribed for a long period of time; in some cases, the course of treatment can reach up to 3 months. Such prolonged use is dangerous for the development of side effects. These include:
- increased blood pressure, which is especially dangerous for people suffering from arterial hypertension. While taking glucocorticoids, resistance to early antihypertensive therapy may occur;
- exacerbation of peptic ulcer of the stomach or duodenum;
- osteoporosis, which leads to increased bone fragility;
- weight gain;
- hyperglycemia. Therefore, when taking glucocorticoids, it is important to monitor glycemic levels. Particular attention should be paid to people with diabetes.
The appearance of these symptoms is the reason for contacting your doctor, who, in turn, either adjusts the dosage of the drug or discontinues it.
The use of cytostatics (azathioprine, cyclophosphamide) is also accompanied by some side effects: the function of the gonads is disrupted, hematopoiesis is inhibited, undesirable effects from the gastrointestinal tract, nephro- and hepatotoxicity are observed. The most gentle drug in this group in this regard is azathioprine. This drug is able to block cell division and degeneration of tissue into fibrous tissue, which has a significant role in the treatment of pulmonary fibrosis. Taking the drug is strictly prohibited during pregnancy and lactation, and is also undesirable if you have existing renal or liver failure.
Colchicine also belongs to antifibrotic drugs, which can inhibit the production of fibronectin. With long-term use, a picture of myelosuppression can be detected, that is, a decrease in leukocytes in the blood, and thrombocytopenia (decrease in platelets), temporary alopecia, myopathy, peripheral neuritis, etc. is not a rare case. The drug is contraindicated in cases of severe impairment of liver and kidney function, cardiovascular pathology, purulent infections, pregnancy and lactation. In all other cases, the use of the drug is justified.
Pathogenesis
Lung connective tissue cells synthesize the proteins elastin and collagen . Elastin has the ability to stretch and return to its original position. Collagen forms strong fibrils and gives rigidity to the lung framework. The connective tissue produces both enzymes (proteinases) that destroy these proteins and proteinase inhibitors that inhibit the destruction process.
The proteinase-inhibitor system is normally in balance, but during inflammatory processes it is disrupted. During inflammation, the production of the enzyme a1-AT, which destroys elastase , decreases, as a result of which its activity increases. Elastase causes disorganization of connective tissue - it destroys elastic and collagen fibers of the alveolar walls. In place of the destroyed alveoli, cavities form. A combined bacterial-viral infection is itself accompanied by high production of elastase. Immune reactions that are triggered in the body during inflammation also activate the production of elastase.
On the other hand, during inflammatory processes, the activity of fibroblasts, which produce type 1 collagen, increases, which is accompanied by increased fibrosis and proliferation of connective tissue in the interstitium of the organ. When connective tissue spreads into the alveoli, intra-alveolar fibrosis occurs, then the connective tissue grows around the arteries and bronchi.
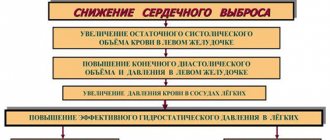
When vessels are involved in the pathological process, their sclerosis , the capillary bed becomes empty and hypoxia of the lung tissue develops. Under its conditions, the function of fibroblasts in relation to collagen production is further activated, which contributes to a more rapid development of pneumofibrosis . Therefore, hypoxia is the main condition for the replacement of normal lung tissue with connective tissue. Vascular involvement complicates blood circulation in the pulmonary circle. There is a load on the right side of the heart and hypertrophy of the right ventricle (pulmonary heart), which over time leads to cardiac decompensation.
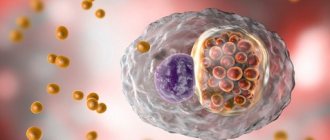
The pathogenesis of idiopathic fibrosing alveolitis is unclear. Presumably, collagen breakdown in interstitial tissue decreases, but its synthesis increases, in which fibroblasts and alveolar macrophages participate. In this case, it is important to reduce the production of an inhibitory factor, which inhibits collagen synthesis under normal conditions. Some authors consider Hamman-Rich syndrome to be an autoimmune disease, since there is overproduction of immunoglobulins of various classes. The resulting antigen-antibody complexes are deposited in the walls of the blood vessels of the lungs. Under the influence of the CEC, the lung tissue is damaged, it becomes denser, the interalveolar septa thicken, and the alveoli and capillaries are filled with fibrous tissue.
