A polyp is an elevation above the level of the mucous membrane of a hollow organ. This is a benign neoplasm that has a different histological structure. Adenomous polyps of the rectum are associated with a high risk of developing a malignant tumor. They are considered precancerous conditions. It is likely that they will develop into colorectal cancer. For this reason, when an adenomatous polyp of the rectum is identified, proctologists at the Yusupov Hospital offer the patient to remove it.
Doctors at the proctology department are fluent in all methods of surgical interventions on the rectum. Surgeons masterfully perform endoscopic and abdominal operations. Patients undergo a comprehensive preoperative examination, which allows us to identify all contraindications to the operation and avoid complications. Sometimes proctologists perform surgery after the patient has been cured of concomitant pathology.
Cause of rectal polyp formation
The definitive cause of benign neoplasms in the rectum has not yet been established. Most scientists agree that the inflammatory process plays a key role in the formation of polyps. The following facts support this:
- Many patients who were diagnosed with a polyp in the rectum had a history of inflammatory bowel disease - Crohn's disease, ulcerative colitis, proctitis.
- Most polyps are located in places where the intestine is subject to constant trauma and irritation from intestinal contents.
- When examining a piece of tissue under a microscope (histological examination), elements of inflammation are detected in the mucous membrane adjacent to the polyp.
Another important factor leading to the development of polyps in the rectum is hereditary predisposition. The likelihood of developing polyps is higher if there are blood relatives who have been diagnosed with this, and the more such relatives, the higher the risks.
In addition, there are several genetic diseases in which there is a high probability of the formation of polyps in the rectum with their subsequent transformation into colorectal cancer:
- Familial adenomatous polyposis. A large number of polyps form in the large intestine, including the rectum. They begin to develop at a young age and if not removed, they will develop into cancer.
- Gardner's syndrome is a type of adenomatous polyposis. Its peculiarity is that in addition to polyps, there are osteomas in the intestine - benign bone tumors, which are mainly localized on the skull.
- Peutz-Jeghers syndrome. Already from childhood, polyps begin to grow throughout the gastrointestinal tract, including those located in the rectum. Histologically, neoplasms differ from ordinary polyps because they have more developed connective tissue. The probability of malignant degeneration is quite high and amounts to 5-10%.
Is prevention possible?
The basis for the prevention of colon cancer and polyps is screening, although there is evidence of the preventive effect of other factors. For example, some studies show that calcium intake prevents the recurrence of colon adenomas (unfortunately, it is still unknown whether calcium has a protective effect against colon cancer), while other studies show that vitamin D helps prevent the development of colorectal cancer .
This issue is still under study, but there are already proven and tested recommendations: the risk of developing dangerous intestinal diseases will be significantly reduced if you develop healthy habits - include more fruits, vegetables, grains in your diet, reduce fat, avoid. Physically, you need to maintain a healthy weight.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Types of rectal polyps
Adenomatous (glandular) polyps are formations of glandular or, as it is also called, secreting epithelium. Externally, they have the shape of a mushroom on a thin stalk, or a node located on a wide base. Their sizes are different and can vary from a few millimeters to several centimeters. The surface of the polyp can be smooth, velvety or bumpy, like that of cauliflower.
Usually there are no symptoms, and neoplasms are discovered during preventive examinations or during examinations for other diseases localized in the rectum.
A type of glandular polyp is villous polyp. They are large in size and located on a flat base. Their surface is velvety or bumpy. Compared to other types of polyps, they have the greatest risk of malignant transformation. In some cases, they can cause hypersecretion syndrome - copious secretion of mucus from the anus and a decrease in potassium levels in the blood. Patients complain of itching in the anus.
Fibrous polyps. Externally, they have the shape of an oval or round node, sizes vary from a few millimeters to 4 cm. The surface is whitish or grayish in color, often covered with ulcers. Such polyps are located along the dentate line of the anal canal. Microscopy reveals squamous epithelium, and the stroma (the main supporting structure) reveals large amounts of connective tissue, particularly collagen, fibroblasts and mast cells.
Diet
The diet is prescribed depending on the patient's condition. Diet numbers suggest a course of treatment and compliance with the regimen according to recommended medical standards.
