A cervical herniated disc is a condition in which part of the structure connecting two vertebrae protrudes beyond that joint. This protrusion occurs in the direction where the elements of the nervous system, the spinal cord and the nerves extending from it, as well as large vessels feeding the brain are located. The dense mass of a deformed disc, pressing on these organs, can disrupt blood circulation in them. This causes characteristic symptoms to appear.
A cervical hernia is a dangerous disease that requires prompt diagnosis and treatment. The goal of therapy: to fix the protruding part of the spinal disc inside it, allowing the peripheral structures to restore the protective “barrier”. If this condition is detected in the early stages and treated, conservative therapy has a good effect. Otherwise, in order to relieve pain and restore quality of life, it is necessary to resort to surgery. Although the latter, in light of the current skills of surgeons and their equipment, is carried out quite quickly and easily, you should not wait until indications for it appear.
Intervertebral hernia of the cervical spine: what everyone should know about
Intervertebral hernia is a disease, the essence of which is the prolapse of the jelly-like element of the intervertebral disc beyond its boundaries.
As a result, the patient's blood circulation is impaired. Most often this occurs in the spinal cord and the nerve endings emanating from it. The peculiarity of cervical intervertebral hernia is that it is the most dangerous. The fact is that this particular place is responsible for such important functions as breathing, heartbeat, mobility and sensitivity of the arms and legs.
Fortunately, the disease we are considering manifests itself almost immediately. If you experience numbness in one or more fingers from time to time, tinnitus and dizziness, be sure to seek help from a specialist.
Principles of therapy
Symptoms and treatment of a herniated cervical spine always require clarification of the diagnosis using X-rays, CT and MRI images (see What MRI of the cervical spine will show). During hardware diagnostics, both the actual size of the hernia and in which direction(s) it protrudes, as well as the presence of disc protrusions in neighboring locations are determined.
For hernias localized in the neck, an additional ultrasound of the blood vessels is performed
Cervical hernia - symptoms and treatment are interrelated. Surgery is suggested immediately if a large hernia is confirmed, which protrudes towards the spinal cord, as this threatens paralysis of the torso and limbs.
In other cases, WHO offers drug therapy and complex treatment using exercise therapy methods, with mandatory regular monitoring of the course of the pathological process. Wearing a neck brace should be determined by individual indications.
Drug treatment
For hernias of the cervical spine, the patient is prescribed the following dose:
- NSAIDs;
- muscle relaxants;
- steroidal anti-inflammatory drugs;
- homeopathic remedies.
NSAIDs quickly relieve the painful syndrome. But they do not cure the disease itself. Long-term use of these medications can lead to stomach, kidney, and liver problems.
Use of muscle relaxants
Muscle relaxants are prescribed to control muscle spasms. The most effective means are presented in the table.
Table 3. Recommended muscle relaxants:
| A drug | Description |
| The mechanism of action of this drug is determined by blocking the nerve impulse entering the brain from the peripheral nervous system. |
| Prescribed for painful muscle spasms that occur as a result of diseases and injuries of the musculoskeletal system. |
| Promotes relaxation of muscle tissue, relieves pain. |
Use of other medications
Steroid anti-inflammatory drugs help relieve pain and relieve swelling of nerve fibers. The analgesic effect lasts throughout the day.
If the patient suffers from very severe pain, he is prescribed steroid injections. The medicine is injected into the area of the tumor.
Use of homeopathic remedies
Homeopathy for cervical hernia helps:
- improving blood circulation;
- relief of swelling of the nerve roots;
- pain relief.
The doctor may recommend to the patient such local agents as Sulfur and Aconite.
Physical therapy exercises
The table presents a set of physical therapy exercises that are useful for hernia.
Table 4. Recommended exercise therapy exercises:
| Exercise | Description |
| Stretching for a cervical hernia begins with raising the shoulders as much as possible. Then you need to gently stretch the muscles. Then you need to relax. Do 2-3 repetitions. |
| First, pull your shoulders forward, then back and squeeze your shoulder blades together. Do 5-6 repetitions. The correctness of this exercise is evidenced by the pleasant warmth spreading through the muscles. |
| First you need to move your shoulders forward, then back. The number of repetitions in each direction is 4. |
| Sitting on a chair without a back, you need to stretch your upper limbs and then relax as much as possible. The back should be straight at all times. |
| First you need to bend over, then raise your head. No stretching needed. Then you need to turn your head right and left. There should be little tension in the neck. If you have a cervical hernia, you cannot perform circular rotations with your head. This may make the situation worse. |
For cervical hernias, the following should be completely excluded:
- Exercises in active sports and contact martial arts, jogging.