Treatment of pulmonary fibrosis
The danger of pulmonary fibrosis lies in the possible development of severe complications: cardiac, respiratory failure, lung cancer, thromboembolism. Scientific studies have proven that the risk of developing cancer in patients with pulmonary fibrosis is several times higher than in healthy people. Therefore, it is important to have timely, comprehensive corrective therapy that normalizes the patient’s condition and prevents the development of complications.
After diagnosing the disease, the specialist prescribes complex therapy, the task of which is to relieve the symptoms of the pathology and block the proliferation of connective tissue.
Drug therapy
The following drugs are used to treat pulmonary fibrosis:
- NSAIDs (nonsteroidal anti-inflammatory drugs) aimed at relieving inflammation and pain in the sternum. Diclofenac, Nimesil, Ibuprofen are prescribed;
- For severe inflammatory processes, glucocorticosteroids (steroid hormones) are used. They are often used to treat linear pulmonary fibrosis. Main drugs: Prednisolone, Hydrocortisone;
- Cytostatic agents that prevent connective tissue from growing further. Azathioprine, Cyclophosphamide are used;
- Antibiotics;
- Antifibrotic drugs: Veroshpiron, Colchicine;
- Antitussives and expectorants: Ambroxol, Eufillin, Salbutamol;
- Drugs that support heart function and prevent the development of heart failure: Methotrexate, Stofantin.
Surgery
In especially severe cases and the low effectiveness of drug therapy, surgical intervention is prescribed. The operation is necessary in the following cases:
- Hypoxia;
- Significant reduction in vital lung capacity;
- Decreased mechanical capacity of the respiratory system;
- Significant respiratory failure.
Extensive lesions require replacement of one or two organs. The operation lasts several hours. Before surgical procedures, the patient is prescribed special therapy. During the recovery period, the patient must take medications to prevent rejection of the replaced organ.
In the surgical treatment of local pulmonary fibrosis, when the lesions are not extensive, a lobectomy is performed. During the procedure, the affected area is excised.
Contraindications to the operation are:
- HIV;
- Hepatitis;
- Kidney failure;
- Serious diseases of the cardiovascular system.
Massotherapy
Massage manipulations can improve respiratory function and alleviate general symptoms. After the procedures, the intensity of the cough decreases, muscles are strengthened, and blood flow is restored.
Massage procedures are performed by a specialist either manually or using special equipment. To achieve the greatest effect, before starting the manipulations, the patient is recommended to take expectorant and antitussive medications.
The main types of massage include:
- Vacuum massage, during which vacuum cans are used. After the procedure, blood circulation in the lungs is normalized;
- Honey procedures. Massage manipulations are carried out using honey. This has a warming effect and activates blood circulation;
- Drainage, vibration procedures, thanks to which gas exchange is restored.
Oxygen therapy
The purpose of the procedure is to saturate the patient’s body with oxygen. The gas enters the human body through inhalation, through the respiratory tract. Pure oxygen and mixtures with it are used. Inhalation is carried out using special tubes, nasal catheters, masks for the nose and mouth.
Oxygen therapy allows you to achieve the following results:
- Normalization of the oxygen level in the blood leads to the restoration of gas exchange in the patient’s body;
- A sufficient concentration of gas leads to improved metabolic processes in the lungs;
- Symptoms are significantly relieved;
- Blood circulation is normalized;
- The patient's general condition is improving.
Breathing exercises
Therapeutic breathing exercises are one of the most effective methods of complementary therapy.
The purpose of breathing exercises is to reduce fatigue, weakness, and relieve tension in the patient. A special technique allows you to speed up blood circulation, improve respiratory function, and alleviate the patient’s condition. Congestion is relieved and sputum is cleared better. Gymnastics is one of the effective ways to treat focal pneumofibrosis, as it helps relieve inflammation that leads to the growth of scar tissue, improves metabolic processes and the protective functions of healthy tissues.