- If a patient develops colitis, the doctor prescribes diet No. 4. Thus, the load on the mucous membrane will not be as heavy.
- For constipation, diet No. 3 is prescribed. The products are selected in such a way that the stool becomes less liquid.
- But if the patient feels well and does not have severe forms of the disease, he is prescribed diet No. 15.
Symptoms of rectal polyps
In the vast majority of cases, neoplasms in the rectum do not have any specific symptoms that could indicate the presence of this pathology. Therefore, they are most often discovered during examination for other diseases. But if there are many of them and they are large in size, some signs can be detected.
Symptoms may include:
- Discharge of mucus from the anus, often accompanied by itching (villous polyps).
- Feeling of a foreign body in the anus (with prolapse of a rectal polyp).
- Rectal bleeding, discharge of blood during bowel movements.
- Streaks of blood on the surface of the stool.
- Prolonged constipation or diarrhea.
- Decreased hemoglobin (iron deficiency anemia) due to chronic bleeding.
- Stomach ache.
These symptoms are nonspecific and can be observed in other diseases - chronic hemorrhoids, rectal cancer, etc.
Classification
Depending on the histological structure, these neoplasms are classified as follows:
| Type of polyps | Description |
| Ferrous | Fibrous polyps of the rectum develop from glandular tissue and are observed in approximately 20% of patients. In most cases, they look like a mushroom on a wide stalk, but they can also have a branched or spherical shape |
| Villous (adenomatous) | This type of growth is also formed from epithelial tissue. They are nodes on short wide legs or creep along the walls of the rectum. Villous (hairy) polyps are rich in blood vessels, so they have a bright red color. The size of these formations can reach 3 cm. They often ulcerate and bleed. In 40% of cases these growths become malignant |
| Hyperplastic | They are small cysts based on tubular depressions in the intestinal epithelium. These are small neoplasms, the size of which does not exceed 0.5 cm. They have a soft consistency and rise slightly above the surface of the mucous membrane, so the disease in most cases is asymptomatic |
Fibrous polyps are quite dense and practically do not differ in color from the mucous membrane. They can reach 2–3 centimeters in diameter. Such neoplasms practically do not bleed and ulcers do not appear on their surface, but in some cases they can degenerate into a malignant tumor.
Neoplasms may have different histological structures
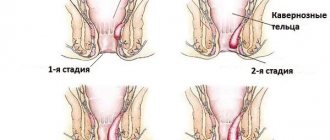
Depending on the number of tumors, they are classified as follows:
- diffuse : their occurrence is observed in familial polyposis, they are almost impossible to count;
- single : most often this is one large growth;
- multiple : usually polyps grow in groups (in some cases chaotically).
Diagnosis of polyposis in the rectum
As we have already said, rectal polyps have a hidden course and may not manifest themselves in any way. Therefore, preventive examinations are key. In some countries, there are even screening programs when people over a certain age (usually after 50 years) are recommended to periodically undergo a total colonoscopy with the immediate removal of detected benign tumors.
This study involves examining the entire surface of the colon using endoscopic equipment - a flexible tube with a cold lighting system and a video camera. The endoscope transmits a magnified image of the area under study to the monitor, which allows visualization of polyps several millimeters in size. In addition to a video camera, it is equipped with manipulators that will help you immediately remove a detected tumor and send it to the laboratory for a more detailed study. A shortened version of colonoscopy is sigmoidoscopy, when the rectum and part of the sigmoid colon are examined using an endoscope.
Another diagnostic method is sigmoidoscopy - examination of the rectum and partially sigmoid colon using a sigmoidoscope. The latter has the form of a rigid tube with a system of lighting and air supply to the intestine to straighten its wall. There is no camera presenting an enlarged image on the screen. The examination is carried out exclusively under the visual supervision of a doctor. However, the device allows you to take a biopsy and remove polyps.
In addition to visual diagnostics, the following studies can be used:
- Fecal occult blood test. Identifies polyps with an ulcerated surface that bleeds.
- Computed and magnetic resonance imaging. These methods are well tolerated by patients, but only large polyps larger than 1 cm are detected. Small neoplasms are often not diagnosed.
