Lumbar protrusion is a disorder in the intervertebral disc, which consists of protrusion beyond the boundaries of the ridge while maintaining the integrity of the ring itself. For a long time, the pathology develops without characteristic symptoms, and signs will appear only during nerve entrapment, during complications. As long as the disease does not develop into a hernia, treatment of lumbar disc protrusion is possible and can easily be treated with conservative methods.
Pain and symptoms of protrusions
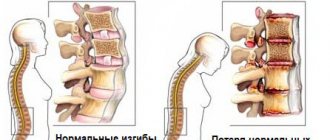
When protrusion occurs, the disc moves away from its anatomically correct position. This occurs as a result of the fact that the fibrous ring (or the so-called fibrous capsule) becomes thinner, changes and no longer holds the nucleus pulposus in the desired position. It begins to protrude from its central position, thereby leading to displacement of the intervertebral disc. This is the so-called protrusion bulge.
Since protrusion can vary in intensity, there are 3 stages:
- At the first stage, there is a slight displacement of the disc beyond the bony part of the vertebra. It itself does not collapse, only the fibrous ring thins and becomes slightly smaller in height. It is very important that the diagnosis of protrusion is carried out at this stage of the disease.
- The second stage (or stage) is where protrusion directly occurs in the lumbar region. At this stage, protrusion beyond the anatomically correct position becomes noticeable, especially when conducting various types of examinations.
- The third stage of progression results in a worse condition called a hernia.
So, in the first two stages, the tension in the disk increases. But, like any tissue, the cartilage structure has its own strength limit. As a result, the cartilage structure is destroyed. Nerves are pinched, causing pressure on the back muscles. The result is intense pain. In addition, a person is deprived of the ability to move normally and make high-amplitude movements.
It is much more difficult to cure a hernia than a protrusion. Therefore, you should pay attention to the slightest changes in your body, listen to pain, crunching sensations, and difficulties in performing any movements. And at the slightest suspicion of deviations in the normal functioning of the body, immediately consult a specialist doctor.
Naturally, the intensity of pain depends on the stage at which the disease is located. In the initial stages, there is often a complete absence of pain. A person may not feel any symptoms at all - this is the danger of the disease. But over time, the pain will definitely make itself felt. This happens because the disc begins to compress the nerve endings and change the tension of the muscle structures.
In particularly severe cases, pressure may be placed on the spinal cord. This happens when the changed fibrous ring presses on it under the pressure of the displaced nucleus pulposus.
Thus, protrusion of the lumbar spine most often has the following symptoms:
- movements in the lumbar region become constrained - a person cannot bend, bend or twist because it is either difficult for him to do this or he experiences pain;
- the pain syndrome can be mild or severe - it all depends on how much the nucleus pulposus has shifted as a whole, and negative sensations affect the pelvic region and legs;
- flaccid leg muscles – this may result in a feeling of lethargy;
- due to impaired blood circulation, swelling occurs in the legs, lower back and hips;
- also, due to the reduced blood flow, the skin from the waist and down begins to become paler, or, conversely, to blush intensely;
- Negative sensations may also include tingling in the lower extremities and thighs;
- it is very difficult for a person who has protrusion of the discs of the lumbosacral spine to perform any physical activity;
- in some cases, problems may arise with internal organs located in the abdominal cavity and pelvic area.
These are the most common signs of protrusion. Although they may differ slightly, depending on the type of disease that develops. Pain sensations may vary depending on what type occurs in each particular case. Symptoms of lumbar protrusion are more pronounced than in other parts of the back, since here the back experiences increased physical stress.
The following types of protrusion are distinguished:
Depending on how the nucleus pulposus protrudes, the following types are distinguished:
- With a circular one, the core expands evenly in all directions. Thus, the fibrous core thins evenly over its entire diameter. And the height of the disk in general decreases significantly. Due to the fact that the expansion occurs evenly in all directions, the maximum amount of nervous tissue is involved in the process of change. A person experiences mild pain almost from the very beginning of the disease. This type is characterized by a chronic course.
- Diffuse - in this case, the nucleus pulposus presses on the fibrous ring on only one side, so the ring may not withstand and rupture. And in this case, a hernia already occurs. This type is most typical for locations in the lumbar region.