The complex consists of 3 stages:
- Inhalation is performed with maximum inflation of the abdomen. The diaphragm is motionless, which is controlled by the hand lying on the chest. Exhalation is done with retraction of the abdomen;
- Then diaphragmatic breathing is performed. Inhalation is carried out with the lungs, the stomach is motionless. You need to try to inhale and exhale as deeply and slowly as possible;
- The final stage involves united breathing. Inhalation is done while inflating the abdomen, then 3 breaths are taken with its maximum protrusion. Then exhale through the chest.
It is recommended to perform exercises up to 6 times a day, starting with 3 times. The most positive result is achieved if you supplement the respiratory complex with walking and cycling.
Diet therapy
In case of pulmonary fibrosis, special attention is paid to the diet. It is necessary to exclude spicy, excessively salty, fatty foods. Increase the amount of vegetables, cereals, and fruits high in vitamin C consumed. It is necessary to consume fish, milk and dairy products, meat, and seafood.
Treatment of pulmonary fibrosis with folk remedies
Among the effective methods of traditional medicine used as additional treatment are:
- Anise infusion, which restores lung tissue, improves general condition. 1 tbsp of seeds is poured into a glass of boiling water, the liquid is brought to a boil and immediately removed from the stove. The decoction should be cooled and taken morning and evening;
- Flax seeds, an infusion of which reduces shortness of breath and relieves cough. 1 tbsp. seeds are poured with a glass of boiling water and infused for 20 minutes. The infusion is taken three times a day.
Classification
With the flow:
- Progressive.
- Not progressive.
According to the prevalence of the process:
- Local.
- Diffuse.
Depending on the damage to individual lung structures (this is determined by computed tomography), the following types of pneumofibrosis are distinguished:
- Interstitial.
- Perivascular (spread of connective tissue around blood vessels).
- Alveolar (intra-alveolar - connective tissue replaces the alveoli).
- Peribronchial (distribution of connective tissue around the bronchi).
- Perilobular (growth along the interlobular septa).
Local pneumofibrosis is also limited. In the local variant, the pathological process of fibroformation covers one area (locus) of the lung tissue. This part of the lung becomes denser, which is very clearly visible on x-rays - the pathological process has clear boundaries.
Local fibrosis is the outcome of macrofocal pneumonia, but can also be detected in chronic bronchiolitis. Most often, local pulmonary fibrosis does not affect respiratory function and is asymptomatic.
Diffuse pulmonary fibrosis is characterized by the appearance of large areas of replacement with connective tissue, which diffusely covers almost all of the lung tissue. of emphysema may also form in the lungs . Since the spread of the process occurs faster than in the local version, the structure of the lungs is significantly deformed and the volume of the lungs decreases, pronounced disturbances in respiratory function are noted.
Complete ventilation of the lungs is significantly reduced and diffuse pulmonary fibrosis relatively quickly leads to the development of respiratory failure. The situation becomes more serious if both lungs are affected and the pleura is involved in the pathological process (pleuropneumofibrosis). This form of pulmonary fibrosis occurs in occupational diseases associated with inhalation of dust from silicon dioxide and metals (in particular, beryllium).
There have been cases of the development of diffuse pneumofibrosis in children with bronchopulmonary dysplasia, which develops in newborns during the treatment of respiratory disorders with artificial ventilation using high concentrations of oxygen. Diffuse pulmonary fibrosis is the outcome of exogenous allergic alveolitis that occurs when inhaling allergens. This may be material containing fungi (actinomycetes, penicillium, aspergillus), bird protein from parrots and pigeons, antigens of insects and fish (for those working with fishmeal).
Hilar pulmonary fibrosis is a lesion of the lungs in the area where the anatomical connection of the lung with the mediastinal organs is located. Radical fibrosis is a consequence of past pneumonia and bronchitis . It can form for a long time after illness. In sarcoidosis, in most cases fibrosis develops in the upper lobes, as well as hilar fibrosis.