- Irrigoscopy. X-ray examination of the colon while filling it with a radiopaque agent. It has low sensitivity and can detect only large tumors.
Thus, today the gold standard is endoscopic examination. It will not only identify the tumor, but also simultaneously remove it.
Diagnosis of intestinal polyps
The main means of diagnosing the underlying disease is screening. This is the gold standard for diagnosing the disease and the most effective strategy - screening allows us to detect a problem before it develops into a malignant disease. Screening can also detect cancer at an early stage, and starting treatment at this stage is much safer and more effective.
Since a colorectal polyp is considered a precancerous condition, special attention is paid to identifying this pathology during screening.
During screening, two tests are performed. The stool is first examined for occult bleeding. This method detects even small amounts of blood in the stool that is not visible during gastric emptying. However, a positive test result does not mean the presence of a polyp, especially cancer. This only indicates that there is hidden bleeding in the body. Colonoscopy helps determine its cause.
Colonoscopy is the most sensitive method for detecting polyps and cancer. During the examination, a thin tube with a camera is inserted into the back of the body. The doctor sees the intestinal mucosa with his own eyes. The examination also allows you to do a biopsy - take a sample of polyp tissue for histological examination. A wire loop is also placed over the colonoscope to remove polyps painlessly.
Colonoscopy
If the result of a stool test is within the normal range, a repeat test is prescribed after two years, but if prescribed by a doctor, it can be done earlier.
Polyps can be detected using a virtual colonoscope (CT colonography), a moving sigmoidoscope, and other methods, but you will still need a colonoscopy to biopsy or remove the polyp.
Why are polyps dangerous?
The main danger of polyps is malignant degeneration, i.e. transformation into rectal cancer. The risks of malignancy depend on the following factors:
- Histological structure. Villous adenomas are the most dangerous in terms of carcinogenicity. Histological examination of the removed material revealed malignant segments in situ (non-invasive cancer) in the tumor in a third of patients, and signs of invasive cancer were found in another third.
- Polyp size. The larger its size, the higher the risks. On average, polyps larger than 1 cm degenerate into cancer much more often than tumors of a smaller size.
- Form. There are pedunculated and broad-based polyps. Pedicled polyps are smaller in size and less likely to become malignant. Broad-based neoplasms are more dangerous. They can be difficult to detect during examination and to remove. If the size of the polyp is more than 2 cm, it is highly likely that it contains a villous component, which has a high malignant potential. During malignancy, the wide base promotes the migration of malignant cells into the submucosa of the rectum, which contributes to the formation of invasive cancer.
- Presence of genetic factors. Hereditary forms of polyposis have a high potential for malignant degeneration. In some cases it reaches 100% (adenomatous polyposis, etc.).
If the patient has one or more risk factors, we invite you to make an appointment with a proctologist for an examination and prescription of preventive or therapeutic measures. Our clinic employs qualified doctors with extensive experience. You can make an appointment by calling the numbers listed on the website.
Possible complications
Surgery is the only method to completely get rid of polyposis; conservative treatment is not effective. If polyps in the rectum are not removed in time, they will cause a number of complications. The most serious complication is cancer. It is also possible to develop inflammatory processes, intestinal obstruction, anemia, fissures and impaired bowel movements.
Risk of degeneration into cancer
Adenomatous polyps, localized in the rectum in 75% of cases of all types of polyps, are most prone to malignancy. The most dangerous of them are villous, branched in shape. The larger the diameter of the polyp, the greater the likelihood of its degeneration into a malignant tumor.
Polyps that are small in diameter and pedunculated are least prone to malignancy. Broad-based polyps degenerate into cancerous tumors more often due to the rapid spread of malignant cells over the surface of the mucous membrane.
Intestinal obstruction
When polyps increase in size and grow into the intestinal lumen, they can completely block it. As a result, intestinal obstruction will occur, which is manifested by acute pain in the lower abdomen. Other characteristic symptoms are nausea and vomiting 2-3 hours after eating and prolonged constipation.
Periodic vomiting can quickly lead the patient’s body to dehydration and exhaustion, constipation can lead to intoxication, which can cause the development of necrosis of the intestinal walls, i.e. to their death. If feces enter the abdominal cavity, peritonitis will occur, requiring urgent medical attention in a hospital setting.