- Jumping from a table and a platform in the pool, as well as any jumping exercises.
- Exercises with weights for the neck muscles, lifting weights.
- Driving on bad roads in a sitting position.
Important! WHO guidelines prohibit any chiropractic treatments for cervical hernias. This applies not only to manual manipulation and traction, but also to the use of any massage. Only self-massage is allowed - shallow stroking and weak rubbing, and then only after the end of the acute period.
Water exercises
Swimming with a cervical hernia benefits the entire body
The effect of drug therapy is enhanced and the patient’s psycho-emotional state improves.
Note! A visit to the pool may be recommended to a patient after surgery.
Swimming for a cervical hernia should be combined with the following exercises in the water:
- walking in place with high limbs raised;
- squats;
- somersaults;
- vertical and horizontal turns;
- sliding in a horizontal plane.
Traditional therapy
Natural remedies are prescribed outside of exacerbation (read more here). The best recipes are presented in the table.
Table 5. Traditional recipes for cervical hernia:
| Means | How to cook | How to use |
| Melt the product in a steam bath and apply a thin layer to a thick cloth. | Apply to the affected area, cover with polyethylene, and wrap with wool. The effect occurs within 60-120 minutes. Such compresses for a cervical hernia should be done within 48 hours. |
| Grind 150 grams of fresh garlic, add 75 ml of alcohol to the pulp, cover with a lid, leave for 1.5 weeks. | Soak a thick cloth in the infusion, apply to the damaged area, cover with polyethylene, and wrap with wool. After 60 minutes, remove the compress and wipe the skin with a damp cloth. This compress is applied daily. |
| Grind the leaves of the plant. Place the mixture on a thick cloth. | Apply the compress to the sore area, wrap with an elastic bandage, and leave overnight. Repeat this manipulation for 14 days. |
Why does intervertebral hernia of the cervical spine occur?
The disease described is quite common: it is diagnosed in one person out of a thousand. Moreover, those at risk are males aged 60 years and older.
The causes of cervical intervertebral hernia are:
- age-related changes, in particular, poor circulation, due to which the tissue covering the intervertebral disc weakens.
- osteochondrosis, which is a consequence of metabolic disorders.
- regular neck injuries.
It is impossible not to note the factors that increase the likelihood of this disease. These include:
- smoking;
- sedentary lifestyle, including sedentary work;
- other diseases of the spine - for example, ankylosing spondylitis or, say, infection of the vertebrae;
- congenital defects.
Causes and provoking factors
One of the provocateurs of pathology is frequent neck injury
A cervical hernia develops for several reasons. They are presented on the plate.
Table 1. Causes and provoking factors:
| Cause | Provoking factor |
| Impaired blood circulation of the intervertebral discs. This leads to fragility of the fibrous ring. | Neck injury. |
| Development of spinal osteochondrosis. Destruction of the intervertebral disc is observed. | This occurs against the background of impaired metabolism. The main provocateur is the development of endocrine pathology. |
| Frequent cervical injuries | Unnatural neck position. |
Risk group
Hernias in the cervical spine are diagnosed in:
- basketball players;
- racers;
- wrestlers;
- boxers;
- smokers;
- knowledge workers.
Neoplasms appear against the background of congenital anomalies in the structure of the cervical vertebrae.
Signs
Signs of a cervical intervertebral hernia are:
- feeling of discomfort;
- crunching sound when turning the head (especially sharply);
- painful sensations.
If a bulging intervertebral disc pinches vessels that are directly connected to the brain, then the following is observed:
- noise in ears;
- unsteady gait;
- complete loss of balance;
- headache;
- “flies” before the eyes;
- blurred vision;
- inability to concentrate on something.
What's the diagnosis, doctor?
Trying to diagnose yourself is not a good idea. The symptoms listed above, even in their minimal manifestation, are a reason to visit a neurologist. The doctor will check reflexes and sensitivity in the shoulders and arms, then find out the location of the hernia and prescribe an in-depth examination.
There are four methods for detecting a hernia:
- Radiography.
- CT (Computed tomography).
- MRI (Magnetic resonance imaging).
- Myelogram.
Let's take a closer look at each of them.
