Causes and risk factors
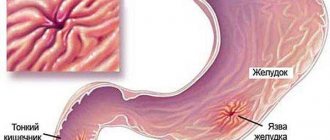
A perforated duodenal ulcer does not belong to a separate type of peptic ulcer, but is considered a dangerous complication, which is characterized by perforation of the intestinal walls. Through holes allow food debris into the abdominal cavity, which leads to constant irritation and disruption of the bacterial nature of the peritoneum. Against this background, an infection of the body occurs, which requires immediate surgery.
The manifestation of an acute ulcer is more typical for the anterior wall of the duodenal process of the duodenum. Most often, the wounds do not exceed 3 mm in size, in rare cases they reach 10 mm.
The most common cause of a perforated duodenal ulcer is untimely detection and asymptomatic progression of a simple ulcer, which as a result corrodes the intestinal wall to the point of perforation. Frequent signs of exacerbation of the disease include neglect of the advice and instructions of the doctor, refusal of diet and bad habits. There are situations when a perforated ulcer develops against the background of seasonal exacerbations: gastrointestinal diseases worsen in the autumn-spring period.
The following negative aspects can lead to perforation of a duodenal ulcer:
- Increased acidity of gastric juice due to poor diet or exacerbation of other stomach diseases.
- Sudden pressure surges.
- Refusal to diet and regular consumption of unhealthy foods (fried, fatty, foods containing harmful chemical additives and dyes).
- Having bad habits - smoking, drugs, alcohol.
- Regular use of non-steroidal medications that have a negative effect on the stomach (Aspirin, Diclofenac, Ibuprofen, Ketorol, etc.).
- Severe emotional and nervous shock.
- Genetic predisposition.
- Helicobacter pylori infection.
- Non-compliance with diet for peptic ulcer disease.
- Excessive physical activity after eating.
Additionally, the depletion and weakening of the protective functions of the intestines is affected by hormonal imbalance and nutrient balance in the body.
Stages of the disease
The clinical picture of the disease includes the following stages:
- Chemical peritonitis (abdominal shock, primary shock).
- Bacterial peritonitis (serous-fibrous peritonitis and systemic reaction, a period of imaginary well-being).
- Diffuse purulent peritonitis (severe abdominal sepsis).
In order to prevent the formation of a perforated ulcer, timely diagnosis and treatment of gastric and duodenal ulcers are indicated.
Classification
Classification of perforation of a duodenal ulcer is carried out according to several main parameters. By type they distinguish:
- perforation of a chronic ulcer;
- perforation of the acute phase of the disease.
According to the type of occurrence of the disease, they are distinguished:
- A typical development in which food masses enter the abdominal cavity. The disease goes through 3 main stages - severe pain shock, followed by a period of improved well-being (false well-being), and then the development of acute peritonitis.
- Atypical development - it is characterized by a covered perforation, in which the through wound is obscured by another organ, which, in turn, prevents the flow of intestinal contents into the abdominal cavity. But at the same time, processed food gets into the omentum or adhesive areas, which leads to bleeding.
Depending on the type of disease, the symptoms and further course of treatment vary significantly. The first option is characterized by severe pain, which is expressed even upon palpation. In the second option, due to the covering of the perforation, the symptoms may characterize a number of other diseases, which complicates the diagnosis.
Statistics show that in more than 80% of cases, perforation occurs in the walls of the duodenal bulb. Also, the disease is more common among the young population, and stomach ulcers are common among older people.
Complications
Severe postoperative consequences appear more often the more time has passed since the onset of the inflammatory process. Due to the lack of control over quality hygiene of the abdominal cavity, limited, local peritonitis with abscesses in the subdiaphragmatic, subhepatic, interintestinal, and Douglas space is possible.
Due to failure of the sutures on the intestine with repeated infection of the abdominal cavity with duodenal contents. Dysfunction of intestinal patency due to intestinal paresis or errors during surgery. Development of bronchopneumonia due to forced lying position. Decreased immunity due to strict diet.
