5 / 5 ( 1 voice )
The article talks about a disease in which the heart muscle is replaced by connective tissue. This condition is called cardiosclerosis. The causes and symptoms of the pathology, treatment and diagnostic measures are described.
Cardiosclerosis is the replacement of functionally active myocardium with connective tissue
Atherosclerotic cardiosclerosis is the process of replacement of the myocardium with connective tissue. The disease manifests itself as angina attacks and heart rhythm disturbances. The diagnosis is made on the basis of laboratory and instrumental methods, treatment is carried out conservatively.
About the disease
The cause of this disease is atherosclerosis - a chronic process in the vascular wall of medium- and large-caliber arterioles, which is based on the accumulation of cholesterol, the growth of scar tissue and the narrowing of the lumen of the vessel.
In the international classification of diseases (ICD 10), cardiosclerosis is coded in the group of coronary heart disease (CHD):
- I25 - chronic ischemic heart disease:
- 0 - atherosclerotic cardiovascular disease.
At the appointment, I diagnose this condition in patients with a long course of coronary heart disease and its consequences (angina pectoris, myocardial infarction, rhythm disturbances, circulatory failure).
Diagnostics
Pathology can be determined through an objective examination of the patient; the diagnosis is confirmed by the results of instrumental studies. An objective examination reveals characteristic symptoms of the disease.
Instrumental diagnostics include:
- electrocardiography – detects rhythm and conduction disturbances of the heart;
- ultrasound examination – detects areas of the myocardium with impaired functional activity;
- Vascular ultrasound, coronary angiography - reveal the location of atherosclerotic plaques.
Laboratory diagnostics determines increased cholesterol levels in the blood.
Ultrasound reveals inactive areas of the myocardium
Causes
Today it has been established that atherosclerotic cardiosclerosis is a disease caused by a combination of many factors. Some of them can be influenced by one or another therapeutic measures. A favorable basis for cholesterol deposition is the presence of damage to the internal lining of the vessel (intima).
Risks of developing atherosclerotic cardiosclerosis:
- Unmodifiable (unchangeable):
- genetic predisposition (hereditary dyslipidemia);
- age (men over 40, women over 50);
- male (estrogens produced during the menstrual cycle protect blood vessels from becoming saturated with cholesterol).
- Modifiable (changeable):
- dyslipidemia caused by poor nutrition;
- arterial hypertension;
- smoking, alcohol;
- overweight, metabolic syndrome;
- carbohydrate metabolism disorders (hyperglycemia, diabetes mellitus);
- tachycardia;
- sedentary lifestyle;
- chronic stress;
- hyperhomocysteinemia (an excess of this amino acid causes damage to the intima of the vessel, to which it is easier for cholesterol to attach).
The basis for the development of atherosclerotic cardiosclerosis is:
- Combined disorder of protein and fat metabolism. Previously, the main role was given to hyperdipidemia - an increased concentration of fats in the patient's serum due to their excess consumption. To date, it has been proven that an imbalance between “good” (high density - HDL) and “bad” (low and very low density - LDL, VLDL) lipoproteins plays a significant role in the deposition of cholesterol plaques.
- Hormonal imbalance. Insulin resistance, diabetes mellitus, and hypothyroidism contribute to the accumulation of cholesterol in the inner layer of cells (endothelium) of arterioles.
- Hemodynamic load. Constant high blood resistance in hypertension contributes to the rapid development of pathological processes in the vascular bed.
- Nervous factor. Constant stress, conflicts, lack of sleep, and unfavorable psycho-emotional background lead to impaired control over the metabolism of proteins and lipids and disorders of vascular tone.
- The immediate condition of the walls of blood vessels. An atherosclerotic plaque does not form on the intact intima of the coronary arteries. Therefore, the presence of age-related changes, an infectious process, and thrombosis facilitates the formation of cholesterol deposits.
The main danger of this disease is that cholesterol plaques, as they increase in size, lose their stability, ulcers form on their surface, and thrombotic masses accumulate. Ultimately, the affected vessel is completely blocked, and myocardial ischemia develops. Only after this do symptoms appear, with which the patient consults a doctor.