- Dorsal protrusion of the intervertebral disc occurs when it protrudes into the region of the canal through which the spinal cord passes. Dorsal protrusions of the lumbar discs are dangerous because they infringe on the column canal.
This puts pressure on the spinal cord, so nerve signals travel worse, and as a result, a person can be completely or partially paralyzed. This is what threatens protrusion for human health.
You might be interested in the article about “All about intervertebral disc protrusion”!
Depending on how much the cartilaginous structure protrudes beyond the vertebrae, the following types of protrusion are distinguished:
- Lateral occurs when protrusion occurs on the right or left side of the axis. Quite often in these cases, pinched nerve roots occur with all the ensuing consequences.
- Posterolateral - at the first stage, the protrusion first occurs in the posterior direction, and then in the lateral direction.
- Median occurs when the cartilage moves towards the spinal cord. Stagnation of cerebrospinal fluid occurs, nerve conduction deteriorates, and blood circulation is disrupted.
With the development of the posterior type, the protrusion goes in a backward direction, which also involves a large amount of nervous tissue, and, consequently, causes pain and changes in the organs of the peritoneum and pelvis.
It is worth noting that depending on a person’s lifestyle, he may have a predisposition to the formation of one or another type of disease.
Classification and size ↑
Classification depending on the direction of exit of the nucleus pulposus:
- Central. Located in the midline in front of the vertebra.
- Posterior (or dorsal). Located in the midline posterior to the vertebra.
- Left-handed. Located on the left lateral side of the vertebra.
- Right-handed. Located on the right lateral side of the vertebra.
- Foraminal. It is located at the opening from which the nerve root emerges.
- Medial (or median). The disc is split exactly along the radius, the hernia is directed from the center of the vertebra to the periphery.
- Posterior median. It is a type of median or middle hernia, and is directed strictly backward.
- Paramedian. Located next to the median hernia.
- Circular. Circumferential damage to the disc is observed.
- Diffuse. The formation of multiple hernias both at the same level and at different ones.
Classification of hernias by size:
- protrusion – from 1 to 3 mm;
- prolapse or prolapse of the disc – from 3 to 6 mm;
- the hernia itself is from 6 to 15 mm.
Causes of protrusion
The main reasons contributing to the occurrence:
- intense physical labor;
- lifting weights;
- prolonged stay in an anatomically incorrect static position;
- changes in metabolism - due to which the nutrition of bone and cartilage tissue deteriorates;
- disturbances in the speed of the bloodstream - if the blood flow is reduced, it means that it does not carry the proper amount of oxygen and all nutrients;
- make physical activity (correct and beneficial for the body) regular - at least twice a week for 40–50 minutes;
- extra pounds are definitely of no use to a person, in any case, because increased weight causes a greater load not only on the post, but also on all other joints and bones in the body;
- age - the older a person becomes, the slower metabolic processes occur in the body, and this, in turn, leads to inadequate nutrition of bone and cartilaginous structures and causes their degenerative changes;
- injuries - with any, even the most minor damage, nutritional functions can be disrupted, and this, in turn, leads to improper development and functioning;
- diseases in this part of the body, such as curvature of the spine, scoliosis and others, are harbingers of the disease.
This disease is quite insidious. Signs of lumbar protrusion may be similar to other diseases of this system. Therefore, you need to be very careful about your body and devote enough time to health. First of all, engage in proper physical activity. Since it is physical therapy that can become not only one of the effective ways to cure generative changes in the back, but also become an excellent means of preventing the disease.
And, most importantly, at the first signs or suspicion of illness, immediately contact a highly qualified doctor. Since only he can diagnose protrusion of the discs of the lumbar spine and prescribe the appropriate comprehensive treatment.
Diagnostics
Diagnosing pathology is not so difficult. First, the patient undergoes an examination and interview with a neurologist.
, after which, if indicated, the doctor refers the person to an MRI or CT scan. Such methods will allow you to visualize the structures of the spine and examine them, determining the condition of the vertebrae and cartilage tissue. Ultrasound and conventional x-rays will not provide the same level of information, therefore they are prescribed only as auxiliary diagnostic methods.