Idiopathic fibrosing alveolitis (IFA) or Hammen-Rich disease is distinguished separately . It is a rapidly progressive form of diffuse pulmonary fibrosis, the cause of which is unknown. The disease is severe with constantly increasing respiratory failure. Idiopathic fibrosing alveolitis is the most unfavorable prognostic lung disease, manifesting itself at different ages, with men getting sick more often. Inflammatory damage to the lung tissue and alveoli develops, which leads to disorganization of the lung parenchyma, interstitial fibrosis and cystic formations in the lungs. ELISA can occur in healthy lung tissue, and against the background of chronic broncho-obstructive pathology.
Do the lungs recover completely?
There is an opinion that fibrous changes, once they appear, do not resolve. Which of those suffering from covid pneumonia may be affected?
- Pulmonary fibrosis due to coronavirus threatens patients with severe infection and those who were on mechanical ventilation. This does not mean that all of them will necessarily end up with irreversible fibrosis.
- In the majority of patients, pulmonary fibrosis does not develop after pneumonia. Their lungs return completely to normal.
Signs of fibrosis, which are detected on CT scans at the height of the disease or on control tomograms, also do not always mean that the changes are irreversible. It takes time for persistent areas of pulmonary fibrosis to form. On average it is two to three months .
Today, radiologically confirmed statistical data on the incidence of fibrosis after covid has not yet been accumulated. It takes about six months after the main wave of mass morbidity has subsided to obtain reliable facts on this issue.
Those radiological symptoms of fibrosis that are visible during the course of the disease are far from the final picture. The course of the viral-bacterial pulmonary process during covid is supplemented by:
- vasculitis,
- thrombosis,
- and is radiologically and clinically different from classic bacterial pneumonia.
If the focus of community-acquired pneumonia on the control x-ray gradually resolves, undergoing reverse dynamics after a course of antibiotics, then covid inflammation can take a long time to transform:
- foci of “ground glass” can resolve in some parts of the lung field and appear in others,
- merge, be supplemented by thickenings of the interalveolar septa, interlobular spaces, shadows of alveoli filled with effusion.
All this can simulate areas of pulmonary fibrosis. Such as, for example, after severe bacterial pneumonia. Hence, in the descriptions of tomograms, conclusions about linear pulmonary fibrosis or the words “focal fibrosis” may appear. It is worth understanding that this is a dynamic condition that may undergo changes during the course of recovery from the viral process.
Causes
First of all, various diseases of the bronchopulmonary system lead to pulmonary fibrosis:
- Pneumonia . Its protracted course is naturally resolved by the formation of post-pneumonic pneumofibrosis, which is observed in 10-20% of patients. With pneumonia caused by Legionella pneumophila, a long course is always observed, foci of infiltration that do not resolve for a long time and a high incidence of post-pneumonic pneumofibrosis. Staphylococcal pneumonia usually occurs with destructive changes in the lungs; there is a slow resolution of the disease, resulting in local pneumofibrosis.
- Occupational dust diseases that are associated with inhalation of dust and gases. They occur as diffuse pneumonitis and progressive alveolitis with a mandatory outcome in fibrosis. Occupational diseases include silicosis , silicosis and metalloconiosis . The fibrogenicity of coal dust varies. Dust with a silicon dioxide content of more than 10% is considered highly fibrogenic and upon contact with it, silicosis, silicosilicosis and anthracosilicosis occur. This group of diseases is characterized by a progressive fibrotic process. When exposed to weakly fibrogenic dust (silicon dioxide in it is less than 10%), silicates, carboconiosis, pneumoconiosis of grinders, metalloconiosis from radiopaque dust, and from dust from electric welding of iron products develop. These diseases are characterized by moderate pneumofibrosis, a benign course with slow progression. They are often complicated by chronic bronchitis, which determines the severity of the disease.