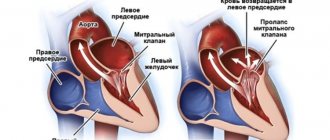
If the affected vessels are small in caliber, over time the blood-supplied areas of the heart muscle grow with connective tissue fibers that replace cardiomyocytes, gradually reducing the contractility of the myocardium. In case of blockage of a larger coronary vessel, a clinical picture of acute coronary syndrome develops with necrosis of heart tissue and replacement of the non-functioning area with a fibrous scar.
Atherosclerotic myocardial damage
The pathology is characterized by an enlargement of the heart organ and its left-sided ventricle, and the heart rhythm is disturbed.
Symptoms are in many ways similar to signs of development of cardiac organ failure.
Before cardiosclerosis begins to develop in the myocardium, the patient may suffer from cardiac pathologies and unstable angina for a long period of time.
Scarring of the myocardium occurs due to insufficient blood flow in it and the development of coronary artery sclerosis.
For this reason, many foci of necrotic changes in the heart muscle form in the myocardium.
Quite often, atherosclerotic cardiosclerosis is accompanied by the following pathologies of the heart and blood flow system:
- Arterial hypertension;
- Aortocardiosclerosis;
- Atrial fibrillation;
- Atherosclerosis of cerebral arteries.
Myocardial scarring
Typical symptoms
Atherosclerotic cardiosclerosis does not have significant symptoms as long as the compensatory capabilities of the blood flow maintain oxygen delivery at the proper level to the area supplied by the affected vessel. A bright clinic is present in the case of critical narrowing of the lumen of the arteriole.
In some areas of the myocardium, over a long period of cholesterol accumulation, new bypass blood supply pathways are formed, or the plaque itself grows with its apex towards the outer wall of the vessel, while the lumen remains unchanged.
With this disease, general clinical signs of atherosclerosis will be present:
- xanthelasmas (subcutaneous accumulations of cholesterol, often around the eyes);
- xanthomas (wart-like deposits of cholesterol on the elbow and palmar bends, along the tendons);
- premature aging, skin aging;
- early gray hair;
- increased hair growth in the ears;
- chronic pancreatitis.
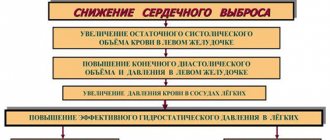
Manifestations of atherosclerotic cardiosclerosis in the heart are caused by a decrease in the mass of functioning muscle cells. All symptoms will indicate chronic heart failure:
- shortness of breath during exercise;
- orthopnea (dissatisfaction with breathing in a horizontal position);
- decreased tolerance to physical activity;
- general malaise, increased fatigue, drowsiness;
- swelling in the legs;
- cardiopalmus;
- attacks of dizziness, low mood;
- night cough.
Since atherosclerosis also affects large-caliber arterioles, the patient may additionally experience symptoms of angina pectoris: pain in the chest in response to physical and emotional stress, which can be relieved by taking Nitroglycerin and rest.
Gradual involvement of the conduction system in the pathological process can provoke heart rhythm disturbances:
- sinus or ventricular tachycardia;
- atrial fibrillation;
- atrioventricular block;
- Hiss bundle branch block.
Kinds
There are two forms of atherosclerotic cardiosclerosis:
- Diffuse small focal;
- Diffuse macrofocal.
The disease is divided into 3 types:
- Ischemic – occurs as a consequence of prolonged fasting due to lack of blood flow;
- Post-infarction - occurs at the site of tissue affected by necrosis;
- Mixed - this type is characterized by the two previous characteristics.
How to make a diagnosis
The diagnosis of “atherosclerotic cardiosclerosis” can only be established on the basis of a detailed examination of the patient for myocardial damage, blockage of coronary vessels and dyslipidemic changes in the blood serum.
The examination plan for a patient with suspected atherosclerotic coronary artery sclerosis includes:
- Laboratory blood test:
- cholesterol level, lipoprotein fractions;
- blood sugar, glycosylated hemoglobin (HBA1c);
- glucose tolerance test;
- biochemical study - creatinine, urea, ALT, AST;
- coagulogram, international normalized ratio (INR);
- hemoglobin, hematocrit;
- natriuretic peptide.