Symptoms
At different stages of a perforated duodenal ulcer, symptoms may vary. The first phase is characterized by the leakage of duodenal contents into the peritoneum, which is accompanied by severe pain. Depending on the flow strength and the size of the perforation, the period can last 3-6 hours. The pain can radiate to the pelvic area. If the patient has recently eaten, vomiting with particles of bile and blood may occur. Additionally, there is a decrease in pulse and blood pressure, general pallor and tone of the abdominal muscles.
During the second phase, a false improvement in well-being occurs, the indicators return to normal, but at the same time there is a feeling of thirst, dryness in the mouth, and the tongue changes color. At the last stage, the patient’s condition noticeably worsens, body temperature rises, the abdomen swells, and vomiting begins. On palpation, you can feel fluid in the peritoneum.
Covered perforation
Duodenal contents are thrown into the peritoneum, but this area is hidden by the omentum, liver or intestines. You can identify it by the following signs:
- small size of the through wound;
- low filling of the organ at the time of perforation;
- proximity of the through wound to the liver, omentum, intestines, and gall bladder.
The process occurs in three stages:
- Perforation. The phase is characterized by sharp pain in the epigastrium or upper abdomen. Possible collapse.
- Calm. Pain is reduced, muscle tension is relieved, and there is no free gas in the peritoneum.
- Complications include local purulent inflammation of the peritoneal tissue, and less commonly, diffuse peritonitis.
This type of perforation develops slowly.
Diagnostics
The primary examination is carried out by the attending physician. He takes basic indicators - body temperature, pulse and blood pressure, conducts an external examination of the patient and palpates the abdomen and sternum. Only after this a referral for further examination is issued.
Clinical data
Immediately after the initial examination, the doctor prescribes a number of clinical studies, which include:
- A standard blood test allows you to detect leukocytosis (with perforation there is a shift of equality to the left), an increase in the erythrocyte sedimentation rate and determine the granularity of neutrophils.
- Urine analysis reveals an increased protein content, which indicates a disruption in the functioning of internal organs.
- Blood biochemistry - with intestinal perforation shows an increase in the amount of urea, globulin, bilirubin, alanium aminotransferase, etc.
Inspection using palpation and auscultation
During the examination, the difficulty of making a diagnosis lies in the fact that the tone of the abdomen and thoracic region may indicate a number of other diseases of the internal organs. The obvious presence of fluid in the abdominal cavity is palpable only in phase 3 of the disease. In the second phase and with an atypical form of perforation, bowel prolapse can be felt during a rectal examination.
X-ray diagnostics
To detect exacerbation of peptic ulcer, X-ray examination with the introduction of a contrast agent is used. A perforated duodenal ulcer appears as a defect in the wall, and stenosis is detected (a mixture of barium leaks through the hole, and this is immediately visible on the x-ray).
Endoscopic diagnostics
A gastroscopic procedure for the mucous membrane of the stomach and intestines allows you to find out the location of the ulcer, its size and morphological features, and provides information about the presence of bleeding and tissue scarring. During endoscopic examination, samples of materials can be taken from the stomach and duodenum of the duodenum for biopsy and histological examination.
In order to find or exclude infection with the bacterium Helicobacter pylori, a polymer chain reaction test and a breath test are prescribed.
Electrocardiogram (ECG)
Perforation of the ulcer is accompanied by severe pain in the epigastric region, similar to knife blows. The same symptoms are characteristic of a heart attack, therefore, in order to exclude one of the diseases, the attending physician may prescribe an ECG. It helps to assess changes in the myocardium. In case of perforation of an intestinal ulcer, the obtained data do not change. Such a study gives results only on the second day after perforation.
