Pseudomonas aeruginosa is a particularly pathogenic bacterium that can be easily acquired during hospital treatment; its transmission in everyday life is possible, but this happens less often. Most often, the microbe “lives” in intensive care units, because they have a large amount of equipment and instruments that are used repeatedly. At the same time, he is not sensitive to many antiseptics, and some, for example, rivanol, are used as food. Bacteria are also credited with a kind of “collective intelligence.”
The point of the story about Pseudomonas aeruginosa and the diseases it causes is not to treat yourself or not to go to the hospital (after all, its concentration is greater within hospital walls than on the street or at home). The point is to do everything possible so that the disease does not require intensive care (there are people who insist on treatment in the intensive care unit). This concept includes a routine examination, contacting a doctor if any incomprehensible symptoms appear, as well as proper nutrition, sufficient activity and maintaining, without fanaticism, cleanliness of the skin.
General information
Pseudomonas infection is a group of various infectious diseases, the etiological factor of which is opportunistic microorganisms of the genus Pseudomonas (in Latin - Pseudomonas).
Microorganisms of the genus Pseudomonas are free-living bacteria and are extremely common in the environment, including water and soil, and are capable of using almost all natural organic compounds as an energy source. The presence of a wide range of enzymes and plasmids in bacteria of this genus ensures high variability and the ability to quickly adapt to changing environmental conditions and withstand powerful and prolonged anthropogenic pressure. Bacteria of the genus Pseudomonas are capable of multiplying at a high rate, have a high growth rate and a wide spectrum of activity, which makes them able to colonize almost any niche and adapt to the action of new chemical compounds.
These adaptations can be expressed in the transformation of the morphology and genotype of the microorganism. May be a component of the normal microflora of the skin, especially around the ears, in the groin/axillary area and mucous membranes (for example, nose, throat). Pseudomonas aeruginosa is also often found in the ear and sputum.
Currently, pseudomonads are widely used in practice (for extracting residual oil from wells, producing antibiotics, combating environmental pollution, as models for theoretical research, etc.). The most important in medical practice is Pseudomonas aeruginosa, which is one of the main causative agents of systemic/local purulent-inflammatory processes (bacteremia, septicemia), especially in patients in hospital. In addition to Pseudomonas aeruginosis, some other types of pseudomonas (P. pseudomallei, P. Cepacia, P. Mallei, P. fluorescens, etc.) can cause infectious diseases, but their share in morbidity is significantly lower.
The spectrum of infectious diseases caused by pseudomonas aeruginosa varies from external minor infections ( soft tissue infection , pseudomonas folliculitis , otitis externa , etc.) to severe and life-threatening diseases ( pneumonia , bacteremia , infections of bones and joints, endocarditis , etc.). Infections caused by Pseudomonas aeruginosa are more common and more severe among individuals:
- Those in a hospital setting.
- Weakened and elderly patients and in patients with severe immunodeficiency .
- Patients with diabetes / cystic fibrosis / cystic fibrosis .
- Taking immunosuppressive drugs.
- In children with congenital anomalies and premature babies.
Pseudomonas aeruginosa is one of the most common causes of nosocomial (nosocomial) infections, accounting for up to 20% of cases. It accounts for almost 25% of purulent pathologies in surgical patients and about 35% of all infections of the urinary system. Pseudomonas aeruginosa is also the infectious agent of primary bacteremia .
Diseases caused by Pseudomonas aeruginosis
Pseudomonas aeruginosa causes various diseases, depending on the location where the infection occurs. According to statistics, it is the causative agent of:
- about 35% of all diseases of the urinary system;
- almost a quarter of all purulent surgical pathologies;
- 5-10% of all community-acquired pneumonia;
- and 10-35% of those inflammations of the lung tissue that developed on the third day or later after admission to the hospital.
Getting into any organism, Pseudomonas aeruginosa goes through three stages of development:
- It attaches to the tissue through which it entered, and then begins to multiply there. This is how the primary focus of infection is formed.
- Spreads from the primary focus to deeper tissues.
- Absorption of the bacterium with all its enzymes and toxins into the blood, and then the pseudomonad spreads through the bloodstream to other organs. Thus, the appearance of soft tissue phlegmon can at that stage lead to the formation of pneumonia, pyelonephritis and even damage to the brain substance.