- Electrocardiography:
- standard at rest (12 leads);
- with dosed physical activity (bicycle ergometry, treadmill test);
- 24-hour Holter monitoring.
- EchoCG (ultrasound examination will accurately show the degree of myocardial hypertrophy, ejection fraction, size of the heart chambers, condition of the valve system). Recently, stress echocardiography has been introduced into practice - the study is performed in combination with physical activity on a treadmill or bicycle ergometer.
- Myocardial scintigraphy (OFCET, PET). The essence of the method is the intravenous administration of a radionulide marker (technetium99). The quality of the blood supply to the heart muscle is examined (the better it is, the more the radiopharmaceutical accumulates in the tissue; well-nourished areas have a bright glow). This scan in combination with stress tests has the greatest diagnostic information value.
- CT scan:
- CT visualization of the coronary arteries without the introduction of contrast - calcification index (cholesterol plaques, during their growth, go through the stage of calcium deposition in them, which can be seen on the scan);
- CT coronary angiography is a study of the coronary arteries using intravenous contrast.
- Invasive coronary angiography. The most accessible method for visualizing atherosclerotic lesions of the heart vessels. During the procedure, a conductor with a contrast agent is inserted through the femoral artery into the coronary artery and the location of the narrowing is determined using x-rays.
All cardiac imaging methods will help make a differential diagnosis between different types of cardiosclerosis (post-infarction, atherosclerotic, myocardial).
Classification
The main way to typify a pathological process is by the criterion of its prevalence.
Accordingly, there are two forms of cardiosclerosis of atherosclerotic origin:
- Focal. As the name suggests, this phenomenon is accompanied by the formation of scar changes in certain areas of the myocardium. There are two subtypes: small-focal and large-focal (depending on the area of the lesion).
A deviation can only be detected through instrumental methods, and this requires high professionalism of a diagnostician.
In most cases there are no symptoms either. Therefore, early detection is very difficult. At the same time, the progression of this type of disorder is extremely slow.
- Diffuse. It spreads to all hearts, the myocardium suffers everywhere at the same time. According to statistical estimates, it is this type that prevails in the development of the atherosclerotic form of cardiosclerosis.
Symptoms, however, do not always develop quickly. A silent existence for years, without a pronounced clinic, is possible.
This scenario is more dangerous due to generalized damage to the entire heart. You cannot delay treatment.
Strictly speaking, any other form of cardiosclerosis is divided in the same way, including that which develops after a myocardial infarction.
Read more about post-infarction cardiosclerosis and methods of its treatment in this article.
Clinical case
Since 2014, I have been seeing patient B., born in 1951, diagnosed with coronary artery disease.
Angina pectoris, functional class II. Atherosclerotic and post-infarction (2013) cardiosclerosis. Hypertension II degree. Heart failure IIA. The patient was overweight (BMI 30.4) and had been a smoker for 22 years. At the beginning of treatment, the patient complained of chest pain and shortness of breath that occurred when climbing to the 3rd floor, swelling of the legs in the evening, and general weakness. Blood pressure ranged from 150-160/90 mm. Hg Art., pulse - 89 beats/min.
Based on the results of additional studies, an increased amount of cholesterol, triglycerides in the blood was established, glucose was 5.8 mmol/l.
Over the course of 4 years of treatment, the patient managed to switch to a healthy diet, quit smoking, and lose weight by 22 kilograms. Regular physical activity helped increase exercise tolerance and stabilize blood pressure, and limiting salt and water made it possible to stop taking Furosemide and reduce the dosage of Enalapril.
At the moment, patient B.’s heart condition remains satisfactory. Episodes of taking Nitroglycerin no more than 1-2 times a week. It is possible to keep cholesterol levels below 4.9 mmol/l.
Development mechanism
If treatment is not started promptly, the disease will progress, leading to blockage of the arteries.