Radiography
Radiography is a method of studying internal organs using x-rays. The final image is projected onto a special film or paper.
Important. Before the procedure, you must remove jewelry, watches and other metal objects.
X-ray
Pros: fast, inexpensive, accessible.
Cons: indicates only indirect signs of pathology.
CT (computed tomography)
Computed tomography, like radiography, is a method of examining the patient’s internal organs using x-rays. The difference is that X-rays provide a two-dimensional image, while CT provides a three-dimensional image. Thanks to the special structure of the CT machine, which consists of a ring-shaped contour, many images are obtained from different angles. The images are processed by computer.
Important. Before the procedure, you must remove jewelry, watches and other metal objects.
CT scan
Pros: CT allows you to accurately assess the condition of the cervical spine.
Disadvantages: this research method is contraindicated for pregnant and breastfeeding women.
MRI (magnetic resonance imaging)
Magnetic resonance imaging, like computed tomography, processes a lot of images and ultimately produces a three-dimensional image of the imaged area. However, MRI uses electromagnetic waves rather than X-rays. Images are obtained by reflected pulses emanating from the area under study. They are captured by equipment, processed by a computer, and then a 3D image is created.
Magnetic resonance imaging
Pros: accuracy and information content of the analysis due to good visibility of soft tissues.
Cons : MRI cannot be performed on patients with a pacemaker or those who have ferromagnetic, metal or electronic implants.
Myelogram
A myelogram is a research method in which a special contrast agent containing iodine is injected into the spinal canal through a special needle. Then the necessary photographs are taken. They show how bulging the intervertebral disc is and whether a pinched nerve has occurred.
Myelogram
Pros: thanks to the introduction of a contrast agent, the degree of narrowing of the spinal canal is clearly visible. This allows you to determine how advanced the disease is.
Cons: carried out only according to strict indications.
Conservative treatment
If a patient with an intervertebral hernia of the cervical spine notices pain in the neck and back, deterioration of hearing and vision, then he is prescribed bed rest for a week and a Shants collar is put on.
He is also assigned:
- medicines;
- exercise therapy;
- physiotherapy.
- medicines
For intervertebral hernia of the cervical spine, the following medications are used:
- anti-inflammatory drugs (Ibuprofen, Diclofenac). It is taken orally and in the form of intramuscular and intravenous injections. Eliminate inflammation and relieve swelling.
- muscle relaxants. Relieves muscle tension.
- chondoprotectors. Prevents the development of the disease.
- blockades are anti-inflammatory and painkillers injected directly into the sore spot. Relevant during exacerbation of the disease.
Diagnosis and basic principles of treatment
Symptoms of a hernia in the cervical spine may correspond to other pathologies, so the doctor’s task is to correctly determine the diagnosis and exclude the influence of other diseases on the disease. Differential diagnosis of a hernia is carried out with diseases such as diabetic polyneuropathy, cervical tumors. The influence of metastases of malignant neoplasms located in other organs cannot be excluded. During the examination, attention is paid to other chronic diseases of the main organs and the musculoskeletal system, and the presence of injuries in the past is determined. Even the smallest injuries can lead to the formation of a hernia, so the patient is advised to remember the influence of any unfavorable factors.
The diagnosis is made based on X-rays of the cervical spine, computed tomography, patient complaints and determination of changes in the area of the intervertebral hernia. Treatment of a hernia is based on the prescription of anti-inflammatory therapy, massage, physiotherapy, and mud therapy. For all spinal hernias, during the recovery period it is necessary to carry out therapeutic exercises to improve the flexibility of the cervical spine and muscle function. Physical exercises performed throughout the rest of life minimize the risk of exacerbation of the disease.
The positive effect of treatment depends not only on the competence of the treating neurologist, but also on at what stage of the pathological process the patient seeks qualified help. Therefore, any headaches, dizziness, disturbances in sensitivity and movements in the hands, discomfort in the neck are a reason for a comprehensive examination of the body.
Exercise therapy
Exercise therapy begins before the end of bed rest. Physical therapy at this time consists of short sessions of diaphragmatic breathing.
A week later, they begin to carefully move the elbow and wrist joints. You can't touch your neck yet.
After removing the Shants collar, they proceed to the main stage. It consists of seven exercises:
- Lying on your back, lightly press the back of your head onto the support.
- From the same starting position, press your forehead onto the other person’s hand.
- Lying on your stomach, press your forehead onto the support.
- From the same starting position, press the back of your head onto the other person's hand.