- Miners' pneumoconiosis combines interstitial fibrosis and local emphysematous areas. During the course of the disease, the prerequisites for productive sclerotic changes are formed, characterized by the development of pneumofibrosis in the acini and lobules of the lung. The reason for the rapid development of connective tissue is a violation of the lymphodynamics of the lungs, since dust particles are excreted lymphogenously through the lymphatic vessels of the acinus. Under conditions of prolonged exposure to dust, removal becomes difficult.
- Chronic obstructive pulmonary disease , which is characterized by inflammatory changes in the bronchial wall with the development of peribronchial fibrosis. In bronchial asthma, subepithelial fibrosis develops.
- Allergic lung diseases. A synonym is exogenous allergic alveolitis. The disease occurs when inhaling dust containing antigens. Damage to the alveoli and surrounding tissue is typical, resulting in fibrosis. An occupational disease develops in persons who have constant contact with dyes, resins, fungicides, polyurethane, chromium, cobalt and arsenic, engaged in rubber production, mushroom cultivation, and compost processing. In addition, one of the most common causes of allergic alveolitis is keeping a house with flying birds (pigeons, budgies) and living in damp rooms with mold. People prone to allergic diseases are at risk. Pneumonitis (alveolitis) has different course options: from recovery to severe development of fibrosis (“honeycomb” lung) with gross damage to the pulmonary architecture.
- Cystic fibrosis . Inflammation in the walls of the bronchi causes fibrotic changes in the wall itself and peribronchial fibrosis. These processes, in turn, contribute to the development of bronchiolitis obliterans with expansion of the alveoli and alveolar ducts.
- Pulmonary sarcoidosis . This is a systemic disease, which is characterized by the formation of granulomas in the lung tissue and intrathoracic lymph nodes. In the lungs, against the background of pneumofibrosis and emphysema, dissemination of foci is determined. As the disease progresses, conglomerates of lesions invade the entire lung tissue, and pulmonary fibrosis and emphysema also intensify. At this stage of the process, the patient develops severe respiratory failure.
- Conditions after lung surgery always end in the formation of pneumofibrosis.
- Tuberculosis . The long course of tuberculosis is accompanied by pneumofibrosis, emphysema and bronchiectasis.
- Mechanical damage to the lung.
Other causes of pulmonary fibrosis include:
- Chronic active hepatitis .
- Scleroderma , systemic lupus erythematosus , rheumatoid arthritis , ankylosing spondylitis .
- Diabetes.
- Radiation exposure. Pneumofibrosis is considered as a complication of radiation therapy for lymphogranulomatosis , breast cancer , and pleural mesotheleoma . Radiation therapy to lymphatic drainage areas is also often accompanied by the development of pneumofibrosis.
- Chronically ongoing infectious processes. The chronic course of cytomegalovirus infection is very characterized by the development of pneumofibrosis.
- Toxic effects of medications. Amiodarone is a drug with proven pulmonary toxicity. When taking amiodarone, as well as cytostatics and nitrofurans, fibrosing alveolitis (allergic alveolitis) may develop. Taking Prokolol is complicated by pulmonary fibrosis, which leads to respiratory failure. The formation of fibrotic masses in the alveoli is observed when taking sulfonamides, penicillins, gold salts and narcotic drugs. Ergotamine causes pleural fibrosis.
- Although the cause of idiopathic interstitial fibrosis is unknown, there are risk factors that contribute to the development of the disease: smoking, respiratory tract infections, exposure to external factors (metal, wood, stone, plant dust, contact with birds, work with herbicides and fungicides, contact with aerosols and dyes hairdressers) and genetic predisposition.
Prevention
The main method of preventing pulmonary fibrosis is timely diagnosis, proper treatment of the underlying disease and pulmonary fibrosis itself, as well as following all doctor’s recommendations.
Smokers, naturally, will have to give up their bad habit.
Attention. If a person’s work activity involves constant contact with hazardous and toxic substances, then the best option would be to abandon such a profession.