Cardiosclerotic disease is a consequence of increased levels of harmful lipids in the blood. If the condition does not normalize for a long time, fatty spots form on the walls of the aorta, which gradually increase in size, blocking the vascular lumen and disrupting blood circulation. Soon an inflammatory complication appears, coronary artery disease syndrome appears, and the risk of developing negative consequences increases.
Due to impaired blood circulation and nutrition of blood vessels and heart muscle, ischemia develops. The cells of the organ cease to function normally, after which they die, and in their place replacement tissue is formed, which does not participate in the function of contraction and transmission of bioelectric impulses. As a result, cardiosclerosis of the heart further develops.
Treatment and observation by a doctor
Atherosclerotic cardiosclerosis is a slowly progressive disease, the lack of treatment of which leads to failure of the heart muscle (areas of dead muscle cells are replaced by connective tissue).
Taking into account the characteristics of this condition, I highlight the main directions of treatment for the disease:
- whenever possible, compensation for the underlying disease;
- symptomatic correction (elimination of edema syndrome, restoration of rhythm, support of myocardial contractile function);
- lipid-lowering therapy;
- lifestyle modification;
- prevention of complications.
The treatment plan for atherosclerotic cardiosclerosis should include:
- A set of physical activity, quitting smoking and alcohol.
- Special diet: limiting the intake of sodium, water, unsaturated fats, gas-forming products, coffee, strong tea. Fractional 5-6 meals a day. Regular weighing.
- Lipid-lowering drugs (Atoris, Rosuvastatin).
- Diuretics (“Furosemide”, “Trifas”, “Veroshpiron”).
- ACE inhibitors (Enap, Lisinopril).
- Beta-blockers (“Bisoprolol”).
- Antiplatelet agents (Cardiomagnyl, Clopidogrel).
- If necessary: ytrates (“Nitroglycerin”);
- cardiac glycosides (Digoxin).
Complications of cardiosclerosis
The process of myocardial sclerosis itself does not cause pain in humans. But this can continue for a certain time, that is, until complications of the disease begin to develop. Cardiosclerosis sooner or later leads to a decrease in the functional capacity of the heart, provoking a worsening of the patient's condition. Even if it is possible to eliminate the causes that caused the pathology, the formation of connective tissue in the myocardium will lead to negative consequences.
The most common complications of cardiosclerosis are:
- chronic fatigue syndrome;
- acquired heart defects;
- cardiac aneurysm;
- thromboembolism;
- arrhythmias;
- CHF.
Most of them are not life-threatening for the patient, but can seriously complicate a person’s existence by limiting his activity. At the same time, such as thromboembolism and aneurysm (if they rupture) pose a threat, since death can occur very quickly, and patients often die before the ambulance arrives.
Prevention of deterioration of the condition
The clinical picture of coronary sclerosis worsens as cholesterol plaques and foci of fibrosis grow. All preventive measures are aimed at maximizing the preservation of myocardial contractility - preventing the progression of heart failure.
In addition to well-chosen drug therapy and control of risk factors, the patient may need:
- implantation of a cardioverter-defibrillator;
- placement of an artificial pacemaker;
- surgical methods of myocardial revascularization (stenting, coronary artery bypass grafting).
Expert advice
The success of treatment, the duration and quality of life of the patient largely depend on his motivation and ability to change his attitude towards himself.
I recommend that my patients follow several rules.
How dangerous are the pathologies in question?
Based on all of the above, many can conclude that the danger lies exclusively in the state of cardiosclerosis, and atherosclerosis of the vascular bed is a practically harmless condition. In fact, everything is not so clear.
Indeed, the condition of atherosclerosis itself (unlike cardiosclerosis) almost never leads to the death of patients. However, it is also fundamentally wrong to consider the pathology harmless and not requiring timely, comprehensive treatment. Progressive atherosclerosis of the vascular bed can provoke:
- IHD in a variety of manifestations;
- heart and kidney failure;
- cerebral ischemia, even to the point of stroke, as well as many other problems that can lead to the death of patients.
The occurrence of heart attack and stroke
That is why practicing doctors are unanimous in the opinion that the conditions of atherosclerosis and cardiosclerosis must not be ignored, both of these pathologies are important and need to be treated in a timely manner!