Mastocytosis is a disease that progresses due to the proliferation, accumulation of mast cells and their infiltration of organs and dermis. Experts identify 5 variants of the manifestation of the disease - telangiectasia, hyperpigmentation, erythrodermic lesions, nodes (both small and large). The clinical picture of the disease depends on the form of mastocytosis. Diagnosis is based on laboratory analysis. With mastocytosis, there will be an increased number of mast cells in the tissues and skin. Treatment of matocytosis is conservative. The treatment plan includes cytostatics, serotonin inhibitors, cyproheptadine hydrochloride, and histamine H2 blockers.
Among all dermatological diseases, mastocytosis in adults is considered a fairly rare pathology (1:10,000). It is diagnosed much more often in children. This may be due to the relative complexity of differential diagnosis, as a result of which the disease is either not diagnosed at all or is registered under the guise of other diseases.
…
What is mastocytosis?
Mastocytosis is a rare disease characterized by an abnormal accumulation of mast cells in the skin, bone marrow, and internal organs (liver, spleen, gastrointestinal tract, and lymph nodes).
Cases beginning in adulthood tend to be chronic and involve the bone marrow in addition to the skin, whereas in childhood the condition is often marked by cutaneous manifestations without involving the internal organs and can often resolve during puberty. In most adult patients, mastocytosis tends to be persistent and may progress to a more advanced stage in a minority of patients. Mastocytosis can be classified into a specific type depending on the symptoms and overall appearance.
Prevention
In order to prevent exacerbations of M., it is recommended to avoid intense solar insolation and overheating of the body.
Bibliography:
Geiro S. B. and Tarjemanova N. I. To the clinic of mast cell reticulosis (malignant mastocytosis), Ter. arkh., vol. 37, no. 9, p. 23, 1965, bibliogr.; Melnikova V.S. and Lopunova Zh.K. On the issue of the clinic, treatment and histochemical characteristics of the polysaccharide and protein components of mast cells in the skin of patients with mastocytosis, Vestn, dermis, i ven., No. 8, p. 27, 1977; Pototsky I. I. Skin reticulosis p. 122, Kyiv, 1972; Degos'R. Mastocytoses cutan£es, Derm.-Vener. (Buc.), v. i p. 97, 1961, bibliogr.; S agher f' a. Even-Paz Z. Mastocytosis and the mast cell, Chicago, 1967, bibliogr.; S zw ed a JA ao Systemic mast cell disease Amer. J. Med., v. 32, p. 227, 1962.
I. M. Raznatovsky.
Types of Mastocytosis
Mastocytosis may mainly affect the skin (called cutaneous mastocytosis) or other parts of the body (called systemic mastocytosis).
- Cutaneous mastocytosis: Cutaneous mastocytosis most often occurs in children. Sometimes mast cells accumulate in the skin only as a single mass (mastocytoma), usually before 6 months of age. Most often, mast cells accumulate in many areas of the skin, forming small reddish-brown spots or bumps (called urticaria pigmentosa). Urticaria pigmentosa rarely develops into systemic mastocytosis in children, but it may occur more often in adults.
- Systemic mastocytosis: Systemic mastocytosis most often occurs in adults. Typically, mast cells accumulate in the bone marrow (where blood cells are made). They often also accumulate in the skin, stomach, intestines, liver, spleen and lymph nodes. Organs can continue to function with almost no disruption. But if too many mast cells accumulate in the bone marrow, the production of blood cells is significantly reduced, and serious blood diseases such as leukemia can develop. If too many mast cells accumulate in organs, the organs begin to malfunction. The resulting problems can be life-threatening.
Clinical picture
Manifestations of mastocytosis are characterized by great diversity. In accordance with the International Classification of the 10th revision, its various forms are distinguished. In practice, mastocytosis is distinguished:
- Cutaneous.
- Systemic.
Cutaneous mastocytosis
It can take the form of:
- Urticaria pigmentosa.
- Knotty shape.