Based on symptoms alone, it is impossible to say that the causative agent of the disease is Pseudomonas aeruginosa, since it causes the same otitis, pneumonia, gastroenteritis as other bacteria (Klebsiella, Staphylococcus). You can suspect this particular microbe either by the fact that the person was recently treated in a hospital, or by the ineffectiveness of initial antibiotic therapy (when a “regular” antibiotic was prescribed, but the temperature continues to persist and the blood count does not improve).
Pathogenesis
The pathogenic effect of Pseudomonas aeruginosa is due to the ability of the bacterium to invade and persist for a long time in various tissues, to have a cytotoxic effect and to stimulate a generalized inflammatory response. Factors directly influencing the formation of local/systemic inflammation include exotoxin S , lipopolysaccharide , nitrate reductase , flagellin , phospholipase C , pyocyanin , most of which initiate the secretion of the leading proinflammatory mediator - TNF (tumor necrosis factor).
P. aeruginosa is characterized by the presence of a type 3 excretion system, which ensures the removal of exoenzymes from the internal environment of the bacterial cell and their subsequent translocation directly to targets inside the eukaryotic cell. Such substances in Pseudomonas aeruginosa are exotoxins (ExoT, ExoS, ExoU, ExoY). Under their influence, DNA synthesis is inhibited, cell shape changes, apoptosis is stimulated, and the cell loses its ability for local adhesion.
Different strains of the P. aeruginosa population are heterogeneous in terms of their ability to synthesize/secrete various toxicity factors, due to the individual interaction of macro- and microorganisms, the influence of environmental conditions and bacterial population density.
The most important mechanism for the expression of virulence factors is the phenomenon of cooperative sensitivity, which consists in changing the physiological functions of bacteria during growth/decrease in their numbers with the formation of a response of a new quality. Under the control of this system is the formation of biofilm through cell aggregation and the release of polysaccharides into the external environment and the synthesis of all exotoxins .
Biofilm formation occurs due to the ordered/coordinated behavior of bacteria (quorum sensing), implemented by signaling through chemical compounds, which provides the P. aeruginosa population with resistance to the effects of certain disinfectants and antimicrobials, leading to outbreaks of nosocomial infections.
P. aeruginosa is capable of specific adhesion due to molecules in the composition of plasma proteins, which are adhesins for bacteria and nonspecific adhesion on various implanted devices (endotracheal tubes, catheters, etc.). Distribution through extracellular spaces is ensured by secreted proteins with high enzymatic activity: lipase, elastase, protease, which underlies the high risk of developing bacteremia in almost any localization of the primary infectious focus.
What is this in simple words?
In simple words, Pseudomonas aeruginosa is a particularly pathogenic bacterium that can be easily acquired during hospital treatment; its transmission in everyday life is possible, but this happens less often. Most often, the microbe “lives” in intensive care units, because they have a large amount of equipment and instruments that are used repeatedly. At the same time, he is not sensitive to many antiseptics, and some, for example, rivanol, are used as food. Bacteria are also credited with a kind of “collective intelligence.”
The point of the story about Pseudomonas aeruginosa and the diseases it causes is not to treat yourself or not to go to the hospital (after all, its concentration is greater within hospital walls than on the street or at home). The point is to do everything possible so that the disease does not require intensive care (there are people who insist on treatment in the intensive care unit). This concept includes a routine examination, contacting a doctor if any incomprehensible symptoms appear, as well as proper nutrition, sufficient activity and maintaining, without fanaticism, cleanliness of the skin.
A number of features allow Pseudomonas aeruginosa to lead in the frequency of nosocomial infections:
- Widespread - the bacterium belongs to the opportunistic microflora and is normally found on the skin, mucous membranes, and gastrointestinal tract of a third of healthy people;
- High variability - the rod quickly becomes resistant to disinfectants and antibiotics;
- Stability in the external environment - the microorganism tolerates the lack of nutrients, temperature changes, and exposure to ultraviolet rays for a long time; a wide range of pathogenic substances - Pseudomonas aeruginosa contains endotoxin in its structures and additionally produces exotoxins, which inhibit the growth of competitive microflora and the activity of immune cells;
- The ability for nonspecific adhesion - the bacterium has the property of attaching to non-biological objects: catheters, tubes of a ventilator, endoscopes, surgical instruments;
- Formation of biofilms - a colony of Pseudomonas aeruginosa forms a continuous layer covered with a biopolymer, which reliably protects them from the effects of adverse environmental factors.
Classification
The classification of the Pseudomonadaceae family is based on the rRNA homology feature, on the basis of which 5 groups are distinguished:
- Group I (genus Pseudomonas) - Pseudomonas aeruginosa, Pseudomonas putida, Pseudomonas alcaligenes, Pseudomonas stutzeri, Pseudomonas fluorescens, Pseudomonas mendocina, Pseudomonas pseudoalcaligenes, etc.