Ultrasound
Ultrasound examination of the abdominal cavity during perforation of the ulcer helps to identify the inflammatory process and assess the intensity of its filling, determine the amount and nature of the fluid. In addition to this, you can directly see the perforation itself on the screen, which is displayed in the form of a regular or irregular cone. An ultrasound may be prescribed to confirm or refute ambiguous data after an x-ray examination.
Determining the location of the ulcer using ultrasound will be difficult if the patient's stomach and intestines are full. Therefore, sometimes before the procedure, medicinal cleansing of these organs is prescribed.
Laboratory research
Laboratory tests help exclude a number of other serious diseases that have similar symptoms. These include the acute phase of cholecystitis, renal and hepatic colic, heart attack, rupture of tumors of internal organs, inflammation of appendicitis, chronic pancreatitis, etc.
Diagnostic laparoscopy
If the use of other methods does not help to establish an unambiguous diagnosis, a surgical diagnostic method is used - laparoscopy. Doctors make two small holes measuring 5-15 mm in the stomach, fill the cavity with gas and insert special tubes with a video camera at the end. This method allows you to study in detail the abdominal cavity and all the organs that are located in it.
This study is considered the most effective, but requires immersing the patient in a state of anesthesia, which carries with it some risks.
Conservative measures
It is used when it is impossible to solve the problem surgically. The Taylor method is to prescribe:
- insertion of a transnasal tube for parenteral nutrition;
- applying cold to the stomach;
- powerful infusion therapy to stabilize the acid-base balance;
- detoxification measures;
- combination antibiotic therapy for a week or longer;
- periodic x-ray monitoring of the development of perforation of the duodenal region.
Along with medications, a strict diet is prescribed.
Treatment of perforated ulcers
Treatment methods for perforated duodenal ulcer are divided into 2 types:
- conservative;
- operational.
However, given that the disease is characterized by severe infectious consequences, a long-term conservative method is used extremely rarely. Most often, after an initial examination by a doctor, patients are sent for urgent hospitalization to the surgery department and additional procedures and studies are performed there.
If a perforated ulcer is suspected, the patient is prescribed oxygen inhalation and infusion of infusion drugs to replenish the current losses of the body. It is not recommended to use analgesics, especially those of a narcotic nature, in treatment. They can negatively affect the patient's condition and lead doctors on the wrong trail.
Conservative treatment
The conservative technique excludes the possibility of surgery; treatment is carried out with medication. The main effect of the drugs is aimed at localizing and eliminating the bacterium Helicobacter pylori, which causes peptic ulcers.
The treatment regimen is as follows:
- Strong antibiotics are taken for 2 weeks, which eliminate the bacteria and remove its waste products (Amoxicillin, Metronidazole, etc.).
- To restore the secretory activity of the stomach, drugs are used that reduce acidity and block histamine receptors in the mucous membrane (Omeprazole, Ranitidine, Lanzoprazole, etc.).
- To relieve pain syndromes, gel antacids and local anesthetics are prescribed.
- Bismuth, Misoprostol and their derivatives are taken as a protective mechanism for the intestinal mucosa.
Treatment is prescribed only by a doctor; spontaneous use of drugs can cause irreparable harm to the body and aggravate the course of the disease.
Surgery
It consists of performing a laparotomy operation. The patient is placed under general anesthesia, and the abdomen is opened by making a longitudinal incision in the abdominal muscles. At this time, the remaining accumulated air and gases may leave the body, which will be indicated by a characteristic sound. In addition, a cloudy liquid with a gray-greenish tint may be found in the voids of the abdominal cavity. It is removed with a special suction.
Upon further examination of the duodenum, surgeons look for the area affected by the ulcer; it stands out against the general background in white. The size of the ulcer can reach 30 mm. The perforated area is located closer to the center, most often its diameter does not exceed 5 mm. The presence of adhesions in the intestine somewhat complicates the field of view for surgeons, so they begin to look for a puncture manually. The ulcer is then sutured.