- Bullous form.
- Mastocytomas.
- Diffuse mastocytosis.
- Persistent macular telangiectasia.
Urticaria pigmentosa
It occurs at any age, but most often it affects children in the first two years of life. In most cases, occurring at an early age, the disease resolves spontaneously with recovery by puberty. However, it often develops after the age of 10 years, lasts with periodic exacerbations throughout life, and can progress and acquire the character of a systemic pathology. During the course of the disease, there are 3 stages - progress, stabilization and regression.
Progressive stage
It occurs in paroxysms with pronounced polymorphism of the rash. Attacks have varying durations. Elements of the rash look like spots, papules, vesicles, blisters. In adults, as a rule, papules, spots with excessive pigmentation, or a combination of both immediately appear. The general condition remains subjectively satisfactory, but 10-15% of patients experience itching. In the presence of a large number of mast cell foci, itching can be painful and difficult to treat.
Mastocytosis in children initially manifests as blisters accompanied by itching, and blisters often appear in newborns. Elements of the rash can be localized on any part of the body, but more often - in the area of the scalp, face, torso, and on the mucous membrane of the oral cavity. The palmar and plantar surfaces are free from rashes. Bubbles and blisters can occur against visually healthy skin or on swollen pink-red papules and spots. After the blisters resolve, persistent hyperpigmented brownish-brown spots remain, and papules may appear against them.
Mastocytosis spots have a characteristic round or oval shape, with clear outlines and a smooth surface without peeling. They do not rise above the surface of the skin and have a diameter from 2 mm to 50 mm. The spots tend to merge, resulting in the formation of large lesions with scalloped outlines, which in a child can cover the entire body. The rash periodically disappears and reappears. During subsequent attacks, its color becomes more intense, almost brown.
After exposure to sunlight, heat, especially after taking a hot bath or shower, in areas of physical impact (pressure, friction, injection), the redness of the rash elements within the boundaries of exposure becomes so intense that their basic brown-brown color becomes invisible, and in children even vesicles appear. Severe swelling and moderate or painful itching also occur. This phenomenon, induced artificially, is called the Unna-Darye phenomenon, or “ignition phenomenon.”
Stabilization stage
This stage of mastocytosis is characterized by the cessation of the appearance of fresh elements. It occurs in the second year of a child’s life or a little later.
Regression stage
Occurs 5-6 years after the onset of mastocytosis or during puberty. This stage is characterized by the disappearance of exudative manifestations of mastocytosis, gradual blanching and resolution of the rash elements.
Manifestations of urticaria pigmentosa: 1. in children; 2. in adults
Knotty shape
It usually affects children in the first two years of life, especially during the neonatal period. There are 3 clinical types of nodular mastocytosis:
- Xanthelomatous, which manifests itself as flat, isolated grouped nodules or nodular elements up to 15 mm in diameter. They have a dense consistency, clear boundaries, yellowish-brown or light yellow color, oval shape and a smooth or orange-peel surface. Individual elements resemble a pigmented nevus in their size and dark brown color.
- Multinodular, represented by hemispherical rashes of pink, red or yellowish color and with a diameter of 5-10 mm, “scattered” over all skin integuments. They have a smooth surface and dense consistency.
- Nodular-confluent, differing from the previous one by the fusion of elements with the formation of large foci, especially in the folds of the skin of the axillary, inguinal and intergluteal areas.
Blisters and blisters may appear on the elements and on visually healthy areas of the skin, and when they resolve, erosions and crusts form. Regardless of these varieties, the phenomenon of “inflammation” is insignificant, and in infants and young children it is completely absent.
All children under 2 years of age with any type of nodular form of mastocytosis periodically experience attacks of local (around the rash) or generalized skin redness as a manifestation of an anaphylactic reaction (histamine shock) in response to excess histamine in the blood. Such attacks can occur spontaneously or under the influence of crying, mechanical, thermal and other stimuli. In these cases, the itching intensifies, swelling and redness of the skin occurs, the child becomes restless, headaches, tearfulness and irritability, and rapid heartbeat. Gastrointestinal disorders are also possible: pain in the stomach, bloating, lack of appetite, nausea and vomiting, diarrhea.