- While sitting, press on the other person’s hand, first with the front of the head, then with the back. As soon as it gets better, you can increase the resistance force.
- Sitting with your hands on a support, raise and lower your shoulders.
- While sitting, turn your head left and right. If it hurts, stop the exercise.
Treatment
The optimal method of therapy is determined by a neurologist, based on the results of the diagnosis. Today, two treatment options are practiced: conservative or surgical. The first option involves medication and physical therapy, the second option uses surgery.
Conservative treatment is a more acceptable option, but such therapy will only be effective if the disease is in its early stages and the blood supply to the brain has not yet been impaired. Typically, six months are allotted for all procedures. If after this time the patient shows no obvious signs of improvement, a decision will be made to proceed with surgery.
The degree of invasive intervention is determined by a neurosurgeon.
Drug therapy
After diagnostic measures have been carried out and a treatment plan has been drawn up, the patient is prescribed to wear fixing orthoses (such as the Shants collar). You will have to wear it constantly until the pain and numbness in the arms and shoulder joints disappear. Gradually, the time of wearing the orthosis is reduced.
All measures carried out as part of conservative treatment are aimed at solving a complex of problems:
- Relieving spasms from the neck muscles;
- Supplying fibrous tissues of the cervical region with nutrients;
- Strengthening the neck muscles;
- Elimination of pain syndrome.
Drug treatment involves the prescription of drugs from the following groups:
- To relieve pain, medications are used in the form of injections. The most commonly used are analgin, diclofenac, and denebol. In the future, it is practiced to take these medications in tablet form.
- Muscle relaxant drugs are prescribed to relieve muscle spasms.
- Chondroprotectors are also prescribed - drugs that promote the restoration of interarticular tissues. They need to be taken for several months, since fibrous tissue is restored extremely slowly.
- Novocaine injections are prescribed if there is severe pain in the hands, burning sensation and tingling. Do them no more than 1-2 times a week.
- Anti-inflammatory drugs - to relieve swelling.
- Drugs that activate blood circulation in the cervical spine.
- To stabilize the nervous system, medications high in vitamin B are prescribed.
The use of drugs from the analgesic group is allowed only in extreme cases, since there is a high risk of side effects from the gastrointestinal tract, including the formation of ulcers. Taking such medications is indicated only in cases where other drugs have failed.
Physiotherapy
After pain relief (usually a week after the start of treatment), the patient is prescribed one or more physiotherapeutic procedures:
- Electrophoresis sessions. The method involves applying a direct electric current to the affected area while simultaneously administering medications in liquid form through the skin. Medicines are delivered directly to the deformed area through the intercellular space, sebaceous and sweat glands.
- Magnetotherapy. Exposure to a low-frequency magnetic field improves blood circulation, strengthens the immune system and heals injuries;
- Myostimulation. The effect of low voltage electric current on the muscles helps strengthen muscle tissue.
- Traction with traction. The procedure is carried out using a special device and involves prolonged traction of the spine. The distance between the vertebrae and discs increases, as a result of which their position is aligned.
- Hydrotherapy is the effect of water jets of varying pressure and temperature on the body.
- Compresses using therapeutic mud and paraffin.
An equally important part of therapy is physical therapy.
Classes should be carried out with the participation of a specialist, since any incorrectly performed movement can worsen the patient’s condition. Exercises allow you to strengthen the muscular corset of the spine and activate blood supply to the affected areas.
Patients are also prescribed therapeutic massage. It relieves muscle tension, minimizes pressure on the nerve endings of the spinal cord, and improves blood supply to the spine. Massage sessions are carried out in specialized rooms. Massage is also used for speedy recovery after surgery.
Surgical hernia removal
If conservative treatment methods do not bring visible improvement in the patient’s condition, the attending physician decides to perform surgery to remove the hernia. After studying the medical history and obtaining all the necessary information, the council of doctors decides on the most preferable method of performing the operation. The cervical region contains large arteries, many nerve endings and blood vessels. Such operations are performed by highly qualified neurosurgeons. There are several techniques for surgical removal of a hernia of the cervical spine:
- Anterior cervical discectomy. A small incision is made on the front surface of the neck, through which the deformed section of articular tissue is removed. A bone or titanium plate is installed in its place, improving the process of bone tissue regeneration.
- Microdiscectomy is performed in the early stages of the disease to remove small hernias. The operation is performed using a surgical microscope. All manipulations are carried out through an incision no larger than five centimeters.