- Group II (genus Burkholderia) - Burkholderia mallei Burkholderia pseudomallei, Burkholderia cepacia, etc.
- Group III (genus Comamonas) - Comamonas terrigena, Comamonas acidovorans, etc.
- Group IV (genus Brevundimonas) - Brevundimonas diminuta, Brevundimonas vesicularis.
- Group V (genus Stenotrophomonas) - Stenotrophomonas maltophilia.
Thus, Pseudomonas aeruginosa belongs to the kingdom - Bacteria, family Pseudomonadaceae, genus - Pseudomonas. Previously, some other representatives were also included in the genus Pseudomonas, but as of today they are classified as an independent genus of proteobacteria Brevundimonas, which, despite their widespread presence in the environment, are isolated extremely rarely from clinical samples, for example, brevundimonas pseudomonas naejangsanesis.
Causes
The causative agent of Pseudomonas aeruginosa infection is in most cases Pseudomonas aeruginosa, which belongs to the opportunistic microflora of the body, capable of causing an infectious disease only if there is an insufficient response or absence of an adequate response of the immune system.
Microbiology of Pseudomonas
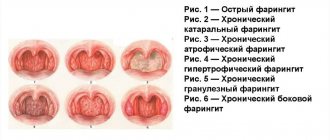
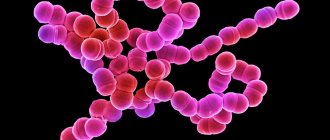
Microorganisms of the genus Pseudomonas (in Latin - Pseudomonas) belong to the group of gram-negative non-fermenting bacilli. They are straight single/pair rods or arranged in the form of chains of rods (Fig. below), 1.0-1.7 × 0.6 microns in size. They do not form capsules, have a flagellum and pili (outgrowths) that provide mobility. They can produce, under certain conditions, extracellular capsule-like mucus of a polysaccharide nature. Cultures produce characteristic pigments: which include compounds that color the environment yellow-green, blue-green and brown.
They are resistant to drying, are well preserved in a humid environment, and are destroyed by boiling, autoclaving, or exposure to chlorine-containing disinfectants and 3% hydrogen peroxide .
Epidemiology
The source of infection is patients and bacteria carriers, the primary localization in the human body is the skin and intestines. How is Pseudomonas aeruginosa transmitted? Outside of hospital settings, the bacillus is transmitted mainly by airborne droplets and contact. In case of hospital infection, the main route of infection is contact: it is transmitted through the hands of medical personnel, unsterile instruments and patient care items.
Due to the excellent ability of Pseudomonas aeruginosa to exist in a humid environment, it contaminates a wide variety of ecological niches - solutions, including some disinfectants, for example, Rivanol , Furacilin , as well as medical equipment, instruments, hospital items (especially in places where liquid accumulates - taps , sinks, respirators, dishes, humidifiers, etc.). Transmission factors are often epidural, urinary and vascular catheters, Esmarch circles, infusion solutions, dressings, infant formula, food, dishes, etc. A consequence of the significant spread of Pseudomonas aeruginosa in the system of medical institutions is a significant colonization of the skin/mucosal surfaces of patients.
The ecological system of the hospital environment is not stationary. We can say that continuous phase transformations occur in it, contributing to the formation of epidemic variants of Pseudomonas aeruginosa and the consistent change of the epidemic and inter-epidemic periods. At the same time, epidemic variants have such virulence factors, metabolic potential and physiological properties that ensure the existence of the microorganism in two forms: in the form of a mobile form that provides them with movement to colonize a new niche or habitat and a fixed biofilm that protects from many unfavorable environmental factors and allowing them to survive in a wide variety of conditions.
Thus, with standard disinfection, the survival time of Pseudomonas aeruginosa in the intensive care unit environment exceeded 3 months. Pseudomonas aeruginosa is one of the pathogens with high epidemic potential and, over a short period (6-7 days), is capable of forming hospital strains and causing nosocomial outbreaks through existing transmission routes.
In addition to exogenous infection, there is also the possibility of endogenous infection, which is caused by a person’s own, normal microflora. The infectious process develops when the immune system is weak or in cases of violation of antimicrobial barriers in the form of infection of wound surfaces with intestinal contents, etc. Susceptibility to the development of Pseudomonas aeruginosa infection is high. Does an adult suffer from Pseudomonas aeruginosa? Yes, Pseudomonas aeruginosa infection occurs in both adults and children, regardless of age group.