Bullous mastocytosis
It is more often found in combination with nodular forms and less often with pigmented forms, and as an independent form - mainly in newborns and children under 2 years of age. It manifests itself as tense blisters with a diameter of up to 20 mm or more with serous or (less often) hemorrhagic contents. Usually they are located under the epidermis, sometimes inside it and deeper. At their bottom there are infiltrates consisting of mast cells. The blisters persist for several days, and after they resolve, a persistent patch of hyperpigmentation often remains.
Mastocytoma
As a rule, it occurs in children in the first 3 months of life, and sometimes from birth to 2 years of age. Among all cases of cutaneous mastocytosis in children, mastocytoma accounts for 10 to 25%.
It is a single (rarely up to 3-4 elements) skin tumor-like formation with clear boundaries and an orange-peel-shaped surface. The color of mastocytoma can be pink, red, orange, brownish or brownish-yellowish, diameter - 2-6 cm, usual localization - cervical region, shoulder girdle, limbs, sometimes - lungs, spleen, bones. As a rule, education is resolved independently.
Mastocytoma
Diffuse mastocytosis
Can affect both children and adults. This type of mastocytosis manifests itself as large dense foci with clear boundaries and irregular outlines. The lesions are yellowish-brown in color and are localized in the axillary and groin areas, in the intergluteal folds of the skin and cause severe, sometimes painful itching. If they progress, they spread to large areas of the skin. The surface of the lesions is often covered with ulcerations, cracks and scratch marks; blisters appear with minor trauma.
Persistent macular telangiectasia
It is a rare form of mastocytosis, occurs only in adults and is much more often, compared to other forms, accompanied by histamine shock. The rashes are abundant, localized mainly on the torso, upper and lower extremities. Telangiectasias appear on the surface of hyperpigmented elements.
1. Diffuse mastocytosis 2. Persistent macular telangiectasia
Systemic mastocytosis
Another name for cutaneous visceral mastocytosis is almost never found among young children. Damage to internal organs in combination with skin symptoms is typical.
Skin symptoms - itching, sudden redness and swelling of the skin, blistering rashes. Less common are limited rashes in the form of yellowish nodules in the area of natural skin folds, the skin becomes thickened and acquires a yellowish color.
The systemic nature of mastocytosis manifests itself only in adults in the form of weight loss, fever, profuse sweats, headaches, nosebleeds, rapid heartbeat, high blood pressure, etc. The digestive system is often affected, which is accompanied (in 25%) by pain, nausea, vomiting and intermittent diarrhea, as well as (in 10%) the formation of ulcers of the stomach, duodenum, enlargement of the liver and spleen.
A malignant type of systemic mastocytosis is mast cell leukemia, which occurs with damage to the skin (not always), the skeletal system and internal organs. Malignant blood pathology, amyloidosis and multiple organ failure develop very quickly, quickly leading to death.
Watch a video about urticaria pigmentosa:
Signs and symptoms
A solitary mastocytoma may not cause symptoms.
The spots and bumps may be itchy, especially if you rub or scratch them. Itching may worsen if:
- temperature changes;
- contact with clothing or other materials;
- the use of certain medications, including non-steroidal anti-inflammatory drugs (NSAIDs);
- consuming hot drinks, spicy foods or alcohol;
- physical activity.
If the spots are rubbed or scratched, they may develop into hives and the skin may become red.
Hyperemia often occurs.
Peptic ulcers can develop because too much histamine is produced, stimulating the secretion of stomach acid in excess. Peptic ulcers can cause stomach pain. Nausea, vomiting and chronic diarrhea may also occur. The abdomen may become enlarged if the liver and spleen are not functioning properly, causing fluid to accumulate in the abdominal cavity.