- Endoscopic discectomy. All manipulations are carried out using micro-instruments, the progress of the procedure is monitored through a camera that transmits the image to the monitor screen.
The latter method is considered the most preferable, since the operation is performed without extensive open intervention. Complications are extremely rare, and the likelihood of scarring is also extremely low.
Prevention of cervical hernia involves regular exercise, a healthy lifestyle and taking vitamin and mineral complexes.
Treatment of the disease will take a lot of time and effort, so adequate preventive measures will certainly be beneficial.
Surgical intervention
Surgery for intervertebral hernia of the cervical spine is performed if conservative treatment does not bring the desired result or is completely ineffective, or if the blood supply to the brain is seriously impaired. It comes in three types:
- Discectomy and spondylonesis. A small incision is made in the skin, through which the surgeon penetrates the damaged area and removes the exfoliated tissue. The resulting void is filled with bone mass.
- Prosthetics.
- Removal of exfoliated tissue without a substitute or prosthesis.
Each type of operation has both pros and cons. The choice is made by the surgeon based on the characteristics of the disease.
Remember that untimely treatment of intervertebral cervical disc disease can lead not only to disability, but also to death. Therefore, if you have the slightest suspicion of this disease - a feeling of discomfort, pain in the neck, a crunching sound when turning your head - sign up for a clinic as soon as possible.
Consequences and complications
A cervical hernia left untreated for a long time not only affects the appearance of pain, but can also cause other pathologies. As a result of a decrease in the distance between the vertebrae, their bone tissue grows, which further increases the likelihood of radicular syndrome. The most likely complications of a herniated cervical spine are:
- The disorder of the basic movements is expressed in the weakness of the hands, the inability to perform some movements. The normal mobility of the muscles of the upper limb and shoulder girdle decreases. The most serious complication may be paresis or paralysis.
- Skin sensitivity disorder. In the first stages of hernia development, increased sensitivity of the skin is determined; later on, on the contrary, it decreases. A feature of an intervertebral hernia is a loss of sensitivity, first from the fingertips, then the symptoms spread to the hands, forearms and above.
- Infringement of the contents of the spinal column, that is, the spinal cord. This condition is considered a serious complication and requires immediate medical attention. Pinching of the spinal cord above the 4th vertebra can lead to respiratory paralysis. Pathology developing at the level of the 4th and 5th vertebrae provokes flaccid paralysis in the arms. Infringement of a hernia between the 6th and 7th vertebrae leads to paralysis of the lower and upper extremities; a distinctive feature is the preservation of mobility of the elbow joint.
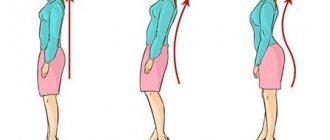
- The constant forced position of the neck, which reduces pain, leads to weakening of the muscles on one side and to their tension on the other. All this causes an incorrect anatomical position of the cervical spine and affects the occurrence of its curvatures, which, with a long course of the disease, is visible to the naked eye.
As a result of the pathological effect on the vertebral artery, vascular disorders occur, manifested by the following symptoms:
- Sudden changes in pressure.
- Dizziness, tinnitus, periodic headache, poorly relieved by analgesics. Patients note increased pain in the head after a forced, uncomfortable position of the neck.
- Violation of visual function - fog and spots are detected before the eyes, the field of vision narrows, the image of the visible object blurs. The eyeballs may twitch randomly.
- Hearing problems arise.
- Nausea and vomiting are also signs of vascular disorders.
- The skin takes on an unnatural color - the face and hands may periodically turn pale or red.
- There are problems with coordination of movements, the patient is poorly oriented in space, and performance decreases.
- Severe cerebral circulatory disorders often lead to the development of strokes, and this applies not only to older patients, but also to young people.
The occurrence of serious consequences for the body with a herniated intervertebral disc in the neck increases as it protrudes into the spinal column. The longer the disease lasts without appropriate therapy, the greater the likelihood of disruption of the entire functioning of the body. Therefore, timely diagnosis and therapy allow the patient to return to normal life in a minimum period of time, and preventive measures will not lead to re-formation of the hernia.
In addition to protrusion, it is even possible to separate part of the disc - sequestration.
Causes
A healthy person does not experience discomfort or pain when bending or turning the neck. Degenerative processes reduce the level of nutrition and depreciation of the disc.