"Weapons" of bacteria
Pseudomonas aeruginosa “strikes” the human body due to the fact that:
- can move using flagella;
- produces a toxin as a product of its own vital activity, that is, until its death;
- produces substances that: “burst” red blood cells, damage liver cells, kill leukocytes - immune cells that are designed to fight any infection;
- synthesizes substances that kill other “competitor” bacteria at the site of entry;
- “stick” to surfaces and to each other, becoming covered with a common “biofilm” that is insensitive to antibiotics, antiseptics and disinfectants. Thus, pseudomonas colonies live on catheters, endotracheal tubes, respiratory and hemodialysis equipment;
- there are enzymes that allow movement through the intercellular space;
- synthesize phospholipase, which destroys the main part of the surfactant - a substance due to which the lungs do not “stick together” and can breathe;
- produces enzymes that break down proteins, so the bacterium causes tissue death in the place where it accumulates in sufficient quantities.
Another feature of pseudomonas is that it has many factors that allow the bacteria not to be destroyed by antibiotics. This:
- enzymes that break down the main bactericidal substance of antibiotics such as penicillin, ceftriaxone, cephalexin and others;
- defects in proteins that close the pores - “gaps” in the cell wall of microbes;
- the ability of a microbe to remove a drug from its cell.
Symptoms of Pseudomonas aeruginosa
The symptoms of Pseudomonas aeruginosa infection are extremely diverse, which is due to the polytropic nature of Pseudomonas aeruginosa, the various ways it enters the body, its predominant localization in the body and the individual characteristics of the patient. The vast majority of cases of clinical manifestations of Pseudomonas aeruginosa relate to nosocomial infections. The following clinical manifestations are distinguished:
Local skin/subcutaneous tissue infection (wound infections, pyoderma, dermatitis)
Most often, infectious inflammation occurs at the site of burns, trauma, cuts and surgical sutures, bedsores, varicose ulcers, etc., especially after antibacterial therapy. A characteristic blue-green color appears on the wound surface, and the scab on the wound surface acquires a dark brown, purple or black color.
Infection on the nails
Under the scab, tissue swelling and hemorrhages , necrotic tissue destruction occurs. The inflammatory process quickly spreads to healthy areas of the skin and soft tissue, as evidenced by pronounced redness. The process often ends with the development of an abscess or gangrene .
The general condition of the patient suffers. One of the common manifestations of Pseudomonas aeruginosa infection on the skin is folliculitis - pustular rashes on the skin, in the center of which there is a hair. May be accompanied by severe itching. Pseudomonas aeruginosa infection can also manifest itself as dermatitis and pyoderma .
Eye infections
It can manifest as purulent conjunctivitis , keratitis and even panophthalmitis (damage to the eyeball) and subsequent destruction of the eyeball. Patients complain of a sensation of a foreign body, pain in the eye and purulent discharge, blurred vision. The most common cause is eye trauma, burns or contamination of contact optical lenses. Initially, a small ulcer appears in the center of the cornea, which quickly expands and covers the sclera. The general condition of the patient does not suffer. After eye surgery and penetrating trauma, purulent endophthalmitis .
Infections of the ear, paranasal/mastoid sinuses
Pseudomonas aeruginosa in the ear most often manifests itself as suppurative otitis externa , manifested by a purulent/sero-bloody discharge from the external auditory canal. Less commonly, the development of otitis media and mastoiditis . When localized on the nasal mucosa, Pseudomonas aeruginosa can cause chronic ongoing rhinitis and inflammation of the paranasal sinuses ( frontal sinusitis / sinusitis ), accompanied by their characteristic symptoms.
Gastrointestinal tract infections
Pseudomonas aeruginosa infection can affect any part of the gastrointestinal tract with varying degrees of inflammatory changes from mild catarrhal to ulcerative necrotic inflammation with perforation of the intestinal wall and the occurrence of bleeding. More often it occurs in the form of food poisoning or gastroenterocolitis . Characterized by an acute onset, vomiting and foul-smelling greenish loose stool mixed with mucus (5-6 times per day), epigastric pain, high fever, rumbling and bloating. The duration of the disease is 2-5 days.
Urinary tract infection
Most often, Pseudomonas aeruginosa enters the urinary tract by an ascending route, but it can also be carried into the urinary tract by a hematogenous route. Pseudomonas aeruginosa in the urinary organs causes the development of urethritis (inflammation of the urinary canal), cystitis (bladder) and pyelonephritis .