If the bone marrow is affected, bone pain may occur.
People with mastocytosis may become irritable, depressed, or moody.
Extensive reactions may occur. With systemic mastocytosis, extensive reactions are usually severe. These include anaphylactic and anaphylactoid reactions, which cause fainting and a life-threatening drop in blood pressure (shock). Anaphylactoid reactions resemble anaphylaxis, but they are not caused by an allergen.
Causes and risk factors
Genetic changes (mutations) resulting in excessive activation of the mast cell growth factor receptor (KIT) have been identified in abnormal mast cells in almost all adults with mastocytosis and in approximately 80% of children with skin lesions. The most common c-kit mutation in mastocytosis is D816V and is thought to cause abnormal proliferation and accumulation of mast cells in tissues. Approximately >90% of adults and 40% of children are also affected by this mutation, while an additional 40% of children have mutations in other KIT regions. The prognostic significance of the type of mutation in childhood disease has not yet been determined. Mutations are somatic in nature and therefore are not transmitted to the next generation in most patients.
The release of mediators produced by mast cells, such as histamine, heparin, chemokines, cytokines, leukotrienes, and prostaglandin D2, among other cellular mediators, leads to symptomatic episodes. Histamine is a naturally occurring chemical released during an allergic reaction, causing itching, shortness of breath, dilation of blood vessels and hypersecretion of stomach acid.
Causes
Since the specific causes of mastocytosis have not been established, it is considered in various pathological conditions. Most authors are inclined to consider it a systemic disease of the reticulohistiocytic system.
The assumption of the role of genetic factors is based on the presence of very rare cases of familial disease, especially among identical twins. In these cases, both autosomal recessive and autosomal dominant types of inheritance with different frequencies of pathology cannot be excluded.
The development of mastocystosis is also possible as a result of mutation of various genes, spontaneous cell proliferation caused by the cytokine system. A connection between the disease and hematopoietic disorders is also assumed. Therefore, other authors consider it in the group of malignant diseases of lymphoid and hematopoietic tissues.
Provoking factors may be immune factors associated with the presence of glycoprotein receptors in mast cells that are highly sensitive to class “E” immunoglobulins (IgE). Risk factors may also include non-immune factors such as:
- physical - friction over large areas of skin;
- cold and heat;
- contact with water;
- venom of bees and snakes, insect bites, stinging jellyfish;
- alcoholic drinks and drugs;
- toxins of bacteria and viruses;
- food products - cheeses, smoked meats, spices, citrus fruits, etc.;
- medications - acetylsalicylic acid, non-steroidal anti-inflammatory drugs containing codeine, B vitamins, morphine, iodide X-ray contrast agents, local anesthetics and some other anesthetic agents.
Disorders with similar symptoms
Symptoms of the following disorders may be similar to those of mastocytosis. Comparison may be useful for differential diagnosis:
- Inflammatory bowel disease (IBD) is associated with an abnormal immune response to naturally occurring bacteria in the gastrointestinal tract. Patients may experience weight loss, abdominal cramps and pain, nausea and vomiting, fatigue, and irregular bowel movements. Diagnosis of inflammatory bowel disease is often based on symptoms, which may include a fast heartbeat (tachycardia) and a low number of red blood cells (anemia), which leads to fatigue, dehydration and fever. There are various tests and imaging studies that may be performed to confirm the diagnosis and may include: complete blood count, serologic studies, stool studies, nutritional assessment, colonoscopy, abdominal ultrasound, and other gastrointestinal imaging studies.