Symptoms
Symptoms depend on the underlying disease against which pulmonary fibrosis occurred, but the main complaints of patients with pulmonary fibrosis of any origin are shortness of breath on exertion and at rest, weakness, and increased fatigue. As shortness of breath progresses over time, it becomes the dominant symptom. Patients may also be bothered by a cough without sputum, chest pain, and sometimes hemoptysis due to associated vasculitis . The temperature rises with exacerbation of the underlying disease. Weight loss is not typical.
With silicosis, the symptoms are scant: cough, shortness of breath, sputum production. In chronic bronchitis and bronchiectasis - cough with sputum. Auscultation of patients reveals weakened breathing, dry wheezing, reminiscent of “crackling cellophane” in the lower parts of the lungs.
Over time, with the development of cor pulmonale, patients develop puffiness of the face and swelling of the veins of the neck. In severe cases of heart failure, swelling of the legs and accumulation of fluid in the cavities appear: hydrothorax (in the pleural cavity), hydropericardium (in the pericardial cavity) and ascites (in the abdominal cavity).
Hamman-Rich syndrome has an acute onset, with cough, fever (associated with bacterial pneumonia) and increasing shortness of breath. In this case, the cough is unproductive (little sputum is produced), the patient is bothered by tightness in the chest and pain in the chest. Respiratory failure , cyanosis increases very quickly pulmonary hypertension and chronic cor pulmonale develop . Steadily progressing shortness of breath limits the patient's movements, he cannot take a deep breath and loses the ability to care for himself. Weight loss progresses and joint pain appears.
In the second variant of the course of idiopathic fibrosing alveolitis, which is more common, there is a gradual onset and slowly progressive shortness of breath (first with exertion, and then at rest).
Patients are concerned about a nonproductive cough, weight loss, and fatigue. In the later stages, thickening of the nail phalanges of the hands—“drumsticks”—is observed. The age at which the disease occurs is 60-70 years.
Tests and diagnostics
- The screening method is fluorography.
- X-rays provide more accurate diagnostic signs. Hamman-Rich syndrome is characterized by the following radiological signs that initially appear in the lower and middle parts of the lungs: strengthening and deformation of the pulmonary pattern, decreased transparency of the lungs due to a large number of strands running along the bronchi and vessels from the root of the lung to the periphery, swelling of the lung tissue along the periphery. A cellular pattern is characteristic due to connective tissue growth around the acini. As the disease progresses, the pleura thickens (parietal, interlobar, diaphragmatic) and the upper sections are involved in the process. Fuzzy focal merging shadows appear in the lungs, and the mobility of the diaphragm decreases. In advanced cases, cavities up to 1-3 cm appear on the periphery of the lungs and the formation of a “honeycomb” lung.
- High resolution computed tomography. This is a highly sensitive method that determines the severity of fibrosis, its prevalence and changes in dynamics. The technique of thin sections and reconstruction of the lung in space makes it possible to see the process in volume. The picture of idiopathic fibrosis in the early stages is represented by changes in the form of “ground glass”. Then basal changes are formed on both sides according to the “honeycomb lung” type, which gives rise to cysts measuring 3-10 mm with thick walls.
- Tomography and bronchography detect bronchiectasis in the lower parts of the lungs.
- Body plethysmography (a study of the elasticity of lung tissue) reveals a “hard” lung.
- Study of the function of external respiration - changes of a restrictive type, a decrease in lung volumes (decrease in vital capacity).
- A study of blood gas composition shows a decrease in the diffusion capacity of the lungs.
- Hypoxemia (partial oxygen tension decreases to less than 60 mm Hg) increases with exercise, and at its height hypercapnia (the level of carbon dioxide increases, its pressure becomes more than 45 mm Hg)
- Cytological and histological examination of lung tissue biopsy.
Diagnostic measures
The most effective diagnostic procedures to identify diffuse pulmonary fibrosis are:
- X-ray examination. The method accurately determines the location, structural changes in the lung, and the degree of damage;
- Angiopulmonography evaluates changes in blood flow in the vascular system of the respiratory organs, blood flow disorders;
- Studies using a tomograph (CT, MRI);
- Spirographic examination. Using this method, a decrease in the functioning of the respiratory organs, the degree of decrease in volume and an increase in respiratory rate are accurately determined;
- Biopsy.