Acute enterocolitis and paraproctitis
Enterocolitis is caused by inflammation of ulcers on the surface of polyps, which also affect healthy rectal tissue. The patient experiences typical symptoms - pain and bloating, rumbling and heaviness in the abdominal cavity, nausea and vomiting. There may be an increase in body temperature and diarrhea with an unpleasant putrid odor; the feces may contain blood. The condition is very dangerous and requires urgent medical attention, since with enterocolitis there is a high risk of perforation of the walls of the rectum.
Paraproctitis develops against the background of an infectious process in the rectum, when the infection penetrates the fatty tissue and an external or internal abscess is formed. The trigger for the onset of the infectious process can be a bleeding polyp, cracks and other lesions of the mucous membrane. The patient experiences pain in the intestine and perineum, which at first is aching in nature, and as the abscess grows, it becomes paroxysmal and pulsating. Other signs of the disease are increased body temperature, lethargy, and fatigue. The disease can develop into a chronic form.
Other complications
Other complications include:
- Abnormal stool – expressed by alternating constipation and diarrhea. Villous adenomas secrete a lot of water and salt, leading to chronic watery diarrhea. This can trigger the development of hypokalemia, when a low level of potassium is observed in the patient's blood. The symptom is dangerous for the body; a lack of potassium disrupts the functioning of vital body systems.
- The appearance of stones in feces - manifests itself against the background of chronic constipation, leading to hardening of feces and the formation of stones from them. The condition is unfavorable for the digestive system and worsens the patient’s quality of life.
- Cracks in the rectum - they are caused by chronic constipation and inflammatory processes. The patient feels pain during bowel movements, minor bleeding is possible, and if the fissures become infected, pus may be discharged.
- Anemia - forms against the background of severe or prolonged bleeding from the anus; if the bleeding is hidden, then the disease can remain a secret for the patient for a long time. The patient feels weak, has a pale complexion, and has decreased overall physical tone, but due to these symptoms he does not always seek medical help.
How to treat rectal polyps
The only treatment for rectal polyps is their surgical removal. Typically, this procedure is performed during colonoscopy or sigmoidoscopy:
- A small amount of special liquid is injected into the intestinal wall under the polyp. It will allow you to visualize the boundaries of the tumor.
- The polyp is captured and fixed with a special manipulator attachment.
- Next, it is cut off from the intestinal wall using a loop to which an electric current is applied. Large polyps can be removed in fragments, piece by piece. The electric current leads to heating of the tissue and instantaneous sealing of the blood vessel.
- If the doctor suspects the presence of a malignant component in the tumor, a tattoo is made at its location. If the diagnosis is confirmed, this will make it easy to locate this site if subsequent further examination is necessary.
- The removed polyp must be sent for histological examination to the laboratory.
In some cases, in our clinic, polyps in the rectum are removed surgically (with a scalpel) through the anus. This operation is called transanal resection. It can be performed if the tumor is located at a level no more than 10 cm from the anal canal.
Progress of the operation:
- The anal canal is widened using a speculum or retractor, and the rectum becomes accessible for manipulation.
- The polyp is excised together with a part of the rectal mucosa that is not affected by the neoplasm (especially important for villous neoplasms).
- The wound is sutured. The resulting material is also sent for histology.
If there are too many polyps in the intestine (for example, with hereditary polyposis or ulcerative colitis, their number can exceed dozens), an operation called a total colonectomy is performed. It involves removal of the colon with partial preservation of the ileum and rectum and the imposition of an anastomosis between them (connecting them to each other). This is a very complex and crippling operation, therefore it is performed according to strict indications. But only it allows you to prevent the development of malignant neoplasms in the colon.
Traditional methods
Traditional methods of treating polyps are:
- oils and ointments (iodine, honey, sea buckthorn, camphor oil);
- decoctions (pine needles, celandine, sage);
- tinctures (viburnum, celandine, walnuts);
- enemas and compresses from plant extracts, their leaves, fruits and stems.