The clinical symptoms of these pseudomonas inflammation correspond to the clinical manifestations of these diseases caused by other microorganisms. Less common are ulcers on the mucous membrane of the bladder, renal pelvis or ureter, characteristic of Pseudomonas aeruginosa infection. A characteristic feature is a protracted/chronic course with frequent exacerbations and polyresistance to antibacterial drugs.
Pseudomonas infection in the lungs
Pseudomonas aeruginosa infection in the respiratory system most often develops in patients with diseases of the bronchopulmonary system: cystic fibrosis , bronchitis , bronchiectasis , as well as in patients in intensive care units and on artificial respiration devices. The symptoms correspond to the appearance of typical pneumonia, but it is characterized by a protracted course, the occurrence of destructive processes in the lungs (disintegration of lung tissue), a weak effect or no effect from the antibacterial therapy.
Damage to the nervous system
Its manifestation is the development of meningitis , which often occurs secondary to sepsis through the introduction of infection from other foci. Less common is primary meningitis , which occurs when the pathogen is introduced into the subarachnoid space during spinal anesthesia , lumbar puncture , medical procedures or head injuries.
Endocarditis
It occurs relatively rarely, mainly when the pathogen is introduced during open-heart surgery through infected suture material. The consequences of endocarditis of this etiology can be metastatic abscesses in the bones ( osteomyelitis ), joints, adrenal glands and lungs.
Bacteremia caused by Pseudomonas aeruginosa
It develops as a result of the generalization of a local infectious process - the clinical forms of which are festering wounds, pneumonia , and urinary tract infection. It is also often the result of a device implanted into the bloodstream that is contaminated with a pathogen. The course of septicemia is extremely severe, accompanied in 35-70% of cases by the death of the patient.
Who is at risk for infection?
The pathogen is especially dangerous for:
- elderly over 60 years of age;
- children in the first three months of life;
- weakened people;
- patients with cystic fibrosis;
- requiring hemodialysis;
- patients with diabetes mellitus;
- HIV-infected;
- patients with leukemia;
- those who received burns;
- people who have undergone organ transplantation;
- receiving hormonal medications for a long time (for example, for the treatment of rheumatoid arthritis, lupus erythematosus or other systemic diseases);
- having malformations of the genitourinary system;
- suffering from chronic bronchitis;
- forced to stay in hospital for a long time.
It is also possible to predict which disease of pseudomonas etiology will develop - by age, primary pathology or manipulation performed
| Risk factor | What may develop |
| Often have to undergo intravenous procedures | Endocarditis. Osteomyelitis. |
| A man has leukemia | Abscess in the gluteal muscle. Sepsis |
| Oncological diseases | Increased risk of Pseudomonas pneumonia |
| Burns | Inflammation of the subcutaneous tissue (cellulitis), as well as sepsis, may develop |
| Surgeries were performed on the organs of the central nervous system | Meningitis |
| A tracheostomy was performed | Pseudomonas pneumonia may develop |
| A corneal ulcer appeared | Inflammation of all membranes of the eye may develop |
| Vascular catheterization was performed | Thrombophlebitis may develop |
| Bladder catheterization was required | Infections of the genitourinary system |
| Newborns | Pseudomonas meningitis, inflammatory bowel disease |
Patients of such departments are most often ill:
- intensive care;
- burn;
- surgical, in which operations on the abdominal cavity are performed, and abscesses and carbuncles are opened;
- cardiac surgery.
Tests and diagnostics
The diagnosis is made based on the results of laboratory examination.
Bacteriological seeding of material on nutrient media (nasopharyngeal mucus, sputum, urine, blood, feces, discharge from wounds, etc.) followed by microscopy (Fig. below). If necessary, instrumental examinations - lumbar puncture, chest x-ray, ultrasound, echocardiography, bronchoscopy, CT and magnetic resonance imaging.
P. aeruginosa colonies
Pseudomonas aeruginosa during bacterioscopy
Pseudomonas aeruginosa in children
Symptoms of Pseudomonas aeruginosa in children, as well as in adult patients, are determined by the localization of the infectious process. It should be noted that if Pseudomonas aeruginosa is detected in children, Komarovsky considers this not a reason to panic, since it can also occur in healthy children. It is important that its release is not accompanied by specific symptoms of the disease. Most often in children, especially young children, the gastrointestinal tract is affected with the development of symptoms of enterocolitis and the respiratory tract with the development of pneumonia. Less common are eye damage, otitis , meningitis , osteomyelitis , pyelonephritis and sepsis .