How to cure lumbar protrusion
Not everyone knows that treatment of protrusion of lumbar spinal discs is a rather labor-intensive process that requires a complete change in lifestyle. It is necessary to influence not only the negative symptoms that interfere with a full lifestyle. But also do not lose attention to the reasons that led to protrusion of the lumbosacral discs.
Since, until the patient eliminates the negative causes, the protrusion of the lumbar spine will continue to progress. If this can be done, then the disease can be stopped. In the vast majority of cases, it is not possible to completely restore health, but the stage does not progress to a more serious one.
After a comprehensive examination, the doctor makes a diagnosis of lumbar protrusion, the patient is comprehensively prescribed several types of traditional treatment:
- medications (oral, local, by injection), which are designed to eliminate pain, relieve swelling, improve blood circulation in the affected tissues, and reduce the inflammatory process;
- massage for lumbar protrusion allows you to restore altered blood circulation, thereby improving tissue nutrition with all the necessary micro and macroelements, vitamins and oxygen;
- manual therapy or osteopathic methods - these two techniques of influence, although they differ in the manner of execution, are still intended to restore the disturbed position of the structures;
- traction of the spine during protrusion of the lumbar region allows you to reduce the load on the cartilaginous structures, return the vertebrae to the anatomically correct position, increasing the distance between them;
- yoga restores health;
- swimming strengthens the muscle frame, which allows you to relieve tension and intense workload;
- the doctor may also recommend a corset for protrusion of the lumbar spine to prevent the lumbar spine from moving even further;
- various methods of physiotherapy;
- In addition, doctors also recommend changing the nutrition system, making the menu rational and healthy.
It is important to remember that injections for lumbar protrusion are prescribed and performed only by a specialist in case of intense pain syndromes that do not allow a person to fully live and carry out their activities. Injections for protrusion are performed exactly in the area where a person feels the most uncomfortable pain, that is, where the degenerative change has occurred.
If most of the measures listed above are taken in the process of restoring the body, then treatment of lumbosacral protrusion has a positive prognosis in the future for the patient.
Medicines
First of all, the doctor prescribes drug treatment for lumbar protrusion. It is designed to relieve the main symptoms. This is the first component, the first step that must be taken in order to reduce the negative consequences of the disease.
There are several groups of medications, each of which affects a specific symptom.
So, for example, the group:
- NSAIDs - non-steroidal anti-inflammatory drugs, such as Ortofen, Nurofen, Ketoprofen, Ibuprofen, Movalis and others are designed to reduce the level of inflammation and thereby reduce pain;
- chondroprotectors contains Glucosamine and Chondroitin in different proportions, depending on the specific drug - as a result of their use, the body receives those biological substances that are necessary for osteochondral tissue for full functioning and which come from food in insufficient quantities (Alflutop, Artron complex, Artra, Stuktum);
- muscle relaxants - designed to relieve excessive spasm in muscle tissue, thereby restoring the proper level of blood circulation (Metaxalon, Diazepam);
- to improve blood circulation, it is used when due to spasms in the muscles there is a decrease in blood flow - this is especially often felt in the brain if there is osteochondrosis of the cervical spine and other problems in this section of the column;
- glucocorticosteroids are effective in cases of intense inflammation and associated pain; they are used as injections as prescribed (Flosterone, Methylprednisolone);
- local ointments, gels and patches that relieve the inflammatory process and reduce pain locally, in a certain area - Nise, Ibuprofen, Diclofenac, Bystrumgel, Nice, Deep Relief, Indomethacin, Rescuer, Osteosanum, Artreid, Sustafast, Honey Spas, Artropant and others .
Since the treatment of lumbar protrusion is a rather complex procedure, the doctor may prescribe several medications at the same time. Moreover, they will certainly be combined with each other and mutually beneficially complement the action of each of them.
Physiotherapy
Physiotherapeutic effects can be completely different. But the doctor also necessarily includes any type of it in the process of complex influence on the disease.
When a diagnosis is made of protrusion of the lumbar intervertebral discs, the following types of physiotherapy are most often prescribed:
- Laser therapy. With the help of local exposure to a laser beam on a certain part of the column, metabolic processes in the affected tissues are stimulated. This effect causes an increase in the chances of regeneration of deteriorating cartilage.
- Magnetotherapy. It also helps improve vital biological processes.
- An ultrasound procedure, which, thanks to the action of a sound wave, destroys salt deposits, reduces muscle spasms and reduces pain.
- Electrophoresis, which uses electric current and a specially selected drug to restore cartilage tissue. As a medicine for applications, the doctor can select either those that belong to the group of chondroprotectors or non-steroidal anti-inflammatory drugs.
- UHF helps to warm the affected areas through exposure to dry heat. At the same time, cartilage is restored due to the acceleration of metabolic processes in it.
Mud therapy for protrusion - this type of physiotherapy is especially good in the early stages of the disease. It is also used in the rehabilitation of patients and those who have undergone surgery on the spinal column.
Due to the healing substances found in the mud, swelling is relieved, the inflammatory process is reduced, and muscle contractures are eliminated. All this has the most beneficial effect on the protrusion of the discs of the lumbar spine.
Massage
The most common way to relieve pain in osteochondrosis is massage.
Massage for protrusion of the lumbar spine is also a fairly effective measure of impact on degenerative changes in the back.
But it cannot be performed independently, resorting to the help of standard massage specialists.
This procedure must be specifically prescribed by the attending physician, a neurologist or orthopedist. And you should only contact a specialist who specializes in back restoration for manipulation. Since protrusion of the spine requires particularly careful handling and close attention from the massage therapist.
Most often, they perform not a general massage, but a back massage. Sometimes, due to the fact that protrusion of the lumbar discs also affects the lower extremities, the massage therapist can manipulate them as well.
This is done in order to restore blood microcirculation and lymphatic drainage not only in the back, but also in the legs, hips and internal organs of the pelvis.
Regarding the type of massage, in the case of this degenerative disease of the column, it is recommended to perform an exclusively therapeutic type of massage. It is used in cases of various back pathologies, such as scoliosis, osteochondrosis, lordosis and others.
The technique of exposure, the intensity of implementation, the number of sessions and courses are selected exclusively by a professional, based on the diagnosis that was previously made by the doctor.
Manual therapy
It is necessary to pay attention before contacting a chiropractor that this manipulation is quite a risky undertaking. After all, one wrong move and the situation will not only not improve, but may even worsen significantly.
Therefore, before manual therapy is used for lumbar protrusion, make sure that it is possible with the attending physician. And then be sure to choose a specialist chiropractor who can really make sure that lumbar disc protrusion can reduce its symptoms. To do this, it is advisable to collect all the real data and reviews about the specialist.
How does the spinal system work?
To understand the cause-and-effect relationships, we propose to go from the general to the specific.
The human spine is a column of several dozen vertebrae connected to each other by intervertebral discs. The discs act as shock absorbers: they absorb the resulting resonance during movement and help stabilize the spine, providing flexibility, firmness and elasticity. At the same time, in case of excessive loads, the discs themselves, alas, do not recover - degenerative-dystrophic changes begin in them. Simply put, the intervertebral discs become thinner, decrease in size, crack and collapse.
For a person, this process cannot go unnoticed. At first, the patient feels fatigue and tension in the damaged parts of the spine. Endurance and the ability to withstand physical activity are significantly reduced. Then the discomfort is joined by attacks of pain, which can come and disappear spontaneously or create a constant aching background. Along with the progression of disc destruction, the pain also intensifies: it becomes regular, almost unbearable and significantly limits motor capabilities. Usually at this stage the patient finally goes to the doctor and hears one of the disappointing diagnoses - protrusion of the intervertebral disc, hernia or radiculitis.
Diet for protrusion
The first thing a person diagnosed with dorsal disc protrusion or other subtypes of this degenerative change needs to do is optimize body weight. It is necessary to understand the anatomy and physiological features of the structure of the back. A person's center of gravity falls on the area around the navel. Thus, the maximum loads are concentrated precisely at the waist. And since it is this part of the human body that bears the entire mass of a person and then transfers it to the lower limbs, then, without fail, it is necessary to reduce this load as much as possible.
This can only be achieved by losing excess body weight. This is achieved by rationalizing your menu, eliminating excessively high-calorie foods, fast food products, fried, sweet, spicy, salty, fatty foods.
Your diet should include as many complex carbohydrates as possible, such as cereals and bran bread. Light carbohydrates (white flour, sugar, confectionery and sweets) should be completely excluded. Such a balanced diet will allow you to quickly, but at the same time gently (without stress for the body) reduce body weight.
The next point concerns the fact that the diet for protrusion should provide full nutrition to the cartilage and bone tissue. The body must receive all the necessary vitamins, microelements, macroelements, omega-3 and omega-6 polyunsaturated fatty acids, and other useful biochemicals.
Only in this case will it be possible, at a minimum, to stop degenerative changes in the structure of the intervertebral disc, and, at best, to achieve a recovery process. But this is only possible in the early stages of the disease.
Based on all of the above, it becomes clear that proper and rational nutrition during protrusion is one of the key points.
Of course, the ideal option would be when proper food is a regular companion in life. In this case, the person avoids as much as possible even the very appearance of this change. But if stopping the diagnosis could not be avoided, then you should listen to the following recommendations:
Include in your diet as much as possible those foods that help restore cartilage structures. These include jellied meats; jellied dishes prepared with fish and meat; jellies made with pectin and gelatin made from animal bones; meat with cartilage inclusions.
Include calcium-rich foods in your diet. These are hard cheeses; raw sesame or sesame milk; fresh, whole natural milk, unprocessed in an industrial enterprise.
Cold-water sea fish is a must on the menu. It is rich in omega 3 polyunsaturated fatty acids (PUFAs). This component is also important for the normal functioning and hydration of the cartilage structure. In addition, fish contains a lot of phosphorus, and this trace element is also a component for bone structure.
In addition to these recommendations, doctors also recommend to their patients when making a diagnosis:
- quit smoking;
- exclude vegetarianism from the menu;
- completely eliminate or minimize caffeine consumption;
- include a large amount of raw fruits and vegetables in quantities of 5 different types by color;
- Take multivitamin and multimineral supplements.
Such a diet can significantly improve the patient’s condition, although one cannot expect an instant or even quick effect. This is a long process that will take six months or more.
Prevention
The main preventive measure is to prevent osteochondrosis, since protrusion is its stage. The following factors are important for prevention:
- correct posture;
- strengthening the muscle corset;
- maintaining your weight at a normal level;
- moderate and regular physical activity: running, swimming, daily exercise, walking are useful;
- elimination of physical overload;
- lifting weights correctly - without sudden movements, from a half-squat;
- proper nutrition: exclusion of junk food, balance of proteins, fats and carbohydrates, sufficient intake of vitamins and minerals;
- compliance with the drinking regime;
- eliminating bad habits;
- correct organization of the sleeping place: orthopedic mattress, correct sleeping position;
- avoiding hypothermia.
After successful treatment of protrusion, it is also important to observe certain preventive measures. It consists of the following measures:
- exclusion of high physical activity;
- active lifestyle;
- avoidance of stressful situations;
- avoiding hypothermia;
- proper nutrition: moderate calorie content, sufficient intake of proteins and polyunsaturated fatty acids.
Disc protrusion implies the progression of osteochondrosis and the risk of its transition to the next stage - intervertebral hernia. It is necessary to promptly begin competent treatment, which involves a complex of conservative methods. Preventive measures will help to avoid such pathology.
Exercises for protrusion of the lumbar spine
All exercises for protrusion of the lumbosacral spine must be performed strictly in order to restore, and not load, this structure of the human body. Therefore, experts recommend performing certain sets of gymnastic movements that are aimed at gently strengthening the muscle frame, reducing the load on the areas between the vertebrae, and increasing blood circulation and lymph flow.
That is why exercise therapy for protrusion of the lumbar spine is recommended to first be performed in a special group, where classes are taught by a specialist in the rehabilitation of injuries and diseases of the back. This way the patient will learn to perform the exercise correctly. And this is a guarantee of not causing more damage to your health. After the movements have been practiced, you can perform them at home.
The main goal of therapeutic exercises for protrusion of the lumbar spine is the following:
- Make muscle structures stronger and more resilient. As a result of this, it is they who will take on most of the load from the person’s weight and from the physical activity that he performs.
- Strengthen the blood circulation process, thereby improving the nutrition of cartilage tissue.
- Increase the elasticity of the ligaments, which will make it possible to perform higher-amplitude movements without causing discomfort.
Physiotherapy
Therapeutic exercise for protrusion of the lumbar spine allows you to stretch the distance between two adjacent vertebrae and release pinched nerve roots and eliminate the load on compressed intervertebral discs.
As a result, the source of pain is eliminated, strengthened and strengthened muscles take on part of the load, taking it away from the spinal column, increased blood flow and lymph circulation relieve the inflammatory process. Very slowly, but quite confidently, charging during protrusion will give its positive results. But for this it is important to do it regularly and systematically.
Moreover, exercise therapy for protrusion of the lumbosacral spine should be performed exclusively in comfortable clothing that does not restrict movement and in a well-ventilated room in order to enhance oxygen supply to the tissues.
All exercises for the back should be performed as planned without sudden movements and only during the period of remission. This method of exposure is strictly not recommended in the acute stage or in case of intense pain.
Exercise can be replaced with yoga. But only for this you need to choose the right Asanas. Better yet, hire a personal yoga consultant with extensive practice experience. In this case, professionally performed yoga for lumbar protrusion can effectively influence the affected tissues and return the person to a full-fledged lifestyle.
As exercises for the lumbar region, it is recommended to perform the following types of loads:
- cat exercise, which allows you to bend and arch your back in this area;
- bending from a position lying on your stomach, pulling yourself up with your arms and legs;
- rolling on your back, clasping your knees with your hands;
- curling into a fetal position, sitting with your buttocks on your heels and resting your forehead on your knees;
- bending from a sitting position so that the chest rests on the outer surface of the thigh to the knee, and the head rests on the knees, while the arms should hang down freely.
When performing a specially selected set of exercises, you should not limit yourself only to the load on the spinal area. After all, if degenerative changes have affected the lower back, then with a high probability they can appear in other departments. Therefore, it is worth performing exercise therapy for the entire back.
Treatment
How to treat protrusion? The main method of therapy is medication. In the subacute period, the patient is prescribed physiotherapy, massage, acupuncture, and traction. Exercises from the complex of therapeutic gymnastics help well.
If conservative therapy for protrusion for 3-4 months does not give the expected effect or leads to an exacerbation, the patient is offered surgery - nucleoplasty or percutaneous discectomy. However, in most cases, they try to do it with non-surgical methods.
Medicines
To reduce pain during protrusion, relieve swelling and restore disc tissue, the following groups of drugs are used:
- non-steroidal anti-inflammatory drugs in tablets - Ortofen, Ibuprofen, Diclofenac, Ketorolac;
- painkillers and warming ointments - Voltaren-gel, Bystrumgel, Viprosal;
- oral glucocorticosteroids - Dexamethasone, Prednisolone, Cortisone;
- hormonal drugs in injections - Celeston, Tricort;
- chondroprotectors - Artra, Alflutop, Dona.
If the protrusions are very painful, the patient is given epidural blockades with Lidocaine or Novocaine.
Orthopedics
In the acute period, the attending physician may recommend wearing orthopedic structures that support the spine in a physiologically correct state.
Most often, when intervertebral discs are deformed, a Shants collar or a bandage in the form of a corset is used, covering the lower back and sacrum.
Exercise therapy and massage
This treatment of protrusions is prescribed during the period of remission. During the massage, blood circulation in the affected areas improves, and nearby muscles relax and strengthen. To achieve a stable and long-lasting effect, it is necessary to carry out a course of at least 10 procedures.
It is very good to treat protrusions with gymnastics. Specially designed exercises gently and effectively load muscles and vertebrae, improve mobility and reduce the development of degenerative processes in the discs. Regular classes are conducted under the supervision of a physical therapy instructor.
Is it possible to cure protrusion? Unfortunately, it is impossible to completely restore destroyed fibrous tissue. However, competent conservative therapy can significantly improve the patient’s condition and stop further disc deformation.
Spinal traction
Today, this procedure is carried out quite intensively in private clinics for people who suffer from this degenerative change in various parts of the back.
But it is worth noting that its effectiveness is short-term. After all, a stretched spinal column temporarily increases the distance between the vertebrae. Thus, the load on the intervertebral discs is reduced. But since the muscular frame still does not support the spine, as a result everything returns to its place. But it only adds up to an even worse condition.
In addition, performing traction, that is, stretching, is categorically not recommended for people:
- having a poor condition of the fibrous ring - when it already has numerous cracks, on the one hand, it can be greatly thinned in width, which may indicate its imminent rupture;
- chronic changes in bone structures, in the development of the spine, muscle structures, changes in the functioning of the central nervous system, as well as the spinal cord;
- having acute injuries to the spinal column or surgical manipulations performed on it, regardless of their duration.
Therefore, traction can only be performed if it is recommended by the attending physician after collecting a thorough history and a complete examination of the condition of the spine and discs between the vertebrae.
Risk factors
There are a number of factors that significantly increase the risk of developing protrusions.
These include:
- being female;
- age 35-40 years;
- sedentary lifestyle;
- constant monotonous movements of the spine;
- presence of bad habits (alcohol abuse, smoking);
- presence of diabetes mellitus;
- hypothyroidism – decreased thyroid function.
Causes
Protrusion of intervertebral discs occurs for the following reasons:
- long-term chronic diseases of the spine (rheumatoid arthritis, osteochondrosis, ankylosing spondylitis, etc.);
- overweight, obesity;
- spinal column injuries (dislocations, bruises, fractures, etc.);
- physiological age-related changes;
- curvature of the spine (kyphosis, lordosis, scoliosis);
- metabolic disorders;
- frequent everyday stress on the spine (for example, work in a summer cottage);
- regular and long-term carrying of weights.
Consequences
As a rule, complications develop at the stage when the protrusion turns into a herniated disc. Before this (at the protrusion stage), a decrease in the lumen and infringement of the spinal canal may occur if the protrusion goes inside the vertebra. In this case, paralysis and paresis occur, sensitivity is impaired, and malfunctions in the pelvic organs appear. .
What is the danger of protrusion, consequences and complications?
This is a developing disease. It does not stand still, even if it develops quite slowly. Constant changes for the worse can lead to a pathological condition called a herniated disc. It occurs when the fibrous ring cannot withstand the pressure of the nucleus pulposus and ruptures under its influence.
Until a hernia occurs, the patient must make every effort to at least stop the degenerative process of cartilage.
It is worth noting that a protrusion of 3 mm in the lumbar region is a rather critical condition when the disease passes from the second stage to the third. This is followed by a hernia. Therefore, the sooner the patient paid attention to his painful condition and began intensive treatment, the greater the chance of recovery.
Forecast
In the absence of comprehensive treatment, the prognosis for spinal disc protrusion is extremely unfavorable.
Under severe loads, the patient’s column begins to rapidly develop and grow.
Because of this, symptoms of pinched nerves arise; a person feels severe pain with any movement. Additionally, motor activity and sensitivity of the ends of the fingers are impaired. Prolonged neglect of pathology leads to disability, the person completely loses his ability to work.
Contraindications for spinal protrusion
It is very important to know what not to do if this disease occurs:
- give an excessively intense load and lift any weight with a straight back and arms straight at the elbows;
- drink excessive amounts of alcoholic beverages;
- include sweet, spicy, fatty, salty foods in your diet;
- stay for a long time in any static position that is not anatomically correct for the spine;
- drink carbonated drinks, as they help flush calcium from the body;
- live in an environmentally unfavorable region.
It is these negative factors that are additional triggers for the development of the disease. After all, in order for a particular disease to develop, including degenerative changes in the spinal column, it is necessary to be exposed to several negative factors. And even if there is an internal predisposition of the body itself to changes in cartilaginous structures, then, as a rule, it is the external negative impact that contributes to the process of destruction of the structure of the human body. In this case, cartilage tissue between two adjacent vertebrae.
Compliance with all the above recommendations and advice will help avoid illness for those who monitor and worry about their health even when the disease has not yet appeared. And of course, most importantly, these tips will help people who have been diagnosed with protrusion to reduce the likelihood of developing the disease and improve their health.