As a rule, the therapeutic course is designed for a long time, so it will not cause harm to the human body. Before treatment, you need to make sure whether the patient has allergic reactions to certain plants. Treatment of intestinal polyps with folk remedies has a number of advantages. We include:
- environmentally friendly drugs;
- strengthening the immune system;
- subject to dosage, no side effects;
- simultaneous use of several drugs;
- 100% result, proven over centuries;
- during treatment, the body receives vitamins, minerals and other beneficial substances;
- there are no negative effects on internal organs and systems.
Compliance with general useful recommendations involves treating polyps with folk remedies. Therapy is carried out over a certain period of time. It is not recommended to interrupt it. Plants and herbs must be collected at a distance of at least 5 km from the city or highway. To preserve more useful substances, it is recommended to prepare medicines in a water bath.
Medicines can be combined with herbal natural preparations. But before this, you should consult your doctor. It is recommended to use toxic herbs with strong effects carefully. In case of side effects, stop the course and contact your doctor to find a different prescription.
Rehabilitation period after rectal surgery
The recovery period after removal of a rectal polyp takes about 2-3 weeks. During this time, it is recommended to adhere to the following rules:
- Follow your diet. The first day after surgery, absolute fasting is indicated, after which you are allowed to drink clean water. Vegetable broth is gradually introduced into the diet, after another 12 hours you can drink rice water and chicken broth. On the 3-4th day, if there are no contraindications, it is allowed to eat liquid porridge, puree from low-fat poultry varieties. Gradually, new foods are introduced into the diet: soups, boiled eggs, etc. Food should be taken regularly, in small portions, with plenty of liquid. It is necessary to exclude alcohol, hot, spicy and salty foods, as well as foods rich in fiber (raw vegetables and fruits) from the diet.
- Avoid sitting for long periods of time.
- Don't lift heavy objects.
- Avoid thermal procedures, visiting a bathhouse or sauna.
Please note that removing polyps does not prevent the occurrence of new formations, so undergo the necessary examination regularly.
Treatment
There is no conservative treatment for polyps; the only way to get rid of the disease is through surgery. The treatment tactics are determined by the doctor after a thorough examination of the patient, which includes several stages:
- determining the size and type of tumor;
- study for tumor metastasis;
- determining the location of polyps, as well as their numbers;
- determination of the structure of formation and method of attachment to epithelial tissues.
Proctologists and surgeons diagnose and make decisions on treating patients. Removal of polyps is rarely performed using abdominal surgery. Most often, endoscopy is used for this - inserting an endoscope with an electrode in the form of a loop, which captures the stalk of the polyp and trims it.
A rehabilitation period after such an operation is not required - the patient can return to professional activity the very next day. However, you will still have to follow the diet (at least 2-3 months).
Prevention of polyps in the rectum
Since the exact cause of the formation of polyps in the rectum is still unknown, there are no specific preventive measures. Nevertheless, there are certain recommendations that will reduce the risk of tumors.
- Balance your diet. Avoid constipation and diarrhea. Minimize foods that contribute to irritation of the intestinal wall (salty, spicy, spicy foods, marinades, smoked foods, alcohol, etc.).
- Maintain adequate physical activity.
- Promptly detect and treat gastrointestinal diseases.
Considering that the main danger of a polyp in the rectum is its malignancy, it is recommended to undergo timely examinations (colonoscopy) with the simultaneous removal of detected polyps. The frequency of examination is recommended by the doctor, based on the patient’s age and medical history. On average, people over 50 years of age need to undergo this procedure at least once every decade.
In the European Clinic, colonoscopy is performed by qualified endoscopists using expert-class equipment from the world-famous Olympus company, which allows this examination to be performed with maximum efficiency.
Book a consultation 24 hours a day
+7+7+78
Risk factors
Risk factors and mechanisms of colon polyps are being actively studied. Among the environmental factors, the nature of nutrition is significant, with a predominance of refined foods in the diet, which contribute to constipation and prolonged stasis of intestinal contents. Dysbacteriosis of the colon has some influence on the occurrence of polyps, reflecting a violation of local and decreased general immunity, contributing to changes in the differentiation and regeneration of mucosal cells. The role of concomitant diseases of the biliary system and impaired production of bile acids, which have a mutagenic effect on the mucous membrane, is also noted as a risk factor. Active chronic inflammation and mucosal dysplasia play a certain role in the occurrence of polyps.