Consequences and complications
The consequences of pulmonary fibrosis are quite serious and the main ones are:
- Progressive respiratory failure.
- Lung cancer , which often develops against the background of idiopathic fibrosis.
- Secondary pulmonary hypertension , which develops already in the first years of the disease, but proceeds unnoticed by the patient. As it progresses, shortness of breath increases, which depends on the level of increase in pressure in the pulmonary artery.
- Pulmonary hemorrhage , pneumothorax and pneumomediastinum are the consequences of rupture of fibrous cavities and cysts that form in the lungs in the late stages of idiopathic fibrosis.
How to stop
Already formed fibrosis, unfortunately, is irreversible. Treating an old scar is a thankless task. Rehabilitation specialists and pulmonologists are trying to decide how to stop pulmonary fibrosis at the formation stage (see rehabilitation after coronavirus). They are the ones who have to deal with patients at high risk of fibrosis while still in the hospital:
- Drugs for fibrosis (glucocorticoids, cytostatics, longidase, bronchodilators, ursodeoxycholic acid drugs) - drug treatment.
- Physical therapy is a non-drug part of recovery. Gymnastics for fibrosis should continue at home.
Recovery after COVID-19. The most effective exercises from a rehabilitation doctor
Fibrosis drugs
Since pulmonary fibrosis with coronavirus is the result of inflammation, its treatment is aimed at suppressing the excessive work of fibroblasts and reducing the area of inflammatory changes.
- Glucocorticoids (dexamethasone, methylprednisolone) are usually prescribed, starting with moderate lung damage. More often, the indication for their use is the need for oxygen support. Tablet or intravenous forms of drugs are used. Doses and duration of the course depend on the levels of C-reactive protein and ferritin: For the first three days in case of severe Covid, methylprednisolone is prescribed at a dose of 1 mg/kg/intravenous every 12 hours, or methylprednisolone 120 mg/intravenously every 8 hours, or dexamethasone in dose of 20 mg/day intravenously for 1 or 2 administrations.
- Then they go on maintenance doses of tablet drugs: 6-12 mg per day of methylprednisolone.
Among the drugs that directly affect the inhibition of fibrosis, longidaza and nintedanib can be used today.
- Longidase is used in the form of a lyophilisate for the preparation of an injection solution. 3000 ME is administered intramuscularly once every 3-5 days. The course includes 10 injections.
- Nintedanib is a cytostatic drug. Actively inhibits the work, migration and maturation of fibrin-producing cells. The drug is also an antitumor drug. Prescribed according to strict indications. Not used in conjunction with anticoagulants. May cause bleeding and liver damage. Contraindicated for pregnant women, breastfeeding women, people with liver or kidney failure, or problems with the blood coagulation system.
Bronchodilators are used to ease breathing in cases of severe pulmonary fibrosis:
- Short-acting beta-2 agonists: salbutamol, fenoterol (Berotec).
- Short-acting anticholyregics: ipratropium bromide (Atrovent, Berodual).
- Long-acting beta-2 agonists: formoterol, indacaterol (Onbrez), salmeterol.
- Long-acting anticholinergics: glycopyrronium bromide (Sibri Breezhaler), tiotropium bromide (Spiriva, Spiolto).
- Inhaled glucocorticoids: beclamethasone, mometasone, budesonide, fluticasone.
- Fixed combinations: glycopyrronium bromide + indacaterol, tiotropium bromide + olodaterol, umeclidinium bromide + vilanterol, beclomethasone + formoterol, budesonide + formoterol, fluticasone + salmeterol.
In 2012, researchers from Belgium published findings on the effectiveness of ursodeoxycholic acid in inflammation of not only the gastrointestinal tract, but also the respiratory tract. These are the drugs:
- Ursosan;
- Ursofalk;
- Ursodeoxycholic acid;
- Ursodez;
- Grinterol;
- Urdoxa;
In 2021, experimental work by Chinese scientists proved that UDCA helps prevent pulmonary edema and fibrosis.