Damage to the gastrointestinal tract
The disease begins acutely with loose stools, abdominal pain, and rumbling in the intestines. The frequency of bowel movements varies from 5 to 15 times, and the consistency is from greenish to yellowish with an admixture of mucus and pus, less often streaks of blood. The temperature reaction and toxicosis in the child increases gradually over the first 2-3 days. Some children with Pseudomonas aeruginosa enterocolitis develop toxicosis with exicosis , and the overwhelming majority develop profound disturbances of the intestinal microbiocenosis due to a significant decrease in the presence of E. coli and bifidobacteria .
In older children, when infected with food, food poisoning , which is characterized by a short incubation period, nausea, pain in the epigastric region, and vomiting of eaten food. The stool is liquid/mushy with a small amount of mucus and a frequency of 3-8 times a day. The severity of the course is determined by the phenomena of general toxicosis . Pseudomonas aeruginosa infection in children is more often acute, and less often it can be protracted.
Pseudomonas aeruginosa infection occurs especially often in neonatal units in the form of outbreaks. Premature babies are especially susceptible to infection, and they become infected through medical personnel. The gastrointestinal tract is predominantly affected with the development of clinical symptoms of enterocolitis with a hemorrhagic component, which occurs in a severe form. There is rapid dehydration of the child and severe loss of body weight. In addition to the digestive tract, the ears, skin, umbilical wound, and eyes can be involved in the pathological process. Treatment of Pseudomonas aeruginosa in children is not fundamentally different from the treatment of adult patients.
Additional treatment
This is the treatment of the disease against which the Pseudomonas aeruginosa infection developed (cystic fibrosis, immunodeficiency states), bacteriophage and the introduction of anti-pseudomonas antibodies.
Bacteriophage
Pseudomonas aeruginosa can be destroyed not only by antibiotics, but also by a specially created non-infectious virus - an antipseudomonas bacteriophage. Before prescribing it, you must first determine your sensitivity to it.
The bacteriophage is effective when administered locally along with antibiotics. So, it can be delivered to the intestines orally or as an enema, and to the vagina and bladder through a thin catheter. It can be injected into the pleural cavity, renal pelvis and sinuses, having previously installed drainage there.
The bacteriophage can also be used for children, even newborns and premature babies.
Learn more about what bacteriophages are, plus a list of drugs.
Autovaccine
Its name is Pseudovac, which is prepared individually, based on the strain isolated from the patient.
Antipseudomonas donor plasma
This is the liquid part of the blood, which can be obtained if the donor is given doses of Pseudomonas aeruginosa that are not dangerous to his health. Then his body begins to synthesize protection against the bacteria - antibodies. Most of them are contained in plasma, which, taking into account the blood type, is administered to the patient.
Prevention
Specific prevention is carried out by administering a polyvalent vaccine to persons with immune deficiency, medical workers, patients with deep/extensive wounds, open fractures, burn patients, and elderly patients.
Nonspecific preventive measures include the prevention of immunodeficiency conditions, timely treatment of chronic infections, health promotion, and proper nutrition. Prevention of nosocomial infection is achieved by carrying out comprehensive anti-epidemic measures.
List of sources
- Smirnov V.V., Kiprianova E.A. Bacteria of the genus Pseudomonas. Kyiv: Naukova Dumka, 1990. 264 p.
- Ivanov D.V. Distribution and mechanisms of resistance of microorganisms of Pseudomonas bacterial strains // Pharmateka / Ivanov D.V., Egorov A.M. - 2007. No. 8/9. — p.159-168.
- Beloborodov V.B. The problem of antibacterial therapy for infections in intensive care units from the perspective of evidence-based medicine. // Consilium medicum. – 2002. – vol.4. – No. 1. "Infections in the hospital."
- Strachunsky, L.S., Reshedko, G.K., Stetsyuk, O.U., Andreeva, A.S., Shchebnikov, A.G. Comparative activity of antipseudomonas antibiotics against nosocomial strains of Pseudomonas aeruginosa isolated in intensive care units of Russia // Antibiotics and Chemotherapy, 2003. - No. 5. – p.35-46/
- Shaginyan, I.A., Chernukha, M.Yu. Non-fermenting gram-negative bacteria in the etiology of nosocomial infections: clinical, microbiological and epidemiological features // Klin. microbiol. antimicrobial chemotherapy – 2005. – T.7. - No. 3. - With. 271-285.