- Irritable bowel syndrome (IBS) is a gastrointestinal disorder associated with abdominal discomfort, altered intestinal structures, and, in some cases, inflammation of the gastrointestinal tract. Patients with IBS may experience heartburn, nausea and vomiting, clear or white mucus, abdominal pain, and constipation or diarrhea. Patients may also experience abdominal bloating, which can be confirmed by a CT scan of the abdomen. There are specific criteria for diagnosing IBS based on the frequency and duration of symptoms of the disorder. The diagnostic criteria for IBS require that patients have had recurrent abdominal pain or discomfort on at least three days per month during the past three months, associated with two or more of the following conditions: relief with bowel movements; onset associated with changes in stool frequency; and/or onset associated with a change in the shape or appearance of the stool. To make a diagnosis of IBS, a physical examination, laboratory tests, and x-rays may be performed to rule out any other causes.
- Intestinal malabsorption includes Patients may experience diarrhea and weight loss; However, more characteristic symptoms are often based on a specific cause. Various tests may be performed to identify the cause and may include blood tests, electrolyte and chemical panel tests, and serological testing. Treatment of malabsorption consists of correcting any nutritional deficiencies as well as treating the underlying condition.
- Myeloproliferative diseases are a group of disorders associated with the proliferation of one or more distinct cell lineages. Patients may experience fatigue, weight loss, abdominal discomfort, easy bruising or bleeding, infections, and other symptoms. Specific diagnosis may be based on laboratory tests (ie, complete blood counts, leukocyte alkaline phosphatase, polymerase chain reaction, serum uric acid levels, red blood cell mass) and bone marrow biopsies, which would reflect changes in blood cell counts. Treatment for myeloproliferative disease depends on the specific cause. Patients with chronic myelogenous leukemia can be treated with a number of chemotherapy agents. In comparison, treatment is focused on maintenance therapy for patients with polycythemia vera, essential thrombocythemia, and myelofibrosis.
- Urticarial rash (hives) is a skin condition associated with the appearance of red, raised patches on the skin that can be itchy and irritating when touched. Urticaria is often an isolated phenomenon not associated with other systemic symptoms or signs. Often urticaria is self-limiting and short-lived. Skin lesions may last from 20 minutes to three hours and then disappear within 24 to 48 hours. New-onset urticaria is often associated with an identifiable cause, such as direct contact, and can be identified from the patient's history. Urticaria can often be confused with other skin diseases. However, based on the characteristic appearance of hives (i.e., itchy red lesions on the skin), a diagnosis can be made. Treatment for hives often involves the use of antihistamines.
- Endocrine tumors such as carcinoid, pheocromocytoma, and medullary thyroid cancer can cause flushing. Hot flashes after menopause are usually short-lived and associated with sweating.
- Monoclonal mast cell activation syndrome. These patients have symptoms of mast cell activation, including recurrent anaphylaxis, but no evidence of cutaneous mastocytosis. Their bone marrow biopsy shows 1 or 2 minor criteria for systemic mastocytosis, but does not meet the full World Health Organization (WHO) criteria.
- Idiopathic mast cell activation syndrome. Patients with this disorder have episodic symptoms of systemic mast cell activation associated with elevated mast cell mediators such as tryptase and histamine or prostaglandin metabolites in the urine, respond favorably to treatment with mast cell mediator blocking drugs, and do not have diagnostic signs of cutaneous or systemic mastocytosis. Other disorders with similar symptoms, such as allergic diseases, must be excluded before this diagnosis is considered.
Diagnosis of mastocytosis and its treatment
Diagnosis of cutaneous mastocytosis includes a history and physical examination, and laboratory tests to see if there is damage to other organs.
Diagnosis of mastocytosis may include the following:
- physical examination for rashes, enlarged lymph nodes, enlarged liver and spleen;
- detailed clinical blood test;
- skin biopsy if necessary;
- It is possible to prescribe an abdominal ultrasound or CT scan.
As a rule, children with cutaneous mastocytosis have a favorable prognosis if it appears in the first 2 years of life, because spontaneous resolution of the disease occurs most often in this age group after several years, before puberty.
Manifestations on the skin begin to disappear after the child is 5-6 years old, the average duration of the disease is 10 years.
Mastocytomas can go away on their own after a few years.
If cutaneous mastocytosis develops after 2 years of age or older, as well as in adulthood, it usually persists. Despite this, in more than 80% of children with cutaneous mastocytosis, the disease resolves on its own.