Forecast
The prognosis for idiopathic fibrosing alveolitis is unfavorable - survival is worse than for malignant tumors. Increasing fibrosis in the natural course of fibrosing alveolitis with the presence of a “honeycomb lung” significantly worsens the patient’s condition. Life expectancy ranges from 2 to 6 years: in acute cases - 2 years, in subacute cases - 2-4 years. With adequate treatment, it is possible to improve the quality of life and its duration. Esbriet increases median survival to 6.9 years .
In cases of secondary pulmonary fibrosis, the prognosis depends on the underlying disease, the extent and rate of progression of fibrosis, as well as the presence of complications ( bronchiectasis , emphysema , respiratory failure ). The prognosis also depends on the type of formation of pulmonary fibrosis. It can form as cords or as a honeycomb lung when the alveoli are affected.
Severe fibrosis in any part of the interstitium of the lungs, as well as atelectatic fibrosis (after pneumonia or as a result of bronchial closure) are favorable types. These types of pulmonary fibrosis do not affect the ventilation and diffusion function of the lungs, and therefore do not lead to severe respiratory failure. If we consider acinar fibrosis and “honeycomb lung”, in which the entire acinus and alveoli are affected (diffusion of gases occurs in them), then they lead to severe respiratory failure. These types of fibrosis are considered unfavorable in terms of prognosis and life expectancy. “Honeycomb lung” is the most unfavorable prognostic sign, especially in the presence of large “honeycombs” or alternating small and large ones located in the lower parts of the lungs.
Fibrosis in silicatosis and carboconiosis progresses slowly, so the prognosis for life is favorable. Silicosis also has a favorable prognosis, but if it is complicated by tuberculosis and spontaneous pneumothorax , the course of the disease and prognosis are unfavorable.
Complex treatment of pathology
How to treat pulmonary fibrosis? It is impossible to completely get rid of the disease. His treatment is aimed at:
- To stop the process,
- Prevention of asphyxia,
- Preservation of the normal state of healthy tissues.
Specific therapy is prescribed by a pulmonologist. In acute cases of the disease and the presence of inflammatory processes, hospital treatment is necessary.
The main direction of medical action is to eliminate the cause of the pathology.
In the absence of obvious clinical manifestations, specific therapy is not required.
For inflammation, the following are prescribed:
- Expectorants;
- Mucolytics;
- Antibiotics.
Episodes of heart failure require the use of:
- Potassium preparations;
- Cardiac glycosides.
To eliminate allergic reactions, glucocorticoids are needed. In case of suppuration and destruction of lung tissue, surgical intervention is required to resect the affected area. Physical methods of conservative treatment:
- exercise therapy;
- Chest massage;
- Physiotherapy;
- Walks in the open air.
The latest innovation in the field of pulmonology is the use of stem cells in fibrotic lung diseases. Using this method, gas exchange and the structure of the respiratory organs are improved.
In advanced stages, lung transplantation is indicated to save the patient's life.
Dietary nutrition is used in treatment. The diet is aimed at accelerating repair in the lungs and reducing protein loss in sputum. High content foods shown:
- Calcium;
- Copper;
- Potassium salts;
- Vitamins A and B9.
List of sources
- Gavrisyuk V.K., Dzyublik A.Ya., Monogarova N.E. Idiopathic fibrosing alveolitis // News of medicine and pharmacy. 2008. No. 256. from 22-24.
- Interstitial lung diseases: a practical guide / Ed. ON THE. Mukhina. M.: Litterra, 2007.
- Sakharchuk I.I., Ilnitsky R.I. Inflammatory diseases of the lungs and pleura. Kyiv; "Book Plus". 2006 – 295 p.
- Aisanov Z.R., Kokosov A.N., Ovcharenko S.I., Khmelkova N.G., Tsoi A.N., Chuchalin A.G., Shmelev E.I. Chronic lung diseases. Federal program. RMJ, 2001; No. 1: p. 9 – 33.
- Ivanova A. S. Fibrosing processes / A. S. Ivanova, E. A. Yuryeva, V. V. Dlin. M.: Overlay, 2008. 196 p.