Indications for certain types of operations
The technique of surgical intervention is determined by the general condition of the patient, as well as some features of the course of the disease. In the presence of peritonitis, treatment is aggravated by possible damage to other internal organs and the formation of an abscess, which can lead to death. Surgery is performed as soon as possible in order to increase the patient's chances of recovery.
A timely operation and a course of postoperative treatment help get rid of the disease and recover quickly. People aged 20-40 years are more likely to suffer from intestinal ulcers. The condition may be caused by poor diet and frequent stress. However, at this age, the chance of a full recovery and absence of relapses in the future increases.
Elderly people are less likely to encounter this complication, however, due to the tendency for repeated exacerbations and damage to the soft tissue of the intestine, the surgeon may decide to resect the organ.
Complications of surgical interventions
If you neglect the prescribed treatment and violate your diet, the following exacerbations of the disease may develop:
- Stenosis, which is accompanied by a narrowing of the adapter from the stomach to the intestines. Because of this, food does not pass into the intestines and accumulates in the stomach, causing constant vomiting, bloating and heartburn. Drug treatment rarely works, so another operation is required.
- Bleeding is considered the most common complication, which is accompanied by the release of blood in the stool, significant loss and blood contamination.
- Malignancy is the transformation of ulcer cells into malignant tumors. Only resection of the affected area and drug treatment can save a life.
Anatomy of the duodenum
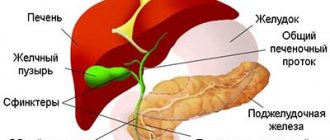
The duodenum has one task - to receive the food mass treated with the acid of gastric juice, mix it with bile and pancreatic enzymes to prepare it for entry into the alkaline environment of the intestine.
A horseshoe-like section of the digestive tube is only 12 fingers or fingers long (in diameter), connected to the stomach by a bulb, and the pancreas is tightly adjacent to the duodenum.
The duodenal bulb is so named for its great similarity, and the folds of the mucous membrane are also like those of an onion - from top to bottom, whereas in other parts of the intestine they are predominantly transverse. In the bulb, the acidic gastric secretion mixes with the alkaline intestinal secretion and it is here that ulcers most often arise, and malignant tumors, on the contrary, rarely develop - in every seventh of all those suffering from duodenal carcinomas.
Next is the descending part with the pancreatic papilla and common bile ducts opening into it; bile produced by the liver and aggressive pancreatic enzymes enter this section. In two out of three cases, it is in this part of the duodenum that a malignant process develops.
Next come the horizontal and ascending parts, the frequency of malignant tumors also goes downwards - neoplasms in these sections are quite rare.
Prevention
During the postoperative period, the patient is prescribed a diet, on which his recovery and future health depend. Strict adherence to the regimen applies to the first 4 months. Then, after consulting a doctor, new foods can be introduced.
The diet is limited by the following rules:
- the daily norm is distributed over 5 meals;
- all dishes are pureed using a blender;
- It is forbidden to eat fried, spicy or salty foods; preference is given to boiled and steamed foods;
- simple carbohydrates are completely eliminated from the diet.
Already on the 2-3rd day after the operation, it is allowed to drink still water, weak tea, jelly and rosehip decoction, and eat broths and liquid porridges. Another day, cottage cheese, boiled eggs and pureed soups with vegetable broth are introduced. After 2 weeks, steam cutlets and fish and cottage cheese casseroles are introduced. After a month, you can drink kefir and yogurt in small quantities.
After complete recovery, it is prohibited to include smoked, canned and spicy foods in the diet.
Forecast
In recent years, the number of deaths during surgery has decreased and accounts for a maximum of 7% of all patients. This figure depends not only on the patient’s condition, but also his age, and the correctness of the chosen method of operation.
In the postoperative period, the number of deaths is also possible. During the first 6 hours, a maximum of 4% of patients may die. The majority of deaths occur within the next 24 hours after surgery. During this time, up to 40% of patients may die.