The treatment of cutaneous mastocytosis is carried out by a pediatrician, if necessary, involving more specialized specialists: a dermatologist, hematologist, allergist and others.
Diagnostics
Diagnostics include:
- medical examination;
- biopsy;
- blood tests to rule out other diseases.
Doctors suspect mastocytosis based on symptoms, especially if there are patches that turn into hives and redness when scratched.
A biopsy can confirm the diagnosis of mastocytosis. Typically, a sample of skin tissue is taken and examined under a microscope for the presence of mast cells. Sometimes the sample is taken from the bone marrow.
If the diagnosis is unclear, doctors may do the following:
- Blood and urine tests to measure levels of substances associated with mast cells. High levels of these substances confirm the diagnosis of systemic mastocytosis.
- Blood and urine tests to rule out diseases that cause similar symptoms.
- Bone scan.
- Tests for a genetic mutation present in many people with mastocytosis.
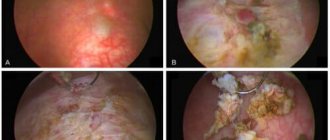
- A biopsy (using an endoscope) to determine if there are abnormally high numbers of mast cells in the digestive tract.
Diagnosis
The diagnosis is made on the basis of a wedge, a picture, a positive Unna symptom and is confirmed histologically (the presence of infiltrates from mast cells).
Differential diagnosis is carried out with nevus (see), leiomyoma (see), syringoma (see Skin, tumors), disseminated xanthoma (see), histiocytoma (see), lentigo (see), urticaria (see), acanthosis nigricans (see), elastic pseudoxanthoma (see elastic pseudoxanthoma), skin reticulosis (see), chronic myeloid leukemia.
Standard Treatments
Treatment includes:
- medications to reduce symptoms;
- for aggressive systemic mastocytosis, other drugs such as interferon or surgery such as splenectomy.
A single mastocytoma may disappear spontaneously.
Itching caused by cutaneous mastocytosis can be treated with antihistamines. For children, no other treatment is required. If adults experience itching and rashes, psoralen (a drug that makes the skin more sensitive to ultraviolet radiation) may be applied to the skin, ultraviolet light, or corticosteroid creams may be used.
Systemic mastocytosis cannot be completely cured, but symptoms can be suppressed with H1 and H2 blockers. H1 blockers (commonly called antihistamines) may relieve itching. H2 blockers reduce the production of acid in the stomach and thus relieve the symptoms of peptic ulcers and help treat the ulcer. Taking cromolyn orally can relieve digestive problems and bone pain. Aspirin relieves flushing but may worsen other symptoms. Children are not given aspirin due to the risk of Reye's syndrome.
Mechanism of disease development
Mast cells (mast cells) are a subtype of leukocytes. In a mature state, they are localized in the connective tissue structures of the body. Mast cells play an important role in the development of inflammation, allergies, and anaphylactic reactions. In addition, they participate in tissue healing and the formation of new blood vessels in places where they are damaged.
The cytoplasm of cells contains a large number of granules with inflammatory mediators - histamine, heparin, cytokines. When released into the surrounding tissues and bloodstream, the substances provoke an increase in vascular permeability. The consequence of this is the development of local edema, increased temperature, and redness. Irritation of sensitive nerve endings causes itching and pain. Activated mast cells on the skin appear as red, swollen spots similar to a mosquito bite.
Forecast
The prognosis depends on the age of onset. Most patients with urticaria pigmentosa present with disease onset before age 2 years, which is associated with an excellent prognosis, often with resolution at puberty. The number of lesions decreases by approximately 10% per year. However, acute widespread degranulation may rarely cause life-threatening episodes of shock.
The onset of cutaneous mastocytosis after age 10 years predicts a worse prognosis because late-onset disease tends to be persistent, is more often associated with systemic disease, and carries a higher risk of malignant transformation.