The reasons for the development of this pathology are:
- spinal injuries;
- physical inactivity;
- incorrect posture;
- osteochondrosis.
People with a genetic predisposition to hernia are susceptible to accelerated development of pathological changes. The increase in the rate of degeneration processes is also influenced by age-related changes, the presence of other congenital defects and unfavorable working conditions.
Types and stages
Discs may be in a state of preherniation or true prolapse. There are several stages of the disease, each of which has characteristic features:
- first – the intervertebral disc is intact, the size of the protrusion does not exceed 0.2 cm;
- second – there is damage to the fibrous ring, the degree of protrusion exceeds 0.2 cm and can reach 0.4 cm;
- third - the ring ruptures and the disc is severely displaced up to 0.6 cm;
- the fourth is a critical degree of damage, threatening the development of sequestration. The size of the prolapse at this stage reaches 0.8 cm.
Sequestration is a complicated form of hernia, which consists of the final separation of a deformed fragment of cartilage from the disc and its entry into the spinal space.
The danger of this condition is the possibility of rapid development of serious irreversible damage to nerve endings and their death. There is a high risk of paralysis of the torso below the affected area, partial or complete paresis of the arms, dysfunction of the reproductive system and genitourinary organs.
Symptoms
The ability to recognize and identify the symptoms of a herniated cervical spine allows you to focus on the problem in the early stages of its development and immediately consult a doctor. In this case, the treatment process is greatly facilitated and less harm is caused to the body.
In addition, by understanding the symptoms, you will be able to fully describe your feelings to the doctor, which will help in making a diagnosis and determining further treatment. Symptoms depend on a number of factors, for example, the size of the cervical hernia, its location, etc.
To begin with, it is worth familiarizing yourself with the general symptoms at the early stage of the disease:
- Initially mild, but over time severe discomfort in the neck, which is characterized by muscle strain, pulling sensations, periodic mild pain that disappears after rest.
- One of the first signs, which is also considered very alarming, is the inability to completely lower the head, touching the chin to the chest. In this case, attempts are accompanied by pulling sensations in the neck.
- Turning the head to the side is often accompanied by a characteristic crunching sound, which can also be accompanied by uncomfortable sensations.
- Headaches with a hernia can also appear in the initial stages, but they are not too frequent, although a certain systematicity can be observed (headaches 2-3 times a week).
The four points described relate directly to the initial symptoms, but one more can be identified - a common one, which is present in all types of hernia, when the pathology progresses and the formation grows.
We are talking about pain, it is they that always accompany this disease of the spine and as the disease progresses they only intensify, when the hernia increases, it becomes impossible to tolerate them. Initially, with a cervical hernia, the pain syndrome is located only between specific segments of the spine, which corresponds to the localization of the formation. But as the hernia grows, the painful sensations intensify, radiating to the shoulder and upper limbs, the scapular area of the back, and intensify with head movements. At the same time, tinnitus, dizziness, etc. are noted.
The pain is characterized by its constancy, they can only be relieved with painkillers, slight relief is noted in a relaxed state if the patient takes an even horizontal position. The nature of the pain is dull, pulling, aching, but in the later stages of the disease sudden sharp pain occurs and lumbago is noted.
This is what the general symptoms look like, but to fully understand the development of the pathological process, it is necessary to highlight the clinical signs of a cervical hernia, when it is localized between specific vertebrae.
Before we begin, it is worth recalling that the cervical spine consists of 7 vertebrae, which in medicine are designated by the letter C. Thus, a hernia between the 2nd and 3rd vertebrae is marked C2-C3, etc.
C1 vertebra
We are talking about a formation between the first and second vertebrae labeled C1-C2. The clinical picture in this case is as follows:
- The pain syndrome is localized in the occipital part and covers the back half of the head. The pain is characterized by systematic manifestations, which become more frequent and intense as the formation grows.
- Frequent sudden dizziness, as well as tinnitus (low-frequency squeaking, ringing, rustling, feeling of fullness).
- Patients have disturbed sleep, which manifests itself in the inability to fall asleep (insomnia) or in restless sleep during the night.
- People with a hernia type C1-C2 suffer from nervous disorders, neuroses, and frequent mood swings for no significant reason.
- There is a general lack of coordination of movements.
C2 and C3 vertebrae
A herniation of the cervical spine between the C2-C3 vertebrae affects the nerve endings and vessels relating to the eyes, tongue, and frontal lobe. For these reasons, in addition to pain, the symptoms are as follows:
- Disturbances of nervous activity, expressed in nervousness, panic attacks, susceptibility to depressive states.
- Visual disturbances, the appearance of goosebumps, black spots, blurred vision.
- Taste sensations are disturbed; in some cases, patients not only poorly recognize tastes, but also confuse them.
- As before, the growth of the hernia is accompanied by more frequent headaches with increasing intensity.
C3 and C4 vertebrae
Intervertebral hernia of the cervical spinal column C3-C4 - in this case, the nerve branches that carry out the conduction of nerve impulses to the teeth, cheeks, outer ear and facial bones are infringed. The clinical picture is as follows:
- Hearing impairment.
- Problems with smell.
- Absence or disturbance of taste.
- Signs of trigeminal neuralgia.
C4 and C5 vertebrae
The hernia affects areas of the nerves responsible for the innervation of the oral cavity and nose; clinical signs are as follows:
- Development of pathologies associated with the ears and nose, deterioration of smell and hearing.
- Frequent headaches.
- Impaired functioning of the facial muscles, partial unilateral paralysis is possible.
- The innervation of the shoulder girdle and forelimbs is disrupted, which manifests itself in the inability to raise or spread the arms to the sides, and it is difficult for the patient to move his shoulders.
- In addition to pain radiating to the arms, for example, the forearm area, as well as the appearance of numbness in the arms, there is a sensation of pressure in the neck area.
C5 and C6 vertebrae
A hernia of the C5-C6 cervical spine most likely aggravates the innervation of the vocal cords, pharynx and pharynx, which is accompanied by the following symptoms:
- A hernia between the 5th and 6th vertebrae leads to hoarseness.
- Feeling of a lump in the throat.
- Susceptibility to eye and throat diseases.
- When the size of the C5-C6 hernia is 3 mm, problems with the hands begin. Control is partially lost, there are early signs of progressive paralysis, expressed in a feeling of numbness, tremor, tingling, burning of the skin of the forearm.
- There is muscle weakness, mainly in the biceps.
- The pain covers the upper extremities, it spreads throughout the arm and reaches the thumb.
C7 vertebra
A hernia between the C6-C7 vertebrae of the cervical spine aggravates the innervation of the shoulder girdle, neck muscles, and tonsils. The clinical picture in this case is as follows:
- Chronic cough, hoarse and hoarse voice.
- Patients suffer from shortness of breath even with minor exertion.
- The pain spreads to the shoulder girdle and arms, reaching the fingers. There are also previous symptoms of impaired coordination of hand movements, numbness, tingling, etc., up to and including paralysis.
Diagnostics
If you experience neck pain radiating to the shoulder girdle, head and arms, you should consult a neurologist or vertebrologist. The doctor will conduct an examination and, if there is a suspicion of a hernia of the neck of the 5th and 6th vertebrae, prescribe instrumental diagnostic methods:
- CT;
- MRI;
- X-ray;
- electromyography.
The most complete information about the condition of the cartilaginous bodies of the spine is provided by MRI. The method allows you to obtain layer-by-layer images of tissue and accurately assess the location of the protrusion and its size.
Peculiarities
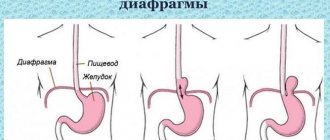
The neck is the upper part of the spinal column, which is characterized by high mobility, allowing free and varied movements of the head. It consists of 7 vertebrae with transverse processes, on both sides of which blood vessels and spinal nerves pass. The two upper vertebrae of the neck differ from the others in their anatomical structure. They provide the connection between the spine and the skull. Between the paired adjacent vertebrae there are intervertebral discs consisting of the fibrous ring and the nucleus pulposus.
A hernia is formed mainly between the 5th and 6th discs, as well as the 6th and 7th cervical vertebrae. Much less commonly, the disease affects the space between the 4th and 5th vertebrae of the neck. Pathology almost never occurs between the 7th cervical and 1st thoracic vertebrae.
The occurrence of prolapse provokes rupture of the ring and protrusion of the disc. Compression of the spinal roots is manifested by a sharp pain syndrome. Due to the close location of the spinal arteries, a hernia can cause neurological disorders and vascular pathologies.
The size of the vertebrae of the neck is much smaller than that of the thoracic and dorsal. However, the anatomical features of this area are such that even the slightest protrusion can provoke the appearance